Provide appropriate tetanus prophylaxis (see Appendix H), and check for associated injuries, such as loose teeth and mandibular or facial fractures. Crushed ice wrapped in clean gauze and held inside the cheek may help limit swelling, bleeding, and discomfort.
 If dental fractures or avulsions are present, explore wounds thoroughly with your gloved finger, looking for a dental fragment within the wound. In deep wounds or whenever there is the question of a retained foreign body, obtain radiographs or perform ultrasonography (using a 6.5-MHz endocavity transducer) to rule it in or out. Ideally, all missing teeth or dental fragments should be accounted for (see Chapter 42).
If dental fractures or avulsions are present, explore wounds thoroughly with your gloved finger, looking for a dental fragment within the wound. In deep wounds or whenever there is the question of a retained foreign body, obtain radiographs or perform ultrasonography (using a 6.5-MHz endocavity transducer) to rule it in or out. Ideally, all missing teeth or dental fragments should be accounted for (see Chapter 42).
 When only small lacerations (less than 2 cm) are present and only minimal gaping of the wound occurs, reassurance and simple aftercare are all that is required. Inform the patient that the wound will become somewhat uncomfortable and covered with pus over the next 48 hours, and instruct him to rinse with lukewarm water or half-strength hydrogen peroxide for several days after meals and every 1 to 2 hours while awake. Patients may rinse with chlorhexidine 0.12% oral rinse, swished in mouth for 30 seconds and spit out four times daily.
When only small lacerations (less than 2 cm) are present and only minimal gaping of the wound occurs, reassurance and simple aftercare are all that is required. Inform the patient that the wound will become somewhat uncomfortable and covered with pus over the next 48 hours, and instruct him to rinse with lukewarm water or half-strength hydrogen peroxide for several days after meals and every 1 to 2 hours while awake. Patients may rinse with chlorhexidine 0.12% oral rinse, swished in mouth for 30 seconds and spit out four times daily.
 If there is continued bleeding or the wound edges fall between chewing surfaces, or if the wound edges gape significantly (especially on the edge of the tongue), or there is a flap or deformity when the underlying musculature contracts, the wound should be anesthetized using lidocaine with epinephrine, cleansed thoroughly with saline, and loosely approximated using a 5-0 or 6-0 absorbable suture.
If there is continued bleeding or the wound edges fall between chewing surfaces, or if the wound edges gape significantly (especially on the edge of the tongue), or there is a flap or deformity when the underlying musculature contracts, the wound should be anesthetized using lidocaine with epinephrine, cleansed thoroughly with saline, and loosely approximated using a 5-0 or 6-0 absorbable suture.
 Most tongue lacerations heal well without suturing. The decision of whether or not to repair tongue lacerations depends on the estimated risk of compromised function after healing. Lacerations that should be considered for repair include large lacerations (greater than 1 cm in length) that extend into or pass through the muscular layers of the tongue, deep lacerations on the lateral border of the tongue, gaping lacerations or those with large flaps, or lacerations that may cause dysfunction if healed improperly (anterior split tongue). Tongue lacerations that do not need repair include those less than 1 cm in length, nongaping lacerations, or lacerations assessed to be clinically minor.
Most tongue lacerations heal well without suturing. The decision of whether or not to repair tongue lacerations depends on the estimated risk of compromised function after healing. Lacerations that should be considered for repair include large lacerations (greater than 1 cm in length) that extend into or pass through the muscular layers of the tongue, deep lacerations on the lateral border of the tongue, gaping lacerations or those with large flaps, or lacerations that may cause dysfunction if healed improperly (anterior split tongue). Tongue lacerations that do not need repair include those less than 1 cm in length, nongaping lacerations, or lacerations assessed to be clinically minor.

 Consider using procedural sedation and analgesia when suturing children who cannot cooperate (see Appendix E).
Consider using procedural sedation and analgesia when suturing children who cannot cooperate (see Appendix E).
 A traction stitch or special rubber-tipped clamp can be very helpful when attempting to suture the tongue of a small child or an intoxicated adult (Figure 51-1). The same aftercare as described earlier applies here as well.
A traction stitch or special rubber-tipped clamp can be very helpful when attempting to suture the tongue of a small child or an intoxicated adult (Figure 51-1). The same aftercare as described earlier applies here as well.
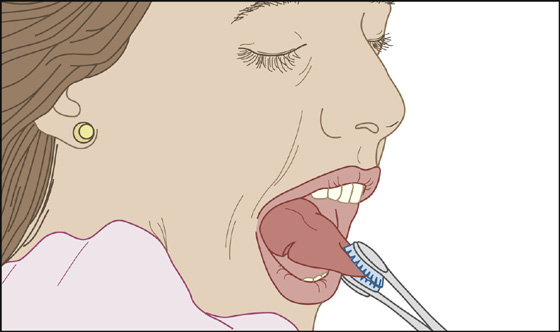
Figure 51-1 Proper use of a rubber-tipped clamp.
 When the exterior surface of the lip is lacerated, any separation of the underlying musculature must be repaired with buried absorbable sutures.
When the exterior surface of the lip is lacerated, any separation of the underlying musculature must be repaired with buried absorbable sutures.
 To avoid an unsightly scar when the lip heals, precise skin approximation is very important. First, approximate the vermilion border, making this the key suture (Figure 51-2). Fine nonabsorbable suture material (e.g., 6-0 nylon or Prolene) is most appropriate for the skin surfaces of the lip, whereas a fine absorbable suture (e.g., 6-0 Dexon or Vicryl) is quite acceptable for use on the mucosa and vermilion.
To avoid an unsightly scar when the lip heals, precise skin approximation is very important. First, approximate the vermilion border, making this the key suture (Figure 51-2). Fine nonabsorbable suture material (e.g., 6-0 nylon or Prolene) is most appropriate for the skin surfaces of the lip, whereas a fine absorbable suture (e.g., 6-0 Dexon or Vicryl) is quite acceptable for use on the mucosa and vermilion.
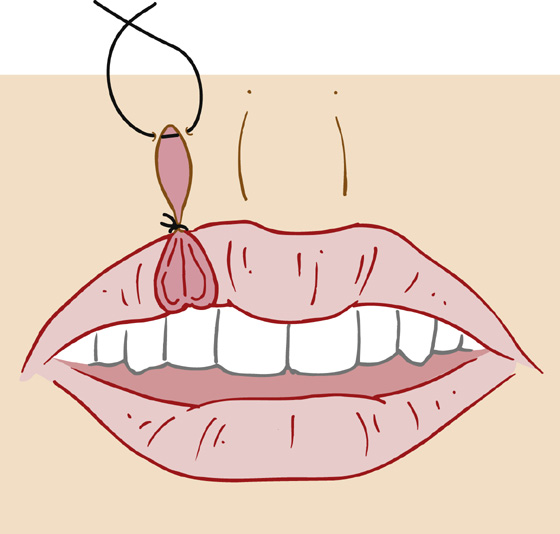
Figure 51-2 In the repair of lip lacerations, the first stitch should be placed at the vermilion-cutaneous border to obtain proper alignment. (From Grabb WC, Kleinert HE: Techniques in surgery: facial and hand injuries. Somerville, NJ, 1980, Ethicon, Inc.)
 Although in most cases antibiotics are not indicated, for deep lacerations of the mucosa or lip or for any sutured laceration in the mouth, it is reasonable to prescribe prophylactic penicillin (penicillin V potassium, 500 mg tid for 3 to 4 days) to prevent deep tissue infections. (Erythromycin or azithromycin may be substituted in penicillin-allergic individuals.)
Although in most cases antibiotics are not indicated, for deep lacerations of the mucosa or lip or for any sutured laceration in the mouth, it is reasonable to prescribe prophylactic penicillin (penicillin V potassium, 500 mg tid for 3 to 4 days) to prevent deep tissue infections. (Erythromycin or azithromycin may be substituted in penicillin-allergic individuals.)
 Recommend acetaminophen or ibuprofen for pain.
Recommend acetaminophen or ibuprofen for pain.
 Instruct patient to return in 48 hours for a wound reevaluation.
Instruct patient to return in 48 hours for a wound reevaluation.
 Recommend that the patient consume only cool liquids and soft foods beginning 4 hours after the repair.
Recommend that the patient consume only cool liquids and soft foods beginning 4 hours after the repair.
What Not To Do:
 Do not bother to repair a simple laceration or avulsion of the frenulum of the upper lip. It will heal quite nicely on its own (Figure 51-3).
Do not bother to repair a simple laceration or avulsion of the frenulum of the upper lip. It will heal quite nicely on its own (Figure 51-3).
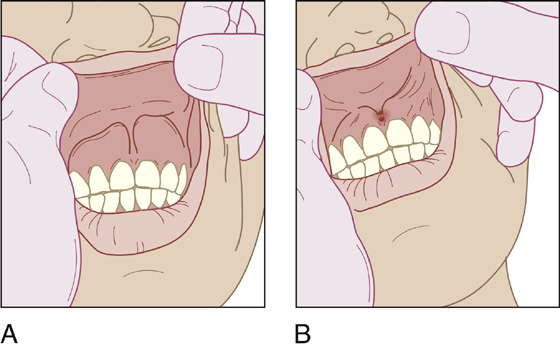
Figure 51-3 Simple laceration or avulsion of the frenulum of the upper lip. A, Normal frenulum. B, Lacerated frenulum.
 Do not use nonabsorbable suture material on the tongue, gingiva, or buccal mucosa. There is no advantage, and suture removal on a small child will be an unpleasant struggle at best.
Do not use nonabsorbable suture material on the tongue, gingiva, or buccal mucosa. There is no advantage, and suture removal on a small child will be an unpleasant struggle at best.
 Do not overlook domestic abuse or child abuse.
Do not overlook domestic abuse or child abuse.
Imprecise repair of the vermilion border will lead to a “step-off” or puckering that is unsightly and difficult to repair later.
Fortunately, the tongue and oral mucosa usually heal with few complicating infections, and there is a low risk for subsequent tissue necrosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



