CHAPTER 149
Paronychia
Presentation
The patient presents with finger or toe pain that has developed rapidly, either over the past several hours or over a few days. This pain is accompanied by a very red, tender swelling of the nail fold, or this swelling may be less red and tender and appear chronic in nature. There are three distinct varieties.
• Acute paronychia almost always involves fingers and usually quickly becomes very painful. It is caused by the introduction of pyogenic bacteria, either spontaneously or as a result of minor trauma, and results in acute inflammation and abscess formation within the thin subcutaneous layer between the skin of the eponychial fold and the germinal layer of the eponychial cul-de-sac (Figure 149-1, A). In its earliest form, there may only be cellulitis with no collection of pus. Fluctuance that may be difficult to detect, along with local purulence at the nail margin, may occur, and infection may extend beneath the nail margin to involve the nail bed.
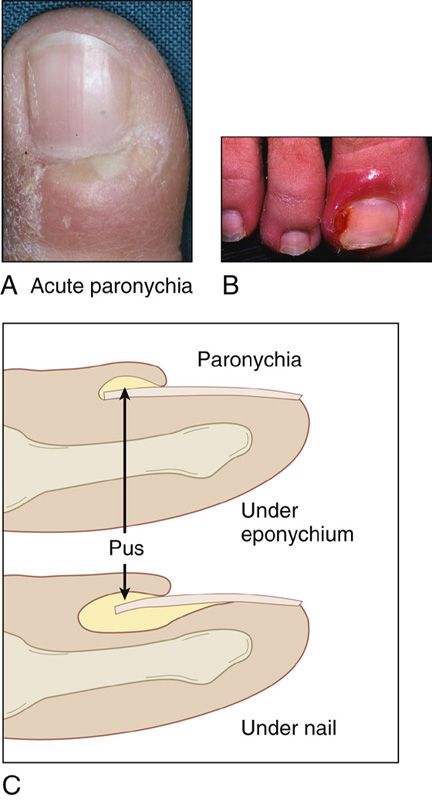
Figure 149-1 A, Acute paronychia of finger with red, hot, tender nail fold showing pus beneath the cuticle. B, Chronic paronychia with an ingrown toenail. C, Subungual extension of pus.
• Chronic paronychia (Figure 149-1, B) is most commonly seen with an ingrown toenail, with chronic inflammation, thickening and purulence of the eponychial fold, and loss of the cuticle. The toenail edge may be embedded in the lateral nail fold. There may or may not be granulation tissue. This also occurs with individuals whose hands are frequently exposed to moisture and minor trauma.
• The third variety of paronychia is a subungual abscess, which occurs in the same location as a subungual hematoma and presents with pain and entrapped pus that is visible between the nail plate and the nail bed (Figure 149-1, C).
What To Do:
Acute Paronychia

 When there is minimal swelling and there appears to be only cellulitis, gently slide an 18-gauge needle parallel to and along the surface of the nail plate (with the bevel up) to separate and lift up the cuticle of the swollen lateral nail fold from the nail. Alternatively, use a large-gauge needle with the bevel down to elevate the lateral nail fold. When this separation or puncture of the cuticle occurs, pus will often unexpectedly drain from the eponychial cul-de-sac. (Digital block anesthesia may not be required, because you are only puncturing or separating epithelial cuticular tissue.) Instruct the patient to then soak the finger in warm antibacterial soap and water for 10 to 15 minutes at least four times per day. The patient can remain quite mobile if he uses a disposable cup to soak his finger while performing his daily routine.
When there is minimal swelling and there appears to be only cellulitis, gently slide an 18-gauge needle parallel to and along the surface of the nail plate (with the bevel up) to separate and lift up the cuticle of the swollen lateral nail fold from the nail. Alternatively, use a large-gauge needle with the bevel down to elevate the lateral nail fold. When this separation or puncture of the cuticle occurs, pus will often unexpectedly drain from the eponychial cul-de-sac. (Digital block anesthesia may not be required, because you are only puncturing or separating epithelial cuticular tissue.) Instruct the patient to then soak the finger in warm antibacterial soap and water for 10 to 15 minutes at least four times per day. The patient can remain quite mobile if he uses a disposable cup to soak his finger while performing his daily routine.
 If no pus was obtained, provide close follow-up and consider prescribing an antibiotic:
If no pus was obtained, provide close follow-up and consider prescribing an antibiotic:
 In uncomplicated cases, without likely oral flora exposure: cephalexin 250 to 500 mg qid × 7 days or dicloxacillin 250 to 500 mg qid × 7 days.
In uncomplicated cases, without likely oral flora exposure: cephalexin 250 to 500 mg qid × 7 days or dicloxacillin 250 to 500 mg qid × 7 days.
 In cases involving more significant disease, or immunosuppression: amoxicillin/clavulanate (Augmentin), 875 mg/125 mg bid or clindamycin (Cleocin), 300 mg qid × 7 days.
In cases involving more significant disease, or immunosuppression: amoxicillin/clavulanate (Augmentin), 875 mg/125 mg bid or clindamycin (Cleocin), 300 mg qid × 7 days.
 In cases with suspected community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA): trimethoprim-sulfamethoxazole, 1 to 2 double-strength tablet(s) bid × 7 days or clindamycin (Cleocin), 300 mg qid × 7 days.
In cases with suspected community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA): trimethoprim-sulfamethoxazole, 1 to 2 double-strength tablet(s) bid × 7 days or clindamycin (Cleocin), 300 mg qid × 7 days.
 When there is significant pain and swelling of the nail fold (there may or may not be a visible overlying pustule), consider performing a digital block to prevent potential manipulative discomfort (see Appendix B). Then, as above, slide an 18-gauge needle or a No. 15 scalpel blade along the surface of the nail plate (keep the blade flat against the nail) under the nail fold, separating or incising the cuticle and thereby opening the eponychial cul-de-sac and draining the pus (Figure 149-2, A).
When there is significant pain and swelling of the nail fold (there may or may not be a visible overlying pustule), consider performing a digital block to prevent potential manipulative discomfort (see Appendix B). Then, as above, slide an 18-gauge needle or a No. 15 scalpel blade along the surface of the nail plate (keep the blade flat against the nail) under the nail fold, separating or incising the cuticle and thereby opening the eponychial cul-de-sac and draining the pus (Figure 149-2, A).
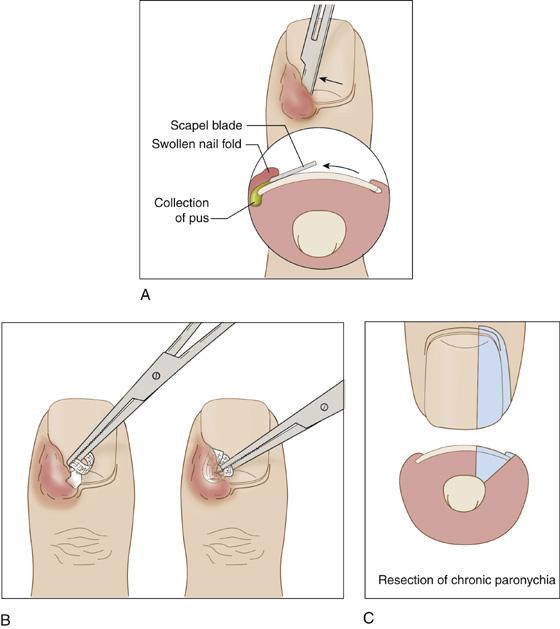
Figure 149-2 A, Draining acute paronychia without invasion of skin. B, A gauze wick may help to ensure continued drainage. C, Extensive excision of chronic paronychia.
 There should be no deliberate invasion into the dermis (although there may be an inadvertent stick); therefore it may still be unnecessary to perform a digital block.
There should be no deliberate invasion into the dermis (although there may be an inadvertent stick); therefore it may still be unnecessary to perform a digital block.
 Although not necessary, a tiny wick (1 cm of ¼-inch plain gauze or a thin strip of nonadherent dressing) may be slid into the opening to help promote continued drainage (Figure 149-2, B).
Although not necessary, a tiny wick (1 cm of ¼-inch plain gauze or a thin strip of nonadherent dressing) may be slid into the opening to help promote continued drainage (Figure 149-2, B).
 Unroof and débride any periungual pustule.
Unroof and débride any periungual pustule.
 Most important, instruct the patient (as described above) to perform warm soaks for 10 to 15 minutes at least qid for 1 to 2 days. He may apply ointment covered by a simple bandage between soaks.
Most important, instruct the patient (as described above) to perform warm soaks for 10 to 15 minutes at least qid for 1 to 2 days. He may apply ointment covered by a simple bandage between soaks.
 When drainage has been provided, antibiotics are not routinely required, and cultures will not benefit the patient or change management, with several notable exceptions. Exceptions include marked cellulitis, a condition of immunosuppression, possible CA-MRSA, and suspicion of unusual infections (Pseudomonas spp., fungal infections). In these special cases, prescribe antibiotics as discussed above. Follow-up should be provided within 2 to 3 days.
When drainage has been provided, antibiotics are not routinely required, and cultures will not benefit the patient or change management, with several notable exceptions. Exceptions include marked cellulitis, a condition of immunosuppression, possible CA-MRSA, and suspicion of unusual infections (Pseudomonas spp., fungal infections). In these special cases, prescribe antibiotics as discussed above. Follow-up should be provided within 2 to 3 days.
Chronic Paronychia
 When symptoms and findings are minimal, consider conservative treatment or temporizing the condition by sliding a cotton wedge or waxed dental floss under the corner of an ingrown nail to lift the nail edge from its embedded position. (Anesthesia is usually not required.) Instruct the patient to use warm soaks at least four times per day. When candidiasis is suspected, the area should be kept dry and treated with local applications of nystatin or a topical antifungal medication combined with a topical steroid (e.g., betamethasone 0.05% + clotrimazole 1% [Lotrisone] cream).
When symptoms and findings are minimal, consider conservative treatment or temporizing the condition by sliding a cotton wedge or waxed dental floss under the corner of an ingrown nail to lift the nail edge from its embedded position. (Anesthesia is usually not required.) Instruct the patient to use warm soaks at least four times per day. When candidiasis is suspected, the area should be kept dry and treated with local applications of nystatin or a topical antifungal medication combined with a topical steroid (e.g., betamethasone 0.05% + clotrimazole 1% [Lotrisone] cream).
 Follow-up with a podiatrist is important for ingrown toenails. Instruct the patient to cut toenails straight across to prevent recurrences. Recommend loose-fitting stockings and shoes with a roomy toe box. Also, instruct the patient to decrease activities such as running or other sports that put pressure on the toes. Inform him that it may take 3 months for an embedded toenail to grow beyond the lateral nail fold and that a cotton wedge must be repeatedly replaced until this occurs.
Follow-up with a podiatrist is important for ingrown toenails. Instruct the patient to cut toenails straight across to prevent recurrences. Recommend loose-fitting stockings and shoes with a roomy toe box. Also, instruct the patient to decrease activities such as running or other sports that put pressure on the toes. Inform him that it may take 3 months for an embedded toenail to grow beyond the lateral nail fold and that a cotton wedge must be repeatedly replaced until this occurs.
 When symptoms and findings are more extensive, a more aggressive approach—and one more likely to be successful—that requires a unilateral or bilateral digital block (see Appendix B) and a bloodless field (use a rubber tourniquet) is to sharply excise the affected portion of the nail, nail bed, and matrix down to the periosteum of the distal phalanx (Figure 149-2, C). First cleanse the toe with an iodine-povidone solution, and then elevate the outer edge of the nail plate by inserting a fine straight hemostat under the nail. Excise approximately one quarter to one third of the nail plate with strong fine scissors to make a longitudinal cut; then pull it out from under the eponychium with the hemostat (Figure 149-3).
When symptoms and findings are more extensive, a more aggressive approach—and one more likely to be successful—that requires a unilateral or bilateral digital block (see Appendix B) and a bloodless field (use a rubber tourniquet) is to sharply excise the affected portion of the nail, nail bed, and matrix down to the periosteum of the distal phalanx (Figure 149-2, C). First cleanse the toe with an iodine-povidone solution, and then elevate the outer edge of the nail plate by inserting a fine straight hemostat under the nail. Excise approximately one quarter to one third of the nail plate with strong fine scissors to make a longitudinal cut; then pull it out from under the eponychium with the hemostat (Figure 149-3).
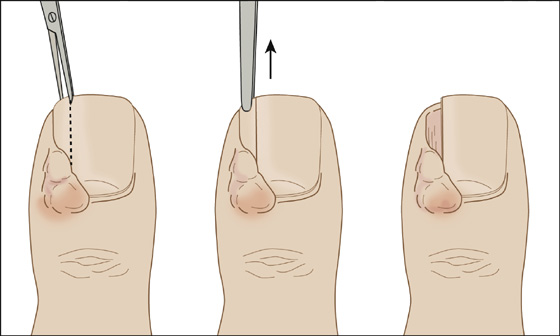
Figure 149-3 For more severe acute and chronic infections, removing a portion of the nail helps to prevent recurrence.
 When only a small amount of granulation tissue is present after the nail plate is excised, the nail bed may be left in place and only the granulation tissue excised. The remaining granulation tissue can be cauterized using silver nitrate. The patient is instructed to soak the toe in warm water for 20 minutes twice per day and arrange for multiple follow-up visits.
When only a small amount of granulation tissue is present after the nail plate is excised, the nail bed may be left in place and only the granulation tissue excised. The remaining granulation tissue can be cauterized using silver nitrate. The patient is instructed to soak the toe in warm water for 20 minutes twice per day and arrange for multiple follow-up visits.
Subungual Abscess (When Pus Is Visible beneath the Nail)
 Consider conservative treatment not requiring a digital block. Merely perform a trephination using the same “hot paper clip” technique used for a subungual hematoma (see Chapter 156). The patient must perform frequent warm soaks over the next 36 hours to prevent recurrence.
Consider conservative treatment not requiring a digital block. Merely perform a trephination using the same “hot paper clip” technique used for a subungual hematoma (see Chapter 156). The patient must perform frequent warm soaks over the next 36 hours to prevent recurrence.
 A more aggressive approach, requiring digital block, is to excise a portion of the nail. Unlike the more extensive procedure used with chronic paronychia, only a portion of the nail plate need be removed (see Figure 149-3). After performing a digital block, cleansing with iodine-povidone and performing a bloodless field, insert a fine straight hemostat between the nail and the nail bed, and push and spread until you enter the eponychial cul-de-sac. Often it is at this point that pus is discovered and released. Using a pair of strong fine scissors, cut away the one quarter to one third of the nail plate bordering the paronychia. Separate the cuticle using the hemostat, and pull this unwanted fragment away. A nonadherent dressing is required over the exposed nail bed, as well as an early dressing change (within 24 hours). Frequent soaks are also required. Inform the patient that extensive damage to the germinal matrix by the infection may preclude healthy nail regrowth.
A more aggressive approach, requiring digital block, is to excise a portion of the nail. Unlike the more extensive procedure used with chronic paronychia, only a portion of the nail plate need be removed (see Figure 149-3). After performing a digital block, cleansing with iodine-povidone and performing a bloodless field, insert a fine straight hemostat between the nail and the nail bed, and push and spread until you enter the eponychial cul-de-sac. Often it is at this point that pus is discovered and released. Using a pair of strong fine scissors, cut away the one quarter to one third of the nail plate bordering the paronychia. Separate the cuticle using the hemostat, and pull this unwanted fragment away. A nonadherent dressing is required over the exposed nail bed, as well as an early dressing change (within 24 hours). Frequent soaks are also required. Inform the patient that extensive damage to the germinal matrix by the infection may preclude healthy nail regrowth.
 When there is a distal collection of pus under the nail plate, a simple excision of an overlying wedge of nail using scissors should provide complete drainage.
When there is a distal collection of pus under the nail plate, a simple excision of an overlying wedge of nail using scissors should provide complete drainage.
What Not To Do:
 Do not order cultures or radiographs for uncomplicated cases. However, remember that CA-MRSA is increasingly prevalent and may affect antibiotic choice if antibiotic therapy is indicated.
Do not order cultures or radiographs for uncomplicated cases. However, remember that CA-MRSA is increasingly prevalent and may affect antibiotic choice if antibiotic therapy is indicated.
 Do not make an actual skin incision while treating acute paronychia. The cuticle needs only to be separated from the nail to release any collection of pus.
Do not make an actual skin incision while treating acute paronychia. The cuticle needs only to be separated from the nail to release any collection of pus.
 Do not remove an entire fingernail or toenail to drain simple paronychia. The patient will be left with a very sensitive exposed nail bed unnecessarily.
Do not remove an entire fingernail or toenail to drain simple paronychia. The patient will be left with a very sensitive exposed nail bed unnecessarily.
 Do not attempt to drain a herpetic whitlow. When coalescing vesicles with surrounding erythema are present, assume that the infection is caused by herpes simplex virus. Treatment involves inhibition of viral replication with acyclovir (Zovirax), valacyclovir (Valtrex), or famciclovir (Famvir) (see Chapter 54).
Do not attempt to drain a herpetic whitlow. When coalescing vesicles with surrounding erythema are present, assume that the infection is caused by herpes simplex virus. Treatment involves inhibition of viral replication with acyclovir (Zovirax), valacyclovir (Valtrex), or famciclovir (Famvir) (see Chapter 54).
 Do not confuse a felon (with a tense tender fingerpad) with a paronychia. Felons will require more extensive surgical treatment.
Do not confuse a felon (with a tense tender fingerpad) with a paronychia. Felons will require more extensive surgical treatment.
Discussion
Acute paronychia most commonly results from nail biting, finger sucking, aggressive manicuring, a hang nail, or penetrating trauma. Most infections are minor and can be treated easily with conservative methods. The more extensive the infection is, the more aggressive the surgical approach must be. Patients who have been adequately treated should be relatively asymptomatic within 3 to 5 days.
Ingrown toenails (onychocryptosis) occur most frequently in the early to midadolescent period. They tend to occur during periods of rapid foot growth when shoes get too tight. A precipitating event is usually cutting the nail at an angle to the sulcus. Subsequent growth causes a spicule of the nail, usually in the lateral sulcus, to penetrate the skin. This spicule introduces bacteria and infection into the surrounding tissue with formation of pus and granulation tissue.
Whenever conservative therapy is instituted, the patient should be advised of the advantages and disadvantages of that approach. If the patient is not willing or reliable enough to perform the required aftercare or cannot accept the potential treatment failure, it would seem prudent to begin with the more aggressive treatment modes.
No single antibiotic will provide complete coverage for the array of bacterial and fungal pathogens cultured from paronychias. In theory, amoxicillin/clavulanate clindamycin should be the most appropriate antibiotics, but because most paronychias are easily cured with simple drainage, systemic antibiotics are usually not indicated. In immunocompromised patients, those with peripheral vascular disease, and those in whom unusual pathogens are suspected, cultures and antibiotics are indeed warranted.
Remain alert to the possible complications of neglected paronychia, such as osteomyelitis, septic tenosynovitis of the flexor tendon, or a closed-space infection of the distal fingerpad (felon). Recurrent infections may be caused by a herpes simplex infection (herpetic whitlow) or fungus (onychomycosis). Tumors such as squamous cell carcinoma or melanoma, cysts, syphilitic chancres, warts, or foreign body granulomas can occasionally mimic paronychia.
Failure to cure paronychia within 4 or 5 days should prompt specialized culture techniques, biopsy, or referral.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


