Chapter 21 Intubating Introducers, Stylets, and Lighted Stylets (Lightwands)
I Introduction
The procedure of placing an endotracheal tube (ETT) in the trachea for ventilation and oxygenation is more than a thousand years old. It was first performed on pigs by the Persian physician, Avicenna, between 980 and 1037 AD.1,2 Blind digital intubation in humans was first described in 1796 by Herholdt and Rafn in a resuscitation protocol for drowning victims.3 In 1880, Macewen described blind digital intubation in awake patients using a curved metal tube.4 However, modern methods of laryngoscopic endotracheal intubation did not emerge until early in the 20th century, after the introduction of a flexible metal tube by Kuhn5 and of the laryngoscope by Jackson.6
Over the years, direct laryngoscopic intubation has been shown to be an effective, safe, and relatively easy technique. In fact, using a laryngoscope to obtain line of sight to the laryngeal inlet has become the standard method of endotracheal intubation in the operating room, the intensive care unit, and the emergency department. However, even in the hands of experienced laryngoscopists, accurate and prompt placement of the ETT remains a significant challenge in some patients. This is particularly true in “unprepared” patients and in patients requiring emergency intubation. With any standard laryngoscope, obtaining line of sight to the patient’s larynx can prove difficult in the presence of specific anatomic variations such as a receding mandible, prominent upper incisors, a restricted mouth opening, or limited movement of the cervical spine. It has been estimated that 1% to 3% of surgical patients have a so-called difficult airway (DA), making laryngoscopic intubation problematic and sometimes impossible.7 In the obstetric population, the incidence of failed laryngoscopic intubation has been reported to be 0.05% to 0.35%.8 Many predictors of difficult laryngoscopy (DL) have been suggested in the literature,9,10 but the sensitivity and specificity of these tests remain relatively low.11–13 Therefore, all clinicians must be prepared to deal with the prospect of both anticipated and unanticipated DLs.
II Intubating Introducers and Stylets
A History
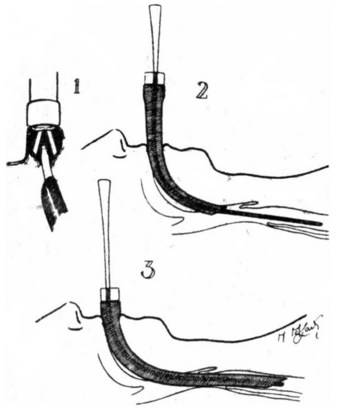
Intubating guides or introducers were first reported in the late 1940s. In 1949, Macintosh described “the use of a gum elastic introducer as an aid to passing endotracheal tubes” (Fig. 21-1) as follows14:
B The Eschmann Introducer
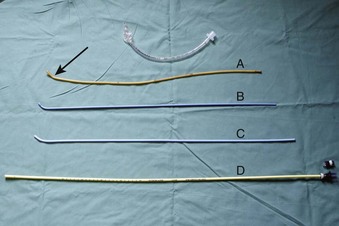
Use of an introducer in this fashion did not become widespread until the development of the Eschmann Introducer (EI) by Venn in 1973. Venn’s design has several key features. First, it is relatively long at 60 cm (Fig. 21-2), allowing one to place the introducer between the cords before “railroading” the ETT over its distal end. It has been suggested that a naked introducer affords better dexterity and tactile sensation to the user compared with an introducer on which an ETT has been preloaded.15 Second, the EI has a coudé tip (a 40-degree bend) for “hooking” under the epiglottis. The material from which the EI is made—a combination of a polyester core and resin covering—no doubt has contributed to its success.15 The EI is malleable, firm enough to direct, yet flexible enough to yield on contact. Furthermore, it is a multiuse device that can be sterilized between uses. The EI is commonly referred to as a “gum elastic bougie” despite not being made of gum, having no elastic properties, and not being a “bougie” at all (a bougie being a dilating device).16,17 The EI is currently sold under the name “Portex Venn Introducer” (Smiths Medical, UK.)
Although an EI can be used to direct the ETT toward an “anterior” or narrow larynx, its real strength lies as a tool to facilitate intubation when the laryngeal aperture cannot be seen during laryngoscopy (e.g., Cormack-Lehane grade 3 view).18 If the epiglottis cannot be visualized at all (i.e., Cormack-Lehane grade 4 view), we do not recommend use of the EI, because the likelihood of successful intubation with the EI is unacceptably low. In cases in which the epiglottis can be seen, the coudé tip can be hooked under the epiglottis and the EI advanced blindly through the glottis. The success of this maneuver is improved if the EI has been preshaped into a curve.19 As the introducer is advanced further, the tracheal “clicks” are felt approximately 90% of the time if the EI is correctly placed,20 whereas no “clicks” will be observed if the EI has been advanced into the esophagus. We believe that “clicks” are more likely to be perceived if, once the tip of the EI is through the cords, the introducer is advanced at a shallow angle relative to the patient. This maneuver is intended to ensure that the tip of the introducer will contact the cartilaginous rings on the anterior tracheal wall as it advances, producing the “clicking” sensation. One can imagine that “clicks” are less likely to be felt if the only contact between the trachea and the EI is the coudé bend in the introducer that is sliding along the posterior tracheal wall, or even along the trachealis muscle.
Additional clues to confirm correct tracheal placement include the perception that the EI slightly deviates to the right as it advances into the right main bronchus and a “hold up” felt at the 30- to 35-cm mark as the EI becomes lodged in a distal airway (reportedly a 100% reliable sign).20 In contrast, if the EI is placed in the esophagus, the entire EI could be advanced without encountering any resistance, although theoretically it would be possible for a pharyngeal pouch to hold up the introducer if one were present.21 Some authors have cautioned against the use of the hold-up sign, believing that it increases the risk of airway trauma. If clicks are felt, then the hold-up test is not required.20
After tracheal placement, the ETT is advanced distally over the EI into the trachea. A jaw lift-jaw thrust by the nondominant hand of the clinician or by a laryngoscope will facilitate the advancement of the ETT over the EI by elevating the tongue and epiglottis. If difficulty persists while the ETT is being advanced, rotating the ETT 90 degrees counterclockwise will turn its bevel posteriorly and minimize the risk of catching on the structures of the glottic opening.22 After intubation, the position of the ETT is confirmed by conventional methods such as measurement of the end-tidal carbon dioxide concentration (EtCO2) and auscultation.
The EI is long enough to be useful for nasal intubations and can also be used to place supralaryngeal airways (SLAs) or double-lumen tubes.23 The long length of the EI enables it to be used as an airway exchange device; it can be placed down the lumen of a correctly placed ETT or SLA, which can then be removed over the introducer and discarded before a new airway is “railroaded” in its place. During the whole maneuver, the EI remains within the trachea, thereby guiding correct placement of the new airway. After the EI is removed, as always, the position of the new airway should be confirmed with the use of standard methods.
C Other Types of Intubating Guides
Many intubating guides of different sizes, shapes, lengths, and materials have been developed. All of the designs serve a function similar to that of the EI, but many have some additional features. Some are single-use devices that were designed after concern was raised regarding the possibility of prion transfer between patients with multiuse airway equipment. However, there is growing skepticism about whether disease transfer from reused but sterilized medical instruments poses any tangible risk to patients, whereas the risk to patients from the use of suboptimal airway equipment with limited clinical evaluation is very real. Clinicians should be wary of new equipment and always insist on using only instruments that have proved to be effective and safe.24
1 Frova Intubation Introducer
The Frova Intubation Introducer (Cook Inc., Bloomington, IN) is a single-use introducer, firmer than the EI, that has a 35-degree coudé tip, two side ports, and a hollow lumen (see Fig. 21-2). It comes with a Rapi-Fit connector that connects directly to standard ventilatory equipment, such as the bag of an air-mask-bag unit (AMBU) or an anesthetic circuit, enabling the Frova to also serve as a conduit for O2 delivery or ventilation. This requires extreme caution however, because high-pressure source ventilation via the narrow lumen may result in severe barotrauma. The Frova may be connected to an esophageal detection device so that one can confirm correct placement before “railroading” the ETT.25 The rigid, removable internal cannula is designed to increase the stiffness of the Frova; it has limited clinical indication and may increase the risk of trauma. The Frova introducer has two sizes: a 65-cm-long blue adult version for ETTs with greater than 5.5 mm inner diameter (ID) and a 33-cm-long yellow pediatric version for ETTs with 3.0 to 5.0 mm ID. First-pass success rates with the Frova introducer are similar to those with the EI and are substantially better than those of the similarly shaped Portex introducer.26 It is presumed that this success is due to the increased malleability of the EI and the Frova, which enables preshaping of the device, compared with the Portex introducer.26
2 Endotracheal Tube Introducer
The Endotracheal Tube Introducer (Sun Med, Largo, FL) is an example of a single-use version of the EI (see Fig. 21-2). It is similar to the EI in size and shape but 10 cm longer (i.e., 70 cm long). Like the Frova, it is stiffer than the EI. There are 10-cm markings on the top of the Sun Med introducer to indicate the depth of insertion. Although it is marketed as a single-use, disposable device, resterilization is possible.
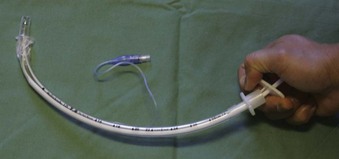
3 Parker Flex-It Directional Stylet
The Schroeder Oral/Nasal Directional Stylet, also known as the Parker Flex-It Directional Stylet (Parker Medical, Englewood, CO), is a disposable articulating stylet that requires no bending before intubation. Inserting the stylet into an ETT allows the clinician to elevate the tip of the ETT by wrapping all four fingers around the proximal ETT and using the base of thumb to depress the proximal end of the stylet (Fig. 21-3). Although the stylet is suitable for both oral and nasal intubation, it has been reported to be somewhat awkward to use, and the curvature created is not at the tip but rather over the distal half of the tube.27 However, it has been reported to be effective for difficult intubations (DIs) as well as for blind intubations.28
The effectiveness of intubating guides in patients with a DA has been well established.29–31 Most of these studies used the EI. With only a few exceptions, there are currently few data to support the use of the newer introducers for endotracheal intubation, particularly in patients with a history of DA. It should be emphasized that most of these new intubating guides and stylets are disposable and designed for single-use. In contrast, the EI is more cost-effective because it is reusable.
D Tube Exchangers
1 Cook Airway Exchange Catheter
The Cook Airway Exchange Catheter (CAEC; Cook Critical Care, division of Cook Inc.) is a hollow, flexible, straight tube that is designed as a tube exchanger for patients with a DA. The CAEC can be used to ventilate patients under difficult circumstances through the inner lumen and the distal ports after fitting the provided adaptor at the proximal end (see Fig. 21-2).
E Stylets
A stylet is a plastic-coated metal rod that can be placed inside the lumen of an ETT before intubation to stiffen or preshape the ETT. Unlike the EI and other introducers, the stylet should not protrude past the tip of the ETT, so as to avoid unnecessary trauma. Water-based lubricant should be used, and easy passage of the stylet in and out of the ETT should be demonstrated before use. The “best” shape for a stylet-shaped ETT depends on the clinician’s preference and the patient’s position and anatomy. However, Levitan and colleagues showed that the line of sight to the larynx can be improved if the stylet remains “straight to cuff,”32 at which point the ETT can then be bent to the desired angle (i.e., shaped like a hockey stick) (Fig. 21-4). An angle of 35 degrees or less reduces the risk of traumatic injury.32 Once the ETT has passed through the vocal cords, the stylet should be withdrawn as the ETT is advanced into the trachea.
In a randomized trial, Gataure and associates compared the efficacy of the EI with that of the malleable stylet in 100 patients with simulated DL (Cormack-Lehane grade 3 view) under general anesthesia. The EI group had a success rate of 96% after two attempts, compared with 66% in the stylet group.33
F Complications
Despite long-standing and widespread use, complications caused by ETT introducers, tube exchangers, and stylets are rare. To date, there have been only half a dozen case reports of pharyngeal, laryngeal, or tracheal perforation during airway manipulation that may have been caused by introducers or stylets.34,35 Reports of trauma during airway management frequently come from cases in which multiple attempts at securing the airway occurred and multiple devices were used, making it difficult to attribute damage to a single device. Because of their firmer material, single-use ETT introducers exert more pressure at the tip compared with the multiuse EI.26 Whether this corresponds to greater risk of airway trauma remains unknown.25 However, as with all airway devices, undue force should always be avoided. Holding an ETT introducer close to the coudé tip (i.e., with Magill’s forceps) increases the pressure exerted at the tip and therefore is not recommended.
After endotracheal intubation, all introducers and stylets should be inspected to ensure that no part of the device has been left behind. One report described a case in which the tip of an EI became detached and lodged in a patient’s airway,36 and in a similar case, plastic coating peeled off a stylet, blocking the ETT.37 An unusual case report described the involution of an ETT at its tip while the EI was being withdrawn, which caused the EI to lodge firmly within the ETT and necessitated removal of both instruments.38 Routine generous lubrication of intubating guides should reduce the likelihood of such events.
G Clinical Utility
Intubating introducers, stylets, and tube exchangers have been used successfully to facilitate endotracheal intubation for many decades. In particular, the EI is a cheap, reliable, and familiar tool in the hands of anesthesia practitioners and, more recently, those of emergency physicians and in the prehospital setting.39–42 Although the popularity of these nonvisual intubating techniques may decrease because of the improved glottic view afforded by the new video laryngoscopes, studies report the efficacy and usefulness of stylets and introducers to assist videoscopic intubation,43–48 suggesting that these instruments will remain a mainstay of intubating adjuncts.
III Lighted Stylets
A History
Macintosh and Richards are frequently credited with being the first to use a lighted stylet for orotracheal intubation. In 1957, they reported the use of a lighted introducer to assist the placement of an ETT in the trachea under direct vision using a laryngoscope.49 However, they did not describe the technique whereby transillumination of the soft tissues of the neck is used to guide the placement of the ETT. This transillumination technique was likely first described by Yamamura and colleagues, who reported the use of a lighted stylet for nasotracheal intubation in 1959.50
Modern lighted stylets use the principle of transillumination of the soft tissues of the anterior neck to guide the tip of the ETT into the trachea. This method takes advantage of the anterior (superficial) location of the trachea relative to the esophagus. When the tip of the ETT with the lighted stylet enters the glottic opening, a well-defined, circumscribed glow can be readily seen slightly below the thyroid prominence (Fig. 21-5A). However, if the tip of the ETT is in the esophagus, the transmitted glow is diffuse and cannot be readily detected under ambient lighting conditions (see Fig. 21-5B). If the tip of the ETT is placed in the vallecula, the light glow is diffuse and appears slightly above the thyroid prominence. Using these landmarks and principles, the clinician can guide the tip of the ETT easily and safely into the trachea without the use of a laryngoscope.
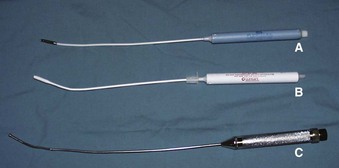
Despite its potential clinical advantages, intubation using a lighted stylet (lightwand) did not receive widespread popularity until a commercial intubating device became available. During the past 30 years, several versions of a lighted stylet have been introduced, including the Fiberoptic Lighted-Intubation Stilette (Benson Medical Industries Inc., Markham, Ont., Canada), the Flexilum (Concept Corporation, Clearwater, FL), the Tubestat (Concept Corporation), and the Fiberoptic Lighted Stylet (Fiberoptic Medical Products, Inc., Allentown, PA) (Fig. 21-6). Over the years, these devices have proved to be effective and safe in placing the ETT both orally and nasally.51–53 Despite favorable results and growing experience with the technique of light-guided intubation,51–54 early commercial lighted stylets had some limitations. These included: (1) poor light intensity; (2) short length, which limited the use of the lighted stylet device to short or cut ETTs; (3) absence of a connector to secure the ETT to the lighted-stylet device; (4) rigidity of the lighted stylet, which hampered use of the devices for other intubating techniques, including light-guided nasal intubation; and (5) single-use design in most lighted stylets, which increased the cost of intubation.
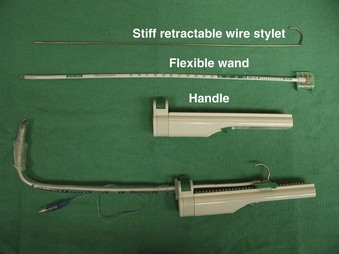
B Trachlight
The Trachlight consists of three parts: a reusable handle, a flexible wand, and a retractable metal wire stylet (Fig. 21-7). The power control circuitry and 3 AAA batteries are encased within the handle. The stylet or “wand” consists of a durable, flexible plastic shaft with a bright light bulb affixed at the distal end. Enclosed within the wand is a stiff but malleable, retractable wire stylet. This stylet may well be the most important feature of this device, because it significantly improves its ease of use.
A major feature of the Trachlight is its improved light source, which in most cases permits intubation under ambient lighting conditions. After 30 seconds of illumination, the light bulb blinks to minimize heat production and provide a convenient reminder of elapsed time. Because the tip of the stylet is encased within the ETT, and because of the efficient heat-exchange capacity of the upper airway mucosa, it is extremely unlikely that heat from the bulb would cause any thermal injury during intubation. An animal study confirmed that there were no histopathologic changes after use of the Trachlight.55
For standard orotracheal intubation, the retractable wire stylet is best used to shape the ETT into the form of a field-hockey stick (see Fig. 21-7). This configuration directs the bright light of the bulb against the anterior wall of the larynx and trachea. In addition, the hockey-stick configuration enhances maneuverability during intubation and facilitates placement of the ETT through the glottic opening. However, this is an awkwardly shaped object to advance into the trachea. Therefore, once the tip of the ETT-Trachlight (ETT-TL) unit has passed through the glottic opening, the wire stylet should be retracted by approximately 10 cm. This makes the distal end of the ETT-TL unit pliable and enables advancement into the trachea safely and without difficulty.
The glow emitted from the Trachlight can be seen to migrate down the patient’s neck and may be used to confirm correct placement of the ETT. When the glow reaches the sternal notch, the tip of the ETT is located about halfway between the vocal cords and the carina.56 The clamp securing the ETT to the Trachlight is released, and the Trachlight is removed, leaving the ETT in place.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree