Chapter 55 Medical-Legal Considerations
The ASA Closed Claims Project
I Historical Perspective
Anesthesiologists have a long-standing appreciation for risks associated with airway management. During the past 60 years, a variety of studies have demonstrated that events involving the respiratory system are a prominent cause of adverse outcomes in anesthesia practice.1–8 A few examples help illustrate this point. The Anesthesia Study Commission, which investigated anesthesia-related fatalities in metropolitan Philadelphia during the period 1935–1944, identified respiratory factors such as airway obstruction, hypoxia, and aspiration as the probable cause of death in approximately 19% of cases.7 A large, multicenter study by Beecher and Todd, conducted about a decade later when curare and other muscle relaxants were first entering clinical practice, led to the recognition of excess mortality associated with perioperative respiratory depression.1 In the 1970s, Utting and colleagues analyzed a 7-year series of anesthesia accidents reported to the Medical Defence Union of the United Kingdom (UK).8 Of 227 cases resulting in death or brain damage, 36% involved adverse respiratory events such as esophageal intubation, ventilator misuse, and aspiration.
Critical-incident studies have offered a similar picture. A landmark study in the late 1970s by Cooper and colleagues revealed that 29% of reported incidents were related to respiratory events such as airway mismanagement or failure and misuse of ventilators and breathing circuits.2 A decade later, the Australian Incident Monitoring Study provided a detailed analysis of the first 2000 cases voluntarily submitted since the late 1980s.6 In their collection of critical incidents, problems with ventilation accounted for 16% of reports from anesthesiologists in Australia and New Zealand.
II the Closed Claims Perspective
Claims represent only a small fraction of all adverse outcomes arising from medical care. The Harvard Medical Practice Study of patients in New York State in 1984 reported that approximately 4% of patients sustained an iatrogenic injury during hospitalization,9 but only 1 of every 8 injured patients filed a malpractice claim. Similar findings were described 10 years earlier by the Medical Insurance Feasibility Study in California.10 These small fractions make it unlikely that claims can be regarded as representing a cross section of all adverse outcomes.
A detailed description of data collection procedures for the Closed Claims Project has been reported previously.11,12 In brief, each claim file is reviewed by a practicing anesthesiologist, and a standardized form is used to record detailed information on characteristics of patients, surgical procedures, anesthetic agents and techniques, involved personnel, sequence of events, standard of care, critical incidents, clinical manifestations, responsibility, and outcome. Standard of care is rated on the basis of reasonable and prudent practices at the time of the event. Practice patterns that may have evolved at a later date are not retrospectively applied when the standard of care is rated. An adverse outcome is deemed preventable with better monitoring if the reviewer finds that the use—or better use—of any monitor would probably have prevented the outcome, whether or not such a monitor was available at the time of the event. An acceptable level of interrater reliability has been established for reviewer judgments on the standard of care and preventability of adverse outcomes with better monitoring.13
A Principal Features of Adverse Respiratory Outcomes and High-Frequency Adverse Respiratory Events
1 Basic Features
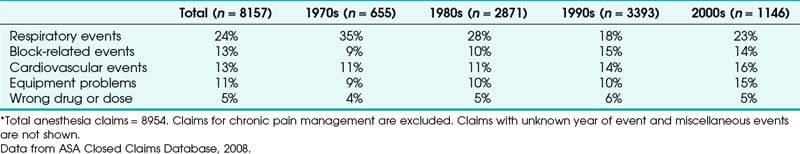
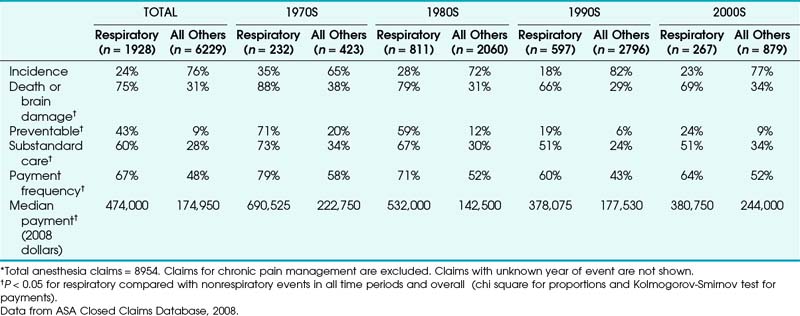
Adverse respiratory events constitute the single largest source of injury in the Closed Claims Project (Table 55-1). A detailed analysis of these events was initiated when the database reached a total of 1541 claims.14 The contrast between adverse respiratory events and other claims was particularly unfavorable. Respiratory event–related claims were (and still are) characterized by a high frequency of devastating outcomes and costly payments (Table 55-2).
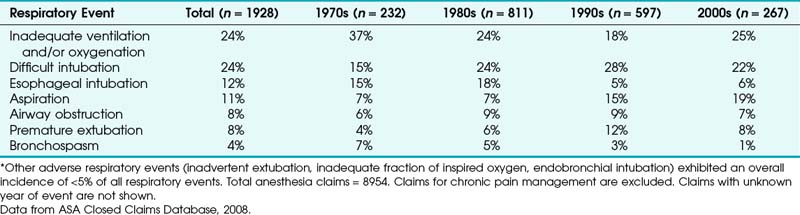
Just three mechanisms of injury accounted for almost two thirds of all claims for adverse respiratory events (Table 55-3). These mechanisms were inadequate ventilation (24% of cases), esophageal intubation (12%), and difficult intubation (DI; 24%). In the 1990s, after the adoption of pulse oximetry and end-tidal CO2 (EtCO2) as monitoring standards, DI (28%) and inadequate ventilation (18%) remained the most common adverse respiratory events, but esophageal intubation (5%) had decreased greatly compared with earlier decades (see Table 55-3). Evaluation of claims from the early 2000s suggests that this profile of adverse respiratory events is staying the same.
TABLE 55-3 Most Common Adverse Respiratory Events as Proportion of All Respiratory Events in Decade*
A detailed display of outcome and payment data for the three most common types of adverse respiratory events since 1990 (inadequate ventilation, DI, and aspiration) is shown in Table 55-4. Death and permanent brain damage were more frequent in claims for respiratory events compared with nonrespiratory events (P < 0.05). Claims for inadequate ventilation exhibited the highest proportion of death and brain damage (89%, see Table 55-4). Overall, payment for respiratory-related claims ranged from $1260 to $11 million (in 2008$). Most claims (61%) resulted in payment. Claims for adverse respiratory events typically involved healthy adults undergoing nonemergency surgery with general anesthesia (GA) (Table 55-5).
TABLE 55-4 Outcome, Payment, and Frequency for the Most Common Adverse Respiratory Events Occurring in 1990 or Later*
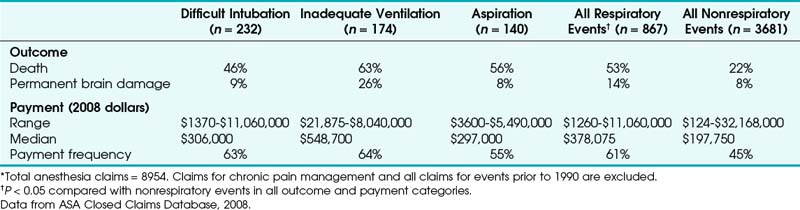
TABLE 55-5 Basic Clinical Features of Cases Involving Adverse Respiratory Events Occurring in 1990 or Later*
| Feature | Respiratory Events (n = 867) | All Others (n = 3681) |
|---|---|---|
| Age in years (mean ± SD) | 47.2 ± 19.8 | 45.5 ± 18.7 |
| Pediatric | 8% | 5% |
| ASAPS 1-2 | 42% | 53% |
| Emergency | 26% | 18% |
| Gender | ||
| Female | 51% | 59% |
| Male | 49% | 41% |
| Primary anesthetic | ||
| General | 81% | 62% |
| Regional | 4% | 27% |
| Monitored anesthesia care (MAC) | 8% | 6% |
| Other† | 7% | 6% |
ASAPS, American Society of Anesthesiologists Physical Status; SD, standard deviation.
* P < 0.05 for respiratory compared with nonrespiratory events in all categories (chi square test for proportions, t-test for age). Total anesthesia claims = 8954. Claims for chronic pain management and all claims prior to 1990 are excluded.
† Includes combined regional and general anesthesia, standby, and unknown.
Data from ASA Closed Claims Database, 2008.
2 Inadequate Ventilation
The largest class of adverse respiratory events was inadequate ventilation. The distinguishing feature in this group of claims was the reviewer’s inability to identify a specific mechanism of injury. In part, the inability to assign a mechanism of injury may reflect uncertainty on the part of the original health care providers. Because most adverse events occurred before the widespread use of pulse oximetry and capnometry, the uncertainty may be due to the limitations of traditional clinical signs, such as chest excursion, reservoir bag motion, and breath sounds. With increasing use of quantitative measures of ventilation, fewer cases have been assigned to the category of inadequate ventilation. These events have declined in occurrence from 37% of all respiratory events in the 1970s to 25% in the 2000s (see Table 55-3). It is also possible that a delayed rather than contemporaneous approach to the investigation of adverse outcomes is not powerful enough to provide an understanding of many events.
3 Esophageal Intubation
In 1990, we performed an in-depth analysis of 94 closed claims for esophageal intubation.14 Almost all (92%) of these claims occurred during the period 1975–1985, before routine use of intraoperative capnometry. The single most striking finding was that detection of esophageal intubation required at least 5 minutes in most cases (97%). Our immediate reaction was simply, “What took so long?” We wondered whether such delays in detection were caused by incompetence or negligence (e.g., intubation performed by a legally blind physician, minimal attention to the patient during the procedure), but we found only eight claims (9%) that could be explained in such a way.
Using this information, we constructed a best-case scenario by assuming that auscultation led to a correct diagnosis in the 3 cases in which it actually did so, as well as in the 61 cases in which there was no information about its role or the information was unclear. Using this approach of constructing a hypothetical situation to demonstrate the greatest possible benefit, auscultation is still associated with a misdiagnosis rate of 32% (30 of 94 cases). Although the limitations of auscultation are well known,15 we think these claims emphasize the importance of confirming intubation with the quantitative and ongoing information provided by capnometry.
Another indirect test of ventilation is cyanosis. Almost all of the esophageal intubation claims that we studied took place before pulse oximetry became part of the ASA Standards for Basic Anesthetic Monitoring. The human eye is relatively insensitive to the changes in skin color that occur during arterial desaturation,16,17 so it is not surprising that cyanosis preceded the recognition of esophageal intubation in only 34% of cases. One might also expect cardiovascular clues to accompany hypoxemia or hypercarbia and that these clues might alert the anesthesiologist to the possibility of esophageal intubation. Indeed, at least one major hemodynamic derangement was recorded in 79 (84%) of the 94 claims for esophageal intubation, and this knowledge preceded the recognition of esophageal intubation in 60 claims (65%). In order of frequency, the abnormalities included bradycardia, asystole, hypotension, unspecified dysrhythmia, tachycardia, and ventricular fibrillation (Table 55-6). Such changes certainly have the potential to serve as cues, but when they are extremely severe (e.g., ventricular fibrillation, asystole) they draw attention away from the underlying problem and leave very little time for effective remedies. These features point to the importance of confirmatory tests that provide early, direct, and ongoing confirmation of ventilation through the ETT.
TABLE 55-6 Major Hemodynamic Derangements Accompanying Esophageal Intubation Claims*
| Hemodynamic Derangement | Percent of Claims (n = 94) |
|---|---|
| Bradycardia | 57 |
| Asystole | 55 |
| Hypotension | 49 |
| Unspecified dysrhythmia | 10 |
| Tachycardia | 5 |
| Ventricular fibrillation | 1 |
* Percentages sum to more than 100 because of multiple derangements. Total anesthesia claims = 1541.
Data from ASA Closed Claims Database, 1990. Table adapted from Caplan RA, Posner KL, Cheney FW, et al: Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology 72:828, 1990.
Is injury from undetected esophageal intubation no longer a concern? As shown in Table 55-3, claims for esophageal intubation decreased considerably in the 1990s and later compared with the prior two decades. A few claims for esophageal intubation still enter the database, but they usually involve cases in which capnometry was unavailable or not used or the procedure took place in a remote location.18
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree