Chapter 26 Separation of the Two Lungs
Double-Lumen Tubes, Endobronchial Blockers, and Endobronchial Single-Lumen Tubes
III Indications for Lung Separation
A Absolute Indications
Absolute indications for lung separation (Box 26-1) include protective isolation of the normal lung, establishment of adequate gas exchange when there is a change in pulmonary compliance or lung pathology, and unilateral bronchopulmonary lavage.
Box 26-1 Indications for Separation of the Two Lungs or One-Lung Ventilation
Absolute Indications
Several unilateral lung conditions lead to inadequate ventilation. A large bronchopleural or bronchocutaneous fistula can lead to little or no ventilation of the nonoperative, healthy lung. In this situation, the increased compliance of the diseased lung results in direction of most of the positive-pressure ventilation (PPV) toward the diseased lung, minimally ventilating the normal lung and producing inadequate gas exchange. Conversely, a relatively noncompliant transplanted lung cannot compete with the better compliance of the native lung, and as a result, the healthy transplanted lung can be severely underventilated. Another scenario involves a lung with bullous or cystic disease or a lung with tracheobronchial disruption.1 Tension pneumothorax or tension mediastinum could result during these scenarios from elevated airway pressures that are often observed with SLV in the lateral decubitus position.
Patients with alveolar proteinosis may require unilateral bronchopulmonary lavage, which involves multiple instillations of large fluid volumes into the target lung with subsequent drainage of the effluent fluid.2–4 Lung separation is mandatory to avoid lung cross-contamination and drowning caused by the large volume of fluid required to perform the lavage.
B Relative Indications
Relative indications for lung isolation involve facilitating surgical exposure, avoiding lung trauma, and improving gas exchange. Operations such as repair of thoracic aneurysms, pneumonectomy, pulmonary lobectomies (especially of the upper lobe), video-assisted thoracoscopic surgery, esophageal surgery, and anterior spinal surgery all benefit from the optimized surgical exposure afforded by SLV (see Box 26-1). Lung isolation further improves recovery by minimizing lung instrumentation and trauma to the nonventilated, nondependent lung. In cases of unilateral lung trauma, oxygenation and recovery may be optimized with SLV by improving  matching.
matching.
IV Techniques
A Double-Lumen Tubes
1 Anatomy
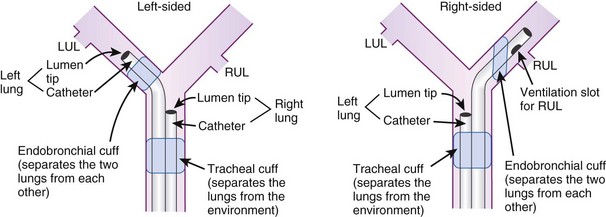
DLTs are essentially two tubes bonded together with a design that allows each tube to ventilate a specified lung. DLTs are right-sided or left-sided devices. Left-sided DLTs have a bronchial port that extends into the left main stem bronchus and a tracheal port that is designed to sit above the carina. In right-sided DLTs, the bronchial port extends into the right main stem bronchus, and the tracheal port sits above the carina. The cuff of the right-sided DLT may be at an oblique angle to facilitate ventilation of the right upper lobe bronchus at the Murphy eye (Fig. 26-1).
The original DLTs were reusable, red rubber tubes with high-pressure cuffs that became stiff and brittle over time, making placement more difficult and traumatic. Newer DLTs are made of nontoxic plastic (the Z-79 marking) and are disposable. As the plastic warms up from the surrounding body temperature, the DLT conforms to the anatomy of the patient. This increased malleability, however, makes it more difficult to reposition the same tube. Current DLTs employ high-volume, low-pressure, color-coded cuffs. The bronchial cuff and its pilot balloon/connector are blue. The tracheal cuff and its pilot balloon/connector are clear or white. Cuff inflation pressure requires a balance between preserving an adequate seal and maintaining mucosal perfusion. Measured cuff pressures between 15 and 30 mm Hg achieve these goals.5–8 In cases involving the use of nitrous oxide, the cuff pressures should be checked periodically.
DLTs come in various French (F) sizes: 28, 32, 35, 37, 39, and 41, and 1 F equals an approximately 0.33-mm measurement of the outer diameter (OD). In most adult men, a 39-F DLT fits well, having adequate length and appropriate diameter, while providing the capability of suctioning or fiberoptic bronchoscopy (FOB), and a 37-F DLT fits most adult women. A radiopaque line may be seen at the end of each lumen to allow for radiographic positioning. A Y-adapter for the proximal end allows ventilation of both lumens through a single circuit. The cross section of the DLT is designed as one round bronchial lumen and one crescent-shaped tracheal lumen. Left- and right-sided DLTs are curved at the distal end to enable advancement into the respective main stem bronchus. DLTs from different manufacturers have their own characteristic feel and slight modifications to the basic design described. The depth required for insertion of the DLT correlates with the height of the patient. For any adult 170 to 180 cm tall, the average depth for a left-sided DLT is 29 cm. For every 10-cm increase or decrease in height, the DLT is advanced or withdrawn 1.0 cm.9
3 Disadvantages
The most significant disadvantages of the DLT are related to its size. Intubation with a DLT is often more difficult than with an SLT.6 Intubation is even more complex in patients with difficult airway anatomy.10 In cases of a distorted or compressed tracheobronchial tree, placement of a DLT can be impossible due to its size and rigidity. DLT size can contribute to airway damage during placement and when the device is left in place for a long period. Because of some difficulty managing DLTs in the ICU with regard to weaning and pulmonary toilet, they are often exchanged for SLTs. The process of exchanging a DLT for an SLT can be dangerous, especially after procedures in which airway edema has occurred. Although DLT lumens are relatively large, FOB may be cumbersome due to the extended length of each tube and the narrowed crescent shape of the tracheal lumen. Multiple ports and connections further require a good working knowledge of the DLT anatomy to prevent errors in ventilation and management.
4 Selection
a Right-Sided Versus Left-Sided Double-Lumen Tubes
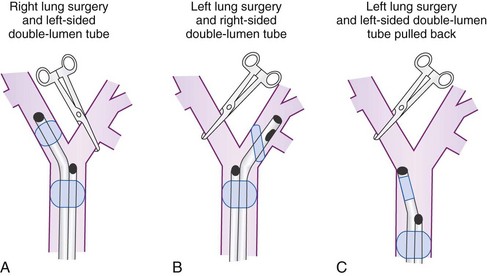
To minimize tube displacement, it may be recommended that the nonoperated bronchus be intubated (i.e., using a left-sided DLT for a patient undergoing right lung surgery) (Fig. 26-2).11 However, controversy exists in regard to left lung procedures because of the anatomic variability of the right upper lobe. The bronchial port of a right-sided tube may be difficult to position for adequate lung isolation and ventilation of the right upper lobe bronchus. This can result in difficulties during surgery, including severe hypoxia during isolated right lung ventilation.12
Many anesthesiologists prefer to use left-sided DLTs for all lung surgeries (see Fig. 26-2); however, there are insufficient data to support actual increased safety, as opposed to the perception of safety when intraoperative hypoxia, hypercapnia, and high airway pressures are used as criteria.13,14 If manipulation of the left main stem bronchus is required, the left-sided DLT is withdrawn and repositioned with the bronchial port above the carina. For operations on the left main stem, including sleeve resection, it may be preferable to use a right-sided DLT (Fig. 26-3).
Contraindications for use of a DLT include anatomic barriers that make positioning improbable or dangerous, such as carinal or bronchial lesions, strictures, vascular compression by aortic aneurysm, and aberrant bronchus.6,15,16 Right-sided DLTs may be indicated in cases with tortuosity and compression of the trachea or left main stem bronchus, which can make placement of a left-sided DLT impossible. Newly designed DLTs may be applicable for patients with special conditions including those with unusual anatomic variability.17
b Double-Lumen Tube Size
The ideal size of a DLT is one that results in a near-complete seal of the bronchial lumen without inflation of the cuff. The high inflation pressures of a small tube can cause as much mucosal damage as forcing too large a tube into a small bronchus.18 Even when height- and weight-based size estimates are used, it is impossible to choose the correct size of tube every time.15,19 Commonly, a 39-F or 41-F DLT is selected for men and a 37-F or 39-F DLT for women of average height and build. The intentional use of smaller DLTs has not had significant clinical benefits.20 A flexible fiberoptic bronchoscope (FFB) may be passed through the bronchial lumen to assess appropriate diameter and length of the DLT during placement (Table 26-1).
TABLE 26-1 Relation of Flexible Fiberoptic Bronchoscope Size to Double-Lumen Tube Size
| FFB OD Size (mm) | DLT Size (F) | Fit of FFB inside DLT |
|---|---|---|
| 5.6 | All sizes | Does not fit |
| 41 | Easy passage | |
| 39 | Moderately easy passage | |
| 4.9 | 37 | Tight fit, needs lubricant,* hand push |
| 35 | Does not fit | |
| 3.6-4.2 | All sizes | Easy passage |
| Approximately 2.0 | All sizes | Most operating rooms need special arrangements to obtain this size FFB |
DLT, Double-lumen tube; FFB, flexible fiberoptic bronchoscope; OD, outer diameter.
* Lubricant recommended is a silicon-based fluid made by the American Cystoscope Co.
5 Positioning
Malposition of the DLT can lead to life-threatening consequences. Ventilation can be severely impaired, leading to hypoxia, gas trapping, tension pneumothorax, cross-contamination of lung contents, and interference with surgical procedures. Multiple studies have shown that DLTs are often malpositioned.15,19 On the basis of these studies, indirect visualization with a FFB may be used routinely for confirmation of positioning. Various techniques using a FFB are discussed in the following sections.
a Placement of the Double-Lumen Tube
DLTs are placed similar to SLTs but with some additional maneuvers and considerations. DLTs are larger in diameter and longer than SLTs, making them more difficult to place. It is important never to force a DLT into position. For laryngoscopy, the shoulder of a Macintosh blade provides better tongue displacement and more space through which to insert the tube. The use of a video laryngoscope has also been described as effective and potentially time-saving.21 The bronchial tip of the DLT is placed through the cords, and the stylet is then removed to prevent trauma. After the bronchial portion has passed the cords, the DLT must be rotated 90 degrees toward the selected side of the bronchial lumen to sit properly. If resistance is encountered on rotating or advancing the tube, the use of a smaller tube needs to be considered. The average depth of insertion is 29 cm for a 170-cm individual. For each 10-cm increase or decrease in height, the tube depth is increased or decreased by 1 cm, respectively.15 When the tube depth is reached, the tracheal cuff is inflated, and the patient is connected to the ventilator. Care must be taken not to tear or puncture the tracheal cuff during intubation. For example, covering the teeth with an unopened alcohol swab can minimize cuff damage.
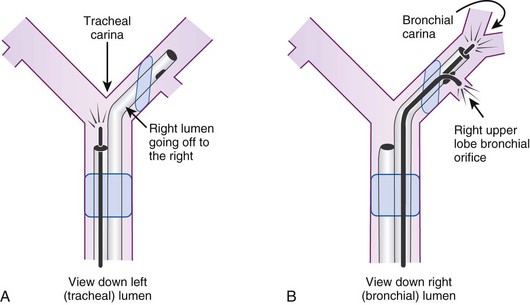
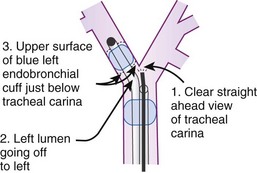
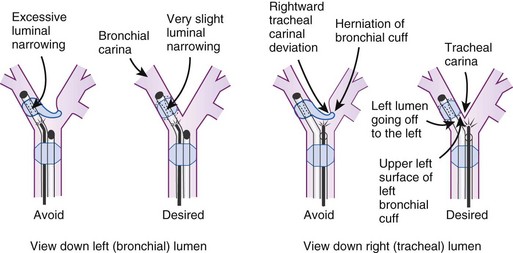
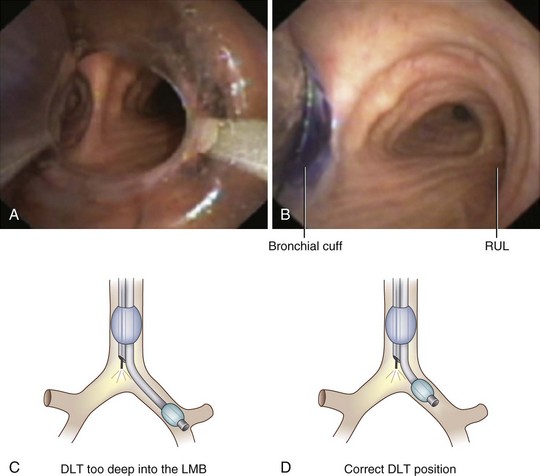
After confirmation of CO2 return and initiation of ventilation, an FFB is placed through the tracheal lumen (Fig. 26-4). The FFB is advanced, and the carina is identified. The bronchial lumen of the tube must be visualized entering the appropriate main stem bronchus (i.e., the bronchial lumen should be in the left main stem bronchus for a left-sided DLT). The balloon of the bronchial lumen should be inflated under direct vision and should lie just distal to the carina. The tube may have to be repositioned to visualize the balloon. Direct visualization of the balloon inflation helps to confirm tube position and size. Some DLTs have an indicator line just proximal to the bronchial cuff that should sit at the level of the carina. Direct visualization may be necessary to ensure that the bronchial balloon does not herniate over the carina or that the tracheal portion of the DLT does not encroach on the carina (Fig. 26-5).
An alternative method of DLT placement is to use the FFB as an intubating stylet to guide the bronchial tip of the DLT directly into the correct main stem bronchus (Fig. 26-6). This is accomplished by inserting the FFB through the bronchial port of the DLT after the bronchial tip has passed the vocal cords. The FFB is then advanced down the trachea while identifying the anterior-posterior and right-left orientation. The FFB is advanced further to identifying the carina and the right and left main stem bronchi, then advanced into the appropriate bronchus. The DLT is advanced over the FFB. It is then necessary to remove the FFB after confirming that the bronchial tip is not obstructed and is proximal to the secondary bronchial branches. The FFB is then placed in the tracheal lumen to confirm the position of the bronchial cuff and to ensure that the tracheal lumen is not encroaching on the carina. This technique allows for assessment of the carina and tracheal rings and allows placement in tortuous airways. However, it takes more time to perform, and in some patients with poor pulmonary reserve, this extra time can lead to desaturation.
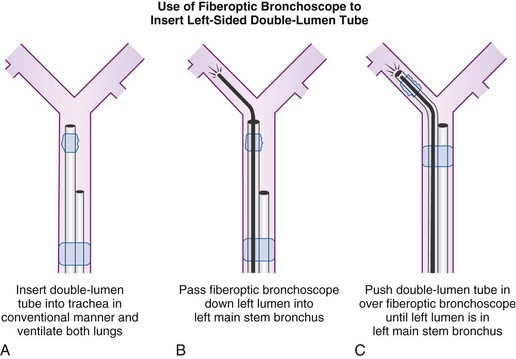
Figure 26-6 A double-lumen tube (DLT) can be put into the trachea in a conventional manner, and both lungs can be ventilated by both lumens (A). A flexible fiberoptic bronchoscope (FFB) may be inserted into the left lumen of the DLT through a self-sealing diaphragm in the elbow connector to the left lumen; this allows continued positive-pressure ventilation of both lungs through the right lumen without creating a leak. After the FFB has been passed into the left main stem bronchus (B), it is used as a stylet for the left lumen (C); the FFB is then withdrawn. Final precise positioning of the DLT is performed with the FFB in the right lumen (see Figs. 26-19 and 26-20).
(From Benumof JL: Anesthesia for thoracic surgery, Philadelphia, 1987, Saunders.)
b Confirmation of Proper Placement
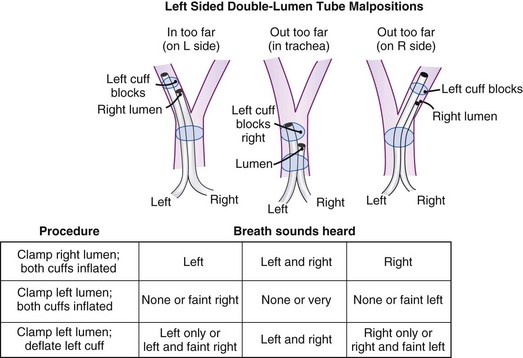
Many maneuvers have been described to assess the proper position of a DLT,22,23 including visualization of chest excursion while alternately clamping and unclamping the tracheal and bronchial ports, auscultation of lung fields while alternately clamping and unclamping the tracheal and bronchial ports (Fig. 26-7), and radiographic confirmation.24,25
The most important advance in checking for the proper position of a DLT is the FFB (Fig. 26-8). Smith and colleagues26 demonstrated that when the disposable DLT was thought to be in the correct position by auscultation and physical examination, subsequent FOB showed that 48% of the tubes were malpositioned. Malpositions may not be clinically significant and may be missed by the clinician. When using a left-sided DLT, the bronchoscope is usually first introduced through the tracheal lumen to visualize the carina and to ensure that the bronchial cuff is not herniated. The upper surface of the blue endobronchial cuff should be just below the tracheal carina; the blue bronchial cuff of the disposable DLT is easily visualized. The bronchoscope is then passed through the bronchial lumen to identify the left upper lobe bronchial orifice. When a right-sided DLT is used, the carina should be visualized through the tracheal lumen, and the orifice of the right upper lobe bronchus should be identified when the bronchoscope is passed through the right upper lobe ventilating slot of the DLT.
Pediatric FOBs are available in several standard sizes: 5.6-, 4.9-, and 3.6-mm OD. The 4.9-mm OD bronchoscope can be passed through DLTs that are 37 F or larger. A 3.6-mm or smaller diameter bronchoscope is easily passed through all sizes of DLTs.27–29
DLT placement must be rechecked when the patient is repositioned, because movement of the tube is common. Training in the use of FFBs may be achieved during evaluation of any SLT-intubated patient and through the use of airway simulation and mannequins.30
6 Malpositioning and Complications
Use of a DLT is associated with a number of problems, the most important of which is malpositioning (see Fig. 26-7).26,31 The tube can be malpositioned in several ways.
A right-sided DLT may occlude the right upper lobe orifice. The mean distance from the carina to the right upper lobe orifice is 2.3 ± 0.7 cm in men and 2.1 ± 0.7 cm in women. With right-sided DLTs, the ventilatory slot in the side of the bronchial catheter must overlie the right upper lobe orifice to permit ventilation of this lobe. However, the margin of safety is extremely small and varies from 1 to 8 mm.32 It is difficult to ensure proper ventilation to the right upper lobe and avoid dislocation of the DLT during surgical manipulation.
The left upper lobe orifice may be obstructed by a left-sided DLT. Traditionally, the take-off of the left upper lobe bronchus was thought to be at a safe distance from the carina and that it would not be obstructed by a left-sided DLT. However, the mean distance between the left upper lobe orifice and the carina is 5.4 ± 0.7 cm in men and 5.0 ± 0.7 cm in women.33 The average distance between the openings of the right and left lumens on the left-sided disposable tubes is 6.9 cm. An obstruction of the left upper lobe bronchus is possible while the tracheal lumen is still above the carina. There is also a 20% variation in the location of the blue endobronchial cuff on the disposable tubes because this cuff is attached to the tube at the end of the manufacturing process.
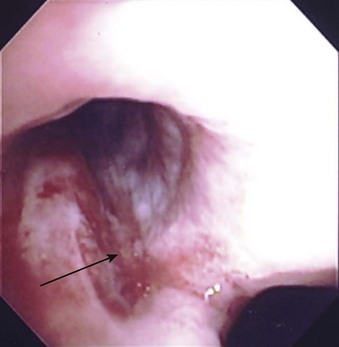
A rare complication with DLTs is tracheal laceration or rupture from the stiff tip of the bronchial lumen (Fig. 26-9). Overinflation of the bronchial cuff, inappropriate positioning, and trauma due to intraoperative dislocation that resulted in bronchial rupture have been associated with use of the Robertshaw tube and the disposable DLT.34 The pressure in the bronchial cuff should be assessed and decreased if the cuff is overinflated. If lung isolation is unnecessary, the bronchial cuff should be deflated and then reinflated slowly to avoid excessive pressure on the bronchial walls. The bronchial cuff should also be deflated during any repositioning of the patient unless lung separation is absolutely required during this time.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 ) matching may occur. Excess positive end-expiratory pressure (PEEP), airway pressures, hypoxia, hypercapnia, and hypovolemia may contribute to an increase in PVR of the dependent lung, thereby increasing the shunt fraction. Improvement of the shunt fraction can be accomplished by decreasing blood flow or supplying O2 to the nondependent lung.
) matching may occur. Excess positive end-expiratory pressure (PEEP), airway pressures, hypoxia, hypercapnia, and hypovolemia may contribute to an increase in PVR of the dependent lung, thereby increasing the shunt fraction. Improvement of the shunt fraction can be accomplished by decreasing blood flow or supplying O2 to the nondependent lung.