ACKNOWLEDGMENTS
The authors of the current chapter gratefully acknowledge the contributions of David Shahian, MD, Vice President, and Laura Rossi, RN, Staff Specialist, Center for Quality and Safety, Massachusetts General Hospital.
I. HANDOFFS DEFINED—A handoff is defined by the Joint Commission as “the process of transferring primary authority and responsibility for providing clinical care to a patient from one departing caregiver to one oncoming caregiver.”
A. In the ICU setting, caregivers include, but are not limited to, attending, fellow and resident physicians; nurse practitioners; physician assistants; nurses; respiratory therapists; physical therapists; occupational therapists; and pharmacists.
II. ESSENTIAL ROLE OF COMMUNICATION IN ADVERSE EVENTS—Handoff quality is heavily dependent on good communication, and it is widely accepted that poor communication plays a substantial role in adverse events. Below are two examples that highlight these relationships.
A. Joint Commission Sentinel Event Alerts—The Joint Commission collects voluntarily submitted sentinel event reports from hospitals nationwide. Data collection began in 1996, and resulted in publication of Sentinel Event Alerts since 1998.
1. Communication is among the top three root causes of sentinel events resulting in patient harm or death each year.
2. In 2013, communication was the second most commonly reported root cause, playing a role in 563 out of 887 total reported cases.
3. From 2004 to 2013, communication was the most commonly reported root cause in cases of delayed treatment, playing a role in 728 out of 903 total reported cases.
B. Closed Malpractice Claims—Analysis of closed malpractice claims has identified communication as a significant factor in adverse patient events leading to litigation.
1. Obstetric anesthesia—Of all adverse events, 31% are related to communication problems. Obstetric newborn death/brain damage cases involving anesthesia had an increased proportion involving poor communication.
2. Surgical cases—Systems factors contributed to error in 82% of malpractice cases, with communication breakdown comprising 24% of system factors.
3. Cases involving trainees—Teamwork breakdowns contributed to 70% of malpractice cases, with handoff problems being a leading cause of teamwork breakdown.
III. COMMUNICATION AND TEAMWORK STRATEGIES IN OTHER INDUSTRIES—Many high-risk industries have realized the importance of standardized communication and have devised strategies for structuring communication between team members. Notable examples include the aviation industry and the military.
A. Airline Industry
1. Sterile cockpit rule
a. In the early 1980s, the FAA identified that crew distractions by non–flight-related activities contributed significantly to a large number of air accidents and incidents.
b. A review of the aviation safety reporting system database demonstrated incidents related to issues such as extraneous conversation (including with the control tower), distractions from the flight attendants, nonpertinent radio calls and PA announcements, and sight-seeing. Some of these incidents resulted in fatalities.
c. These incidents led directly to the implementation of the Sterile Cockpit Rule in 1981. This rule states that during “critical phases of the flight” (ground operations, takeoff, landing, and all flight operations below 10,000 feet), crew are prohibited from performing duties other than those required for safe operation of the aircraft.
2. Crew resource management
a. Root cause analysis of plane crashes in the 1970s revealed that failures of communication and teamwork resulted in significant risk. These investigations resulted in a recommendation for teamwork training programs for flight crews, the first of which was held by NASA in 1979.
b. The improvement program is designed to enhance team situational awareness and communication by using standardized techniques called inquiry and advocacy and fosters a questioning attitude among team members. This involves standardized communication, outlined below, to escalate concerns or questions:
1. Get the person’s attention.
2. State your concern.
3. State the problem as you see it.
4. State a solution.
5. Obtain agreement.
IV. COMMUNICATION STRATEGIES ADAPTED FOR HEALTH CARE: TeamSTEPPS
This evidence-based program for improving teamwork in hospitals was developed and distributed by the Agency for Healthcare Research and Quality (AHRQ) and the Department of Defense (DoD). With the goal of enhancing team situational awareness, TeamSTEPPS involves a readiness assessment, implementation, and sustainment phases. The program was field-tested and then fully implemented at many hospitals throughout the country, with plans to disseminate to all hospitals nationwide. There are four core competencies that are crucial for ensuring effective team performance:
A. Team Leadership
B. Situation Monitoring
C. Mutual Support
D. Communication
TeamSTEPPS promotes an environment of open communication and candor, where everyone on the team feels comfortable “speaking up.”
V. TYPES OF HANDOFFS IN THE ICU—There are several different types of handoffs. Below are several of the major categories in which an effective and efficient transfer of patient responsibility is necessary.
A. Shift-to-shift Handoff—This is a direct transfer of responsibility for the patient from one clinician to another for a defined period of time. With changes in resident work hours, health care delivery models have required more handoffs as day teams sign out to their night teams to ensure continued clinical coverage. The departing clinician must deliver an efficient and informative overview of the patient’s current clinical condition over the past shift (8–12 hours) and provide an update on any anticipated events over the next 8 to 12 hours.
B. Permanent Unit-to-unit Handoff—This is a permanent (or semipermanent) change in location of a patient from a sending clinical unit to a receiving clinical unit. Examples include emergency room or operating room to ICU and ICU to floor.
C. Temporary Unit-to-unit Handoff—As implied, this is a temporary transfer of clinical responsibility of a patient for some length of time, typically for a procedure or diagnostic test. For example, locations for temporary transfer may include interventional radiology, imaging, or operating room with plans to return to the ICU.
D. External Transfer—patient being admitted to or discharged from the hospital. This is a handoff between the referring facility and the accepting facility. It should cover all of the same information as an internal transition of care, plus additional information that may be less readily available to the receiving provider outside the organization (such as copies of reports for procedures, tests, etc.).
E. Escalating an Acute Situation—If there is a rapid and significant change in a patient’s clinical condition, it is paramount that that information be efficiently and effectively communicated up the chain of command.
F. Ongoing, Living Record of Patient History of Hospital Course—Included as part of written sign-out only, the background and history of the patient’s hospital course should be updated at least daily and can reside in the electronic record.
VI. WRITTEN AND VERBAL HANDOFFS—In both the written and verbal handoffs, it is important that the giver of the handoff dedicate time to prepare a comprehensive, well-organized synopsis of the patients being transferred to the receiving clinician.
A. Verbal Handoff—should include an efficient synopsis of the patient’s clinical condition given by the sending clinician to a receiving clinician. There are several different styles by which verbal handoffs are given, but generally they should include the following information, as exemplified by several recently published handover studies, including I-PASS (see below):
1. Patient’s current clinical condition, in brief—This should be communicated so that all clinicians are speaking the same “language” and have the same perception of the terminology (e.g., “LOL” has several meanings).
2. A brief summary of patient’s treatment, condition, and history. The length and amount of detail will depend on the clinical complexity of the patient.
3. A sign out of tasks that require attention (e.g., ordering medications, checking test results, actions to be taken, etc.)
4. Anticipatory planning for potential events and who needs to be notified (e.g., suggested actions for clinical deterioration—if “X” happens, do “Y.”)
5. An opportunity for the receiver of the handoff to ask questions and convey their understanding or concerns
B. Written Handoff: This is typically a paper or electronic document to accompany the verbal handoff.
1. Usually follows a more detailed format than a verbal handoff
2. Many electronic medical record (EMR) solutions include a handoff tool that is integrated into the system. This is designed to improve communication, allowing each role group access to view each other’s handoff notes (i.e., physician can see a nurse’s sign out on the same patient and vice versa).
VIII. COMMONLY USED HANDOFF TOOLS—There are a variety of tools available for handoffs. Two common approaches are detailed below:
A. SBAR
1. Components and mnemonic
a. S = Situation: a concise statement of the problem
b. B = Background: pertinent and brief information related to the situation
c. A = Assessment: analysis and considerations of options—what you found/think
d. R = Recommendation: action requested/recommended—what you want
2. This tool was developed by the Navy—it is not health care specific
3. Intended for unexpected or escalation situations, but has been adapted successfully for other scenarios, as well
4. Provides clinicians with a predictable and structured framework for communication that is standardized across settings
B. I-PASS
1. Components and mnemonic (Fig. 37.1)
a. I = Illness Severity: Standard language of stable, “watcher,” or unstable
b. P = Patient Summary: summary statements of events leading up to admission, the hospital course, ongoing assessment, and the plan of care
c. A = Action List: a “to-do” list with timeline and assigned ownership
d. S = Situational Awareness/Contingency Planning: high-level context of patient care and plans for potential complications or events (i.e.. if “X” happens, do “Y.”)
e. S = Synthesis by receiver: receiver recaps handoff, restating key items and asking questions; encourages active listening and participation of receiver
2. Two multisite studies published the following:
a. Ten site study with ~50% reduction in medical errors
b. Twenty-three site study in children showing ~30% reduction in medical errors
3. Adaptable for all clinical disciplines, though originally created for physicians
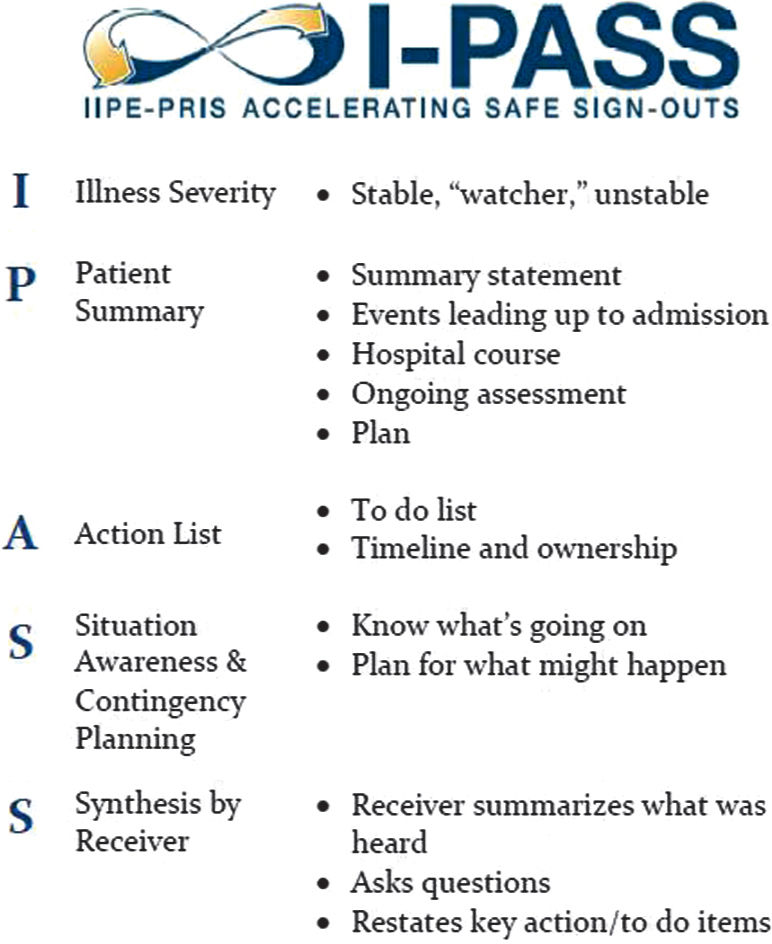
FIGURE 37.1 I-PASS framework (From Starmer A, Spector N, Srivastava R, et al. I-PASS, a mnemonic to standardize verbal handoffs. Pediatrics 2012;129:201–204, with permission).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







