Hemorrhoids
Steven Lowy MD
Hemorrhoids (sometimes referred to as piles) are tumors made up of enlarged rectal and anal veins along with reactive tissue surrounding those veins. Although a common condition and one that causes significant patient discomfort and concern, hemorrhoids most often can be managed conservatively with good result, especially early in their course. Correct diagnosis is paramount, though, because hemorrhoids can coexist with other, more serious disease entities that cause similar symptoms.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
There are two sets of hemorrhoidal veins: the superior hemorrhoidal plexus, which gives rise to internal hemorrhoids, and the inferior plexus, which gives rise to external hemorrhoids. The superior plexus is connected to the relatively high venous pressure of the portal system, lies above the dentate line in its normal position, and is covered by rectal mucosa. The inferior plexus has little connection to intra-abdominal venous pressure, lies below the dentate line, and is covered by perianal skin.
Factors associated with the formation of hemorrhoids include the following:
Genetic predisposition
Increased venous pressure from various causes (eg, overlong sitting on the toilet seat, straining at constipated stool, prolonged standing, heavy lifting, coughing, pregnancy or other pelvic masses, and portal hypertension)
Diarrhea
Rectal tumors and causes for incomplete evacuation of stool from the rectum that cause excessive straining to empty the rectum.
Whatever the cause, formation of an internal hemorrhoid begins with swelling of a venous structure of the superior plexus, usually as a slow and gradual process. As the vein enlarges it pushes its covering mucosa into the lumen of the rectum. Once in the lumen it is subject to the expelling forces of defecation and gradually enlarges as peristalsis and fecal flow push it toward the anus.
As it stretches, the vein becomes attenuated and prone to bleeding, which is often the first symptom of a hemorrhoid. Although bleeding from a hemorrhoid is usually described as bright-red drops of blood in the toilet bowl or on the toilet tissue after defecation, it may be so slight as to go unnoticed or, in contrast, may have the quality of an arterial bleed, leading to hypotension and shock. Eventually, the hemorrhoidal mass can become large and long enough to extend below the dentate line and beyond the anal verge: at this point it becomes a prolapsed hemorrhoid.
EPIDEMIOLOGY
Exact epidemiologic data are difficult to determine because hemorrhoids are so common and are often not reported. Typical Western diets consisting of highly refined foods and little roughage cause firm, dry stools that are difficult to pass and lead to excessive straining at defecation. In poorer parts of the world, where food is less processed, hemorrhoids are less common.
DIAGNOSTIC CRITERIA
Diagnosis is made on the basis of history and a thorough examination. It is essential not to reach a diagnosis of hemorrhoids too quickly. Although hemorrhoids are the most common cause of many of the noted symptoms, other, more ominous processes, particularly rectal carcinoma, can cause these same symptoms. Benign conditions such as anal fissures and condylomata can also cause similar symptoms, but they require different treatment. A thorough digital examination and colonoscopy with particular attention to the rectosigmoid should be part of every diagnostic workup.
HISTORY AND PHYSICAL EXAMINATION
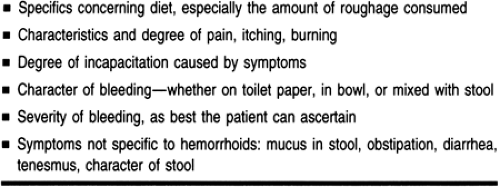
Bleeding and rectal discomfort are the most common complaints voiced about hemorrhoids. Essentials of the history are noted in Table 25-1. When the hemorrhoid prolapses, the following symptoms may appear, even if the prolapse is fully reducible manually or reduces spontaneously:
A sense of incomplete evacuation and rectal tenesmus
Irritation and itching
Mucosal ulceration (another cause of bleeding)
Acute onset of severe pain and swelling secondary to thrombosis.
Physical findings for internal hemorrhoids are one or more intrarectal masses, usually soft and sometimes tender, with or without the presence of bright-red blood. Characteristically, the bleeding of hemorrhoids coats the stool, whereas the stool itself is negative for occult blood; the finding of stool that is positive for occult blood should reinforce the need for a complete diagnostic workup of the gastrointestinal tract.
If internal hemorrhoids are large, they may be seen prolapsing through the anus or may prolapse as the finger is removed from the rectum. Thrombosed hemorrhoids can be firm, although not nearly so hard as a carcinoma, and are quite tender early in their course; there may be significant anal sphincter spasm. A prolapsed and thrombosed hemorrhoid presents as a
swollen, firm mass protruding through the anus with mucus and possibly ulceration. With resolution, there may remain only redundant tissue in the rectum, because the resultant fibrosis after thrombosis may actually cure the patient of that particular internal hemorrhoid. Chronic internal hemorrhoids may result in the formation of anal skin tags.
swollen, firm mass protruding through the anus with mucus and possibly ulceration. With resolution, there may remain only redundant tissue in the rectum, because the resultant fibrosis after thrombosis may actually cure the patient of that particular internal hemorrhoid. Chronic internal hemorrhoids may result in the formation of anal skin tags.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree