GENITOURINARY TRAUMA
RENAL TRAUMA
Epidemiology
Trauma patients suffer renal injury at rates of 1.4%-3.25% with proportionally higher rates seen in younger patients and in men (3:1 male to female).–13 Most renal trauma in the United States and Europe is blunt (95%-97%),2,4 but there are major worldwide differences in the mechanism of renal injury (i.e., Turkey 31% blunt).5,6 The most common blunt mechanism is motor vehicle accident and the most common penetrating injuries are from stab and gunshot wounds, with penetrating traumas having a proportionally higher rate of severe injury.2 With the advent of sophisticated renal trauma imaging and grading systems, the majority of contemporary renal traumas can be managed nonoperatively.7
Pathophysiology
Blunt Renal Trauma. The kidneys are relatively protected organs, surrounded by the abdominal viscera anteriorly, the diaphragm and liver superiorly, and the back muscles and spine anteriormedially. This degree of protection means that only major blunt forces to the body lead to renal trauma, explaining the high rate of associated injuries to surrounding viscera (20%-94%).8,9
Motor vehicle accidents and falls are the most common mechanism for blunt renal trauma, with injuries coming both from direct impact of the abdominal wall and ribs with the kidney and from secondary impacts during the acute deceleration. The renal pedicle is especially prone to deceleration injuries. Because the renal vein and artery are the kidney’s most secure attachments, they absorb the majority of the force during deceleration, leading to both tears and thrombosis of the renal vasculature. Parenchymal injuries of the kidney can result from both direct and secondary impacts with the surrounding musculature, the 11th and 12th ribs and the spinous processes8,10 (Fig. 29.1).
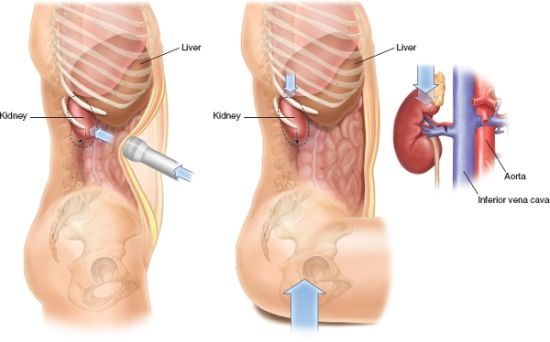
FIGURE 29.1. Mechanisms for blunt injury of the renal parenchyma.
Penetrating Renal Trauma. Penetrating trauma tends to be more severe and more unpredictable than blunt trauma. Gunshot injuries can damage the kidney from both direct impact of the bullet (permanent cavity) and from the bullets blast effect (temporary cavity), with high-velocity bullets leading to relatively more damage.6 With stab wounds, the path of the injury can sometimes provide insight into the severity of injury. Wounds posterior to the anterior axillary line will more often lead to parenchymal injury only, most of which can be managed nonoperatively. Conversely, anterior renal injuries are more likely to injure the hilar strictures, which tend to be more life threatening in nature and require operative management, though use of these anatomical landmarks should never supplant appropriate imaging when possible.11
Initial Evaluation
Physical Exam. Historical and clinical findings suggestive of blunt renal trauma include hematuria, flank pain, flank ecchymoses, fractured ribs, and abdominal distention, with hematuria being the most common finding (80%-94%)12 (Fig. 29.2).

FIGURE 29.2. Typical physical exam findings in a patient that has suffered blunt renal trauma. (From Dr. Jack McAninch, with permission).
Laboratory. An evaluation of the urine should be done in all trauma patients, including both gross evaluation and either dipstick or microscopic analysis. Hematuria should alert one to genitourinary injury, though the degree of hematuria does not always correlate well with the severity of renal injury, especially with penetrating and hilar injuries.13 Serum creatinine at the time of trauma is rarely helpful as it generally reflects serum creatinine before injury. However, elevated creatinine may indicate preexisting renal pathology which has been cited as a risk factor for renal injury in the event of trauma.14
Imaging. The gold-standard imaging modality for genitourinary trauma in the hemodynamically stable patient is an IV contrast CT scan with both arterial and excretory phases (10 minutes after initial injection) (Fig. 29.3).15 The excretory phase can be eliminated if no renal pathology is seen on the arterial phase, but is helpful in diagnosing the collecting system and ureteral injuries. Understanding which patients should undergo imaging is critical in the proper management of renal trauma and in general, all trauma patients with gross hematuria should be imaged with a CT scan. In blunt trauma patients with microscopic hematuria (>3RBCs/hpf) only, imaging can be reserved for adults who are unstable (systolic BP < 90) and in children with >50 RBCs/hpf, as major genitourinary injury has been found in only 0.2% and 2% of these patients, respectively.16
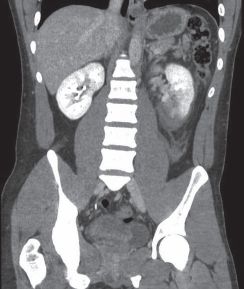
FIGURE 29.3. Grade IV renal trauma. (From Dr. Jack McAninch, with permission).
There are other less ideal imaging modalities including ultrasound, which in skilled hands can diagnose perinephric fluid collections but generally not the severity of renal injury.17 Renal angiography is unnecessarily invasive to diagnose renal trauma in the era of CT scan, but can be used in conjunction with angioembolization when used to treat hemorrhage.18 IVP can be especially useful in the setting of unstable patients, where renal injury is suspected, but imaging is not obtained prior to laparotomy. A single, on-table abdominal plain-film 10 minutes after a rapid bolus of contrast (2 mL/kg) can rule out most major renal injuries if found to be normal.19
Injury Classification. The American Association for the Surgery of Trauma (AAST) grading system for renal trauma, which has been recently modified (Table 29.1; Fig. 29.4), has been validated as a predictor of both injury severity and negative patient outcomes in large retrospective studies.4,20 It relies on a properly performed CT scan for accurate grading and staging. Most grade I-III injuries can be managed conservatively. With the new grading modifications, many grade IV injuries can also be initially managed nonoperatively, whereas, nearly all grade V injuries will require intervention.4,20,21
TABLE 29.1
AAST GRADING SYSTEM
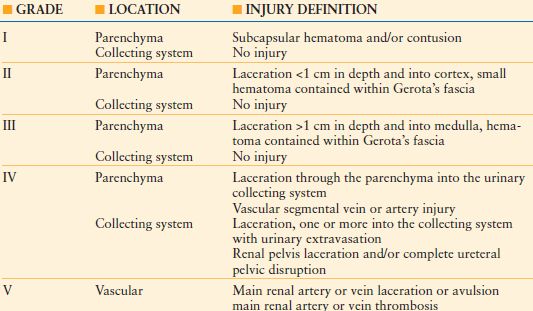
From Buckley JC, McAninch JW. Revision of current american association for the surgery of trauma renal injury grading system. J Trauma 2011;70(1): 35–37.
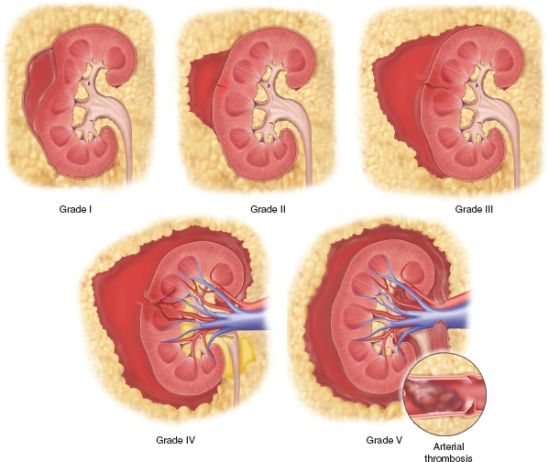
FIGURE 29.4. Modified AAST renal trauma grading system.
Management
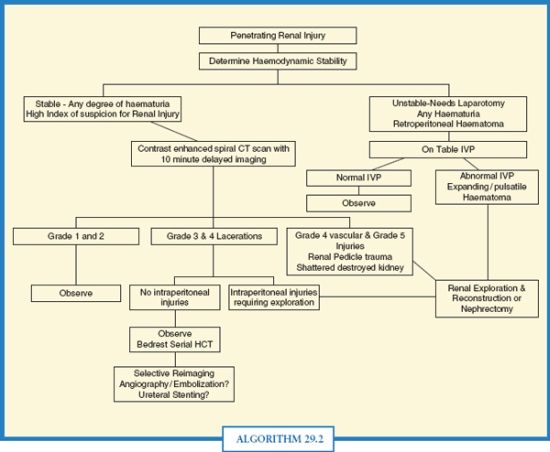
Conservative Renal Management. Directed conservative management is the mainstay of most contemporary renal trauma management algorithms (Algorithms. 29.1 and 29.2). While historically penetrating trauma to the kidney from gunshot and stab wounds resulted in renal exploration, it is no longer an absolute indicator for surgery with the advent of modern imaging techniques allowing for more accurate staging.2 The protected retroperitoneal location of the kidney and its enveloping by Gerota’s fascia will often be sufficient to tamponade renal bleeding.8 Many conservative protocols include serial hematocrit concentration and bed rest for 24–48 hours, though these have never been rigorously validated.16 Repeat imaging is also recommended for conservatively managed grade III-V injuries and for those patients with worsening clinical findings and/or Hct concentration as late bleeds can occur in up to 25% of patients.22
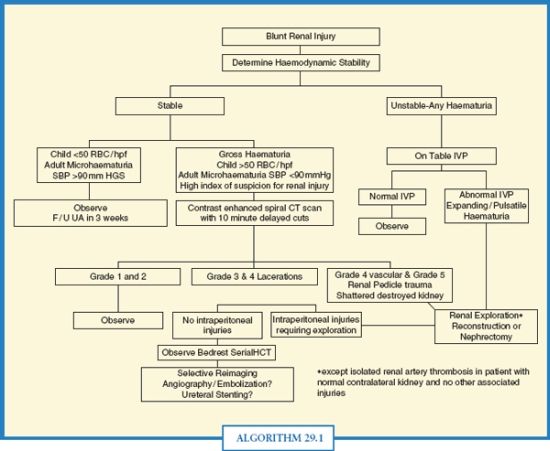
ALGORITHM 29.1 Blunt Renal Trauma Management algorithm. (From Santucci R, Wessels H, Bartsch G, et al. Evaluation and management of renal injuries: consensus statement of the renal trauma subcommittee. BJU Int. 2004;93(7): 937–954.)
ALGORITHM 29.2 Penetrating Renal Trauma algorithm. (From Santucci R, Wessels H, Bartsch G, et al. Evaluation and management of renal injuries: consensus statement of the renal trauma subcommittee. BJU Int. 2004;93(7): 937–954.)
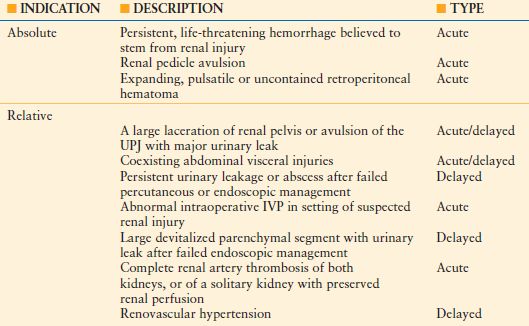
Surgical Management. Absolute indications for surgical management are few (Table 29.2), but prompt recognition is important as renal hemorrhage can be life threatening. The surgical approach to the damaged kidney is complicated and controversial. We have found that control of the renal vasculature prior to opening Gerota’s fascia can decrease the likelihood of nephrectomy and make any subsequent renal surgery more controlled as bleeding can be managed prospectively, though others have disagreed with these findings.2,23–25
TABLE 29.2
INDICATIONS FOR RENAL EXPLORATION
The initial surgical approach after laparotomy when vascular control is obtained, begins with identification of the aorta, where an incision of the posterior peritoneum is then made superior to the inferior mesenteric artery, gaining access to the retroperitoneum. Extension of the incision superiorly will lead to the left renal vein, which is the key anatomical landmark. The right renal artery can be found superior and medial to the left renal vein, often located with cephalad retraction of the vein and dissection between the aorta and inferior vena cava. The left renal artery lies just posterior and superior to the left renal vein. The right renal vein can be found on the opposite the left renal vein on the contralateral side of the IVC. Once the vessels are isolated, vessels loops are placed, but not occluded. The colon ipsilateral to the injury is then retracted medially and Gerota’s fascia is opened. If uncontrollable bleeding is encountered, the vessels are then occluded by the vessel loops, starting with the respective renal artery and followed by the renal vein if necessary23 (Fig. 29.5).
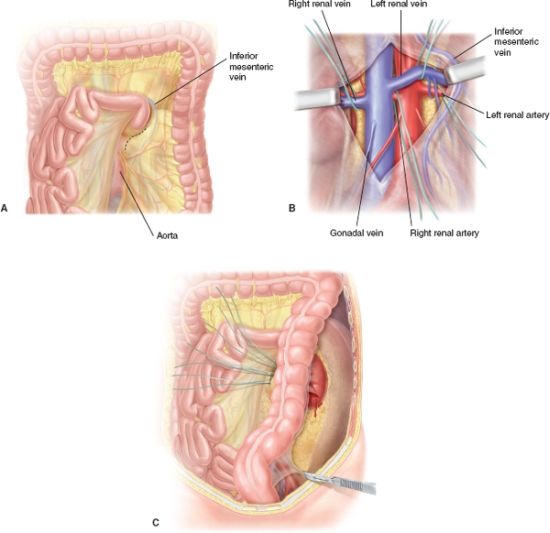
FIGURE 29.5. Surgical Approach to obtaining Hilar Control.
Renorrhaphy should be attempted for renal parenchymal injuries if possible (Fig. 29.6). All nonviable tissue should first be removed sharply. If greater than two-third of the kidney is nonviable, a nephrectomy should be strongly considered. Any bleeding parenchymal vessels should then be suture ligated with 4-0 chromic suture and any collecting system lacerations with a watertight running 4-0 chromic. Adequate collecting system closure can be confirmed by injection of methylene blue into the renal pelvis.26
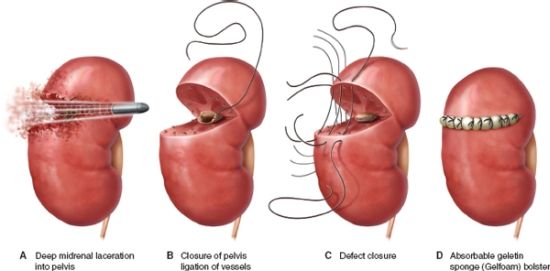
FIGURE 29.6. Renorrhaphy technique.
Coverage of the repaired parenchymal bed is essential. If the renal capsule is still present, it can be used for coverage. Alternatively, coverage with off-the-shelf agents, such as Gelfoam, has been shown to assist with both parenchymal hemostasis and wound compression.27,28 Bolsters made from these materials are secured to the remaining capsule with carefully placed 3-0 monofilament sutures. Additional coverage can be achieved with omentum, perinephric fat, and peritoneal flaps as needed.
Renal vascular injuries that require surgical intervention can be managed with the same initial operative approach. Incomplete renal arterial injuries can be repaired primarily with fine interrupted monofilament suture. Complete disruptions will often require nephrectomy, but if it’s clinically necessary to attempt repair, arterial debridement and thrombectomy are usually required before the reanastomosis is attempted. In cases where a tension-free anastomosis is not possible, interposition with the hypogastric artery is preferred over the saphenous vein.23,29
Renal vein injuries are often more difficult to diagnose and to treat. Venous tears can be repaired primarily, but complete disruptions generally lead to nephrectomy. With left renal vein injuries near the IVC, ligation of the vein does not necessitate nephrectomy if collateral venous drainage provided by the adrenal, gonadal, and lumbar veins remains intact.30
Relative indications for surgical exploration of the kidney are shown in Table 29.2. If the retroperitoneum is incompletely staged and a large hematoma is noted at the time of surgery, an IVP should be obtained with abnormalities dictating exploration.31 Repairing the kidney when concomitant abdominal visceral injuries are present can minimize complications such as postoperative infection and fistula.32,33 With large devitalized segments present, exploration and removal of the segments may minimize postoperative abscesses, urinomas, and late hemorrhage.34 Late or persistent bleeds may also require renal exploration, though angioembolization is being utilized at trauma centers more often with initial outcomes comparable to surgery.18 Urinomas seen on CT scan will generally resolve spontaneously, but may require late percutaneous or endoscopic procedures, and rarely open surgery.35
Interventional Radiology. In patients with major renal injuries who are not undergoing laparotomy for other concomitant injuries, persistent renal bleeding that has failed conservative management (persistent bleeding requiring transfusion) may be managed with angioembolization of the kidney.36 Early outcomes with this approach have been favorable, but failures do occur and open surgical management must always be considered if embolization fails to control bleeding.
Complications of Renal Injury and Management. Secondary hemorrhage and arteriovenous fistula formation in conservatively managed renal injuries is more common with deeper and higher-grade lesions, with rates of late bleeds in grade III and IV lesions between 13% and 25%.37 Most of these bleeds can be managed successfully with angiographic embolization. Late bleeds have been reported up to 1 month after the initial injury which may correspond to the timing of retroperitoneal hematoma resolution, exposing a previously tamponaded artery.38 Presentation is generally flank pain and/or hematuria or in the setting of an arteriovenous fistula, new onset hypertension.
Urinary extravasation from UPJ injury or from calyceal injury from a devitalized segment can successfully be managed with ureteral stent and/or percutaneous drain placement in >90% of cases, but may require open repair if a large devitalized renal segment is preventing healing or if leakage persists.35 Abscesses associated with these leaks can be usually managed with percutaneous drainage alone.
New onset hypertension is noted in 5% of patients with conservatively managed renal trauma, with higher rates (40%-50%) in individuals with severe renal arterial injuries.39 The mechanism is thought to be from renal ischemia and inappropriate renin release. Nephrectomy is the most common and most effective treatment. Renal insufficiency after conservative management has not been well studied, but angioembolization of renal hemorrhage leads to a 10% ipsilateral renal function and it is thought that some loss of function should be expected, especially with severe injury.40
Summary. With the advent of improved imaging techniques, outcomes data and grading criteria, the contemporary management of renal trauma has become mostly nonoperative. Grade V injuries and unstable patients will require surgery most often and in instances where the kidney must be explored, appropriate surgical techniques can lead to preservation of renal parenchyma in many cases. Prompt recognition of potential renal injuries followed by appropriate laboratory studies and imaging techniques can decrease renal trauma morbidity and mortality considerably.
URETERAL TRAUMA
Epidemiology
Ureteral injuries from external trauma are rare, accounting for <1% of urologic trauma, likely due to their small size, mobility, and relatively protected location in the retroperitoneum.41 They are infrequently subject to injury from external blunt trauma, with the exception of UPJ deceleration injuries, which are more common in children.42 When the ureter is injured from penetrating trauma, it is frequently associated with other abdominal injuries which can make them difficult to diagnose since the other injuries will often take diagnostic and management precedent.43
Most ureteral trauma experience comes from iatrogenic injury, usually encountered during difficult pelvic or ureteroscopic stone surgery, occurring at rates of 0.05%-30% depending on the type and difficulty of surgery being performed.44 The most common types of iatrogenic injury are suture ligation, crush injury, and ureteral devascularization from aggressive ureteral skeletonization. Gynecologic surgery accounts for over half of injuries, with the remainder occurring during urologic, colorectal, general, and vascular surgery. Iatrogenic injuries can be prevented with good exposure and a thorough understanding of surgical anatomy. Preoperative imaging45 and ureteral stenting have not been shown to decrease injury rate, but may make identification of the injury and subsequent repair easier.46
Diagnosis
Presentation. Early signs and symptoms of ureteral trauma are generally vague and nonspecific and include flank pain and hematuria. However, hematuria can be absent in up to 30% of cases and therefore, a high index of suspicion must be present whenever there is concern for a ureteral injury if an accurate diagnosis is to be made.41 The surgical field/anatomy, mechanism of injury, and path of the external trauma must be scrutinized with a low threshold to image and/or explore the ureter if injury is suspected.
Unfortunately, many ureteral injuries will present in a delayed fashion (65%-93%), often with symptoms such as prolonged ileus, low urine output, flank/abdominal pain, acute renal failure, or high drain output.47 Morbidity from ureteral trauma is significantly higher when the diagnosis is delayed, resulting in higher rates of urinoma, infection, and renal unit loss.48
Imaging. With penetrating trauma, the best imaging modality to diagnose ureteral injury is a CT scan with delayed images obtained 10 minute after injection of IV contrast dye (Fig. 29.7). Delayed extravasation of contrast medial to the kidney is common for UPJ injuries and more distal extravasation for ureteral injuries. Ureteral injuries may also show hydronephrosis, delayed nephrograms, and contrast absent in the distal ureter. A complete IVP will also accurately diagnose most injuries, though this is rarely used anymore in the acute setting.49 When a laparotomy is being performed without preoperative imaging and ureteral injury is suspected, a one-shot IVP can be utilized, which has high test specificity. However, the sensitivity is unacceptably low to rule out injury (20%-30%) and in these cases surgical exploration is probably the best way to diagnose injury, which can be improved by injection of intravenous methylene blue and inspection of the surgical field for dye extravasation. Retrograde pyelograms are both sensitive and specific but are logistically difficult to perform in the trauma setting and best used for diagnosing iatrogenic or delayed ureteral injuries or in the setting where IVP or CT scan results are equivocal.
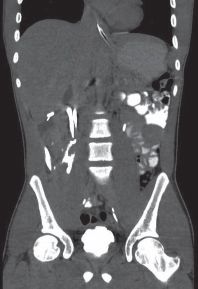
FIGURE 29.7. CT scan showing ureteral trauma on excretory images.
Treatment (Algorithm. 29.3)
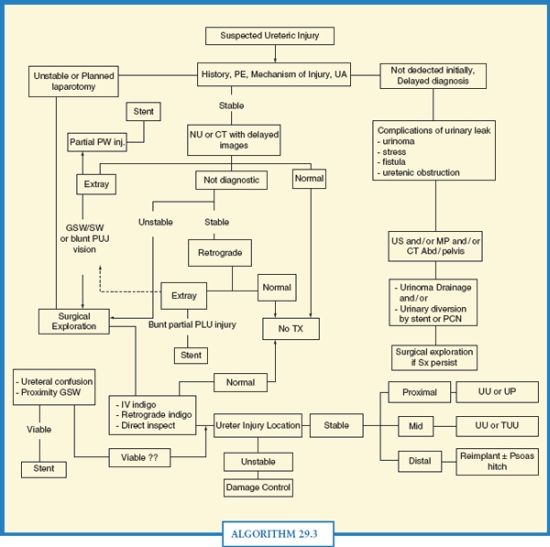
ALGORITHM 29.3 Ureteral Trauma algorithm. (From Brandes S, Chelsky M, Armenakas N, McAninch J. Diagnosis and management of ureteric injury: an evidence based analysis. BJU Int. 2004;94(3): 277–289.
ENDOSCOPIC MANAGEMENT
Endoscopic management with a ureteral stent can be utilized in patients with incomplete injuries, including those in the UPJ, that are not otherwise undergoing surgical exploration. In patients with delayed presentation of iatrogenic injuries after surgery, placing a ureteral stent is a reasonable first option as these injuries are often caused by inadvertent stitch placement that may dissolve with time relieving the obstruction.43 Outcomes of partial ureteral and UPJ injuries managed with stenting alone are excellent, with open intervention required rarely.
SURGICAL MANAGEMENT
Most penetrating injuries will be diagnosed during surgical exploration. Repair options are generally dictated by the patient’s overall clinical picture, but in general, the ureter should be repaired in the same operative setting. The type of repair is dependent on both the mechanism and location of the injury. Gunshot injuries will often be associated with other abdominal injuries, but these should never preclude ureteral repair in the stable patient. Careful attention must be paid to the path of the bullet and any concern for injury to the ureter warrants exploration of the retroperitoneum with careful attention to the blast cavity. Any discoloration of the ureter may indicate devascularization injury and would warrant surgical repair as late leaks are common.44
Principles of a good ureteral repair are the same regardless of location and include careful mobilization of the ureter with adventia sparing so not to devascularize the segment, aggressive debridement of the damaged ureter until healthy, bleeding ends are encountered, and, finally, a stented, tension-free watertight anastomosis.
Proximal ureteral injuries are best managed with excision of the injured segment and reanastomosis with either the healthy proximal ureter (ipsilateral ureteroureterostomy, IUU) or the renal pelvis. Mid-ureteral injuries can be managed with an IUU if the distal segment is healthy. However, in cases where the distal segment is unreliable or damaged, the ureter can be anastomosed to the contralateral ureter (transureteroureterostomy) or a Boari flap (tabularized bladder flap) can be created. Distal ureteral injuries should be managed with reimplantation since the distal blood supply is less reliable after injury. If the distance from the injury to the bladder cannot be bridged without tension, a psoas hitch can be utilized. Additional options for longer-segment injuries include ileal interposition and autotransplantation, though these are seldom utilized in the acute traumatic setting. Outcomes for ureteral injuries of all kinds are excellent if the above-mentioned principles are followed, though comparison outcomes studies are lacking.
With ureteral injuries in traumatic situations, a damage control approach to the injury should always be considered. Suture ligation of the ureter proximal to the injury with subsequent percutaneous nephrostomy tube is a reasonable option in the unstable patient and is much preferable to leaving the ureter drain into the surgical cavity. If the patient stabilizes, delayed repair can then be performed with improved outcomes.
Conclusion. Ureteral trauma is rare and will most often be encountered after iatrogenic injury. Early diagnosis is key to successful management, though this can often be difficult in a traumatic situation. Maintaining a high index of suspicion followed by appropriate imaging and intraoperative techniques can minimize morbidity from injury. Surgical repair of ureteral injuries is generally straightforward and often successful if proper repair principles are followed.
BLADDER TRAUMA
Epidemiology
Traumatic bladder injury is a result of blunt trauma 65%-85% of the time.50 Nearly 2% of blunt abdominal trauma will injure the bladder, with 80% of these a result of pelvic fracture.51 Of all pelvic fractures, 5%-10% will suffer a major bladder injury.50,52Penetrating trauma is less common, with bladder injuries reported in 3.6% of abdominal gunshot wounds. Iatrogenic injury to the bladder occurs in 0.1%-10% of all pelvic cases, with increasing complexity of cases leading to higher rates of injury.53
Pathophysiology
The most common cause of blunt bladder trauma is motor vehicle accident (90%), either from a direct blow to the bladder, most commonly by the steering wheel or lap belt, or in the setting of a pelvic fracture.53 Driving while intoxicated is an independent risk factor for bladder injury, as it predisposes to both MVAs and full bladders.54
When pelvic fractures lead to bladder injury, they are generally located at the fascial attachments of the bladder to pelvis, with pubic symphysis diastasis (RR 9.8) and obturator ring fractures (RR 3.2) being the most predictive fracture patterns for bladder injury.55 Fractures in other locations can lead to bladder injury when fragments secondarily penetrate the bladder.56 Bladder injuries from pelvic fracture are associated with urethral disruption in up to 15% of cases.57 Direct blows to the bladder from external trauma lead to high intravesical pressures and ruptures are generally found at the dome of the bladder, generally the weakest location.
Penetrating trauma to the bladder is most often a result of gunshot or stab wounds. These will rarely be isolated injuries and will many times lead to multiple vesicotomies.58
Initial Evaluation
Physical Exam. The most common signs and symptoms of bladder trauma are hematuria (80%-100%) and abdominal pain (62%).53 With direct trauma, bruising may be seen on the anterior abdominal wall, and urine extravasation may also be noted as perineal, scrotal, thigh, and abdominal wall edema and swelling.58 In patients with a delayed diagnosis, symptoms may include low urine output or prolonged ileus.
Laboratory. A urinalysis should be obtained in all trauma patients, and hematuria should alert one to the possibility of genitourinary injury. Gross hematuria in the setting of pelvic fracture should always raise the suspicion of bladder and/or urethral injury. Bladder injuries that are recognized in a delayed fashion may present with elevated Cr levels secondary to systemic absorption of urine or prolonged ileus after injury.
Imaging. Correct imaging is the single most important factor in guiding appropriate management of bladder injury. If blood is seen at the urethral meatus, begin with a retrograde urethrogram to rule out concomitant urethral injury. A catheter should then be placed when appropriate and used to perform either a static or CT cystogram. If a CT scan is already being performed, CT cystogram is usually the most appropriate study. Distention of the bladder with contrast is important, and a minimum of 350 mL of contrast should be instilled to improve diagnostic sensitivity, which when performed appropriately, is over 95%.59 Clamping the catheter during CT scan with IV contrast is not an appropriate alternative and if <350 mL is used, clot or peritoneal contents, which nearly always initially fill the cystotomy, may not be sufficiently displaced and injuries will be missed.58 Static cystograms will always require AP, lateral and excretory images. CT cystograms will require only pelvic imaging after the bladder is filled, though excretory images may help delineate the location of injury.60
Injury Classification. Injuries are most commonly separated into extra- and intraperitoneal, with combined injuries present in up to 5%.53 Extraperitoneal ruptures will show contrast extravasation generally confined to perivesical soft tissues, often in a “flare” pattern (Fig. 29.8). Intraperitoneal ruptures will show contrast extravasating into the cul-de-sac, outlining loops of bowel and if large enough, extend to other abdominal viscera such as the spleen (Fig. 29.9). Of blunt injuries, approximately 40% will be intraperitoneal and 60% extraperitoneal. Most penetrating injuries to the bladder will have an intraperitoneal component and concomitant abdominal visceral injuries.61 Bladder neck injuries, which are most often associated with pelvic fractures and extraperitoneal injuries, should be carefully looked for as well as these can dramatically change management and outcomes.62 Medial and inferior contrast extravasation is commonly seen with injuries of the bladder neck.
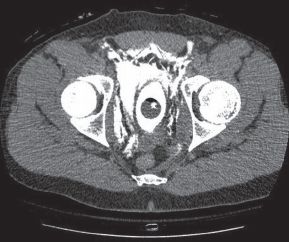
FIGURE 29.8. CT scan showing extraperitoneal bladder injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree