CHAPTER 108
Extensor Tendon Avulsion—Distal Phalanx
(Baseball or Mallet Finger)
Presentation
There is a history of a sudden resisted flexion of the distal interphalangeal (DIP) joint, such as when the finger tip is struck by a ball or jammed against a stationary object, resulting in pain and tenderness over the dorsum of the base of the distal phalanx. This injury can occur with relatively minor trauma (such as jamming a finger while reaching for a light switch in the dark) or even as a result of a direct blow to the dorsum of the finger. It may or may not be accompanied by swelling and ecchymosis over the DIP joint. When the finger is at rest or held in extension, the injured DIP joint remains in slight or moderate flexion (Figure 108-1).
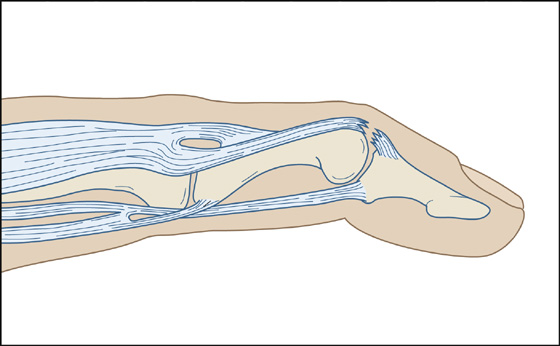
Figure 108-1 Injured distal interphalangeal joint in slight flexion.
What To Do:
 Obtain a radiograph with anteroposterior and lateral views, which may or may not demonstrate an avulsion fracture. The lateral view will allow visualization of a bony avulsion at the dorsal base of the distal phalanx (Figure 108-2).
Obtain a radiograph with anteroposterior and lateral views, which may or may not demonstrate an avulsion fracture. The lateral view will allow visualization of a bony avulsion at the dorsal base of the distal phalanx (Figure 108-2).

Figure 108-2 Radiograph showing avulsion fracture. (Adapted from Raby N, Berman L, de Lacey G: Accident and emergency radiology. Philadelphia, 2005, WB Saunders.)
 Test for stability of the collateral ligaments of the DIP joint with varus and valgus stress.
Test for stability of the collateral ligaments of the DIP joint with varus and valgus stress.
 While stabilizing the metacarpophalangeal (MCP) and the proximal interphalangeal joint (PIP) in extension, ask the patient to extend the DIP joint. There should be a loss of full active extension while active flexion and passive range of motion remain intact.
While stabilizing the metacarpophalangeal (MCP) and the proximal interphalangeal joint (PIP) in extension, ask the patient to extend the DIP joint. There should be a loss of full active extension while active flexion and passive range of motion remain intact.
 If the avulsion fragment is small or there is no bone involvement, nonoperative treatment is preferred. Apply a finger splint that will hold the DIP joint in neutral position or slight hyperextension and gently secure it in place with tape. Either a dorsal or a volar splint of aluminum and foam may be used. Plastic fingertip splints are manufactured in various sizes (e.g., Stax extension splints) (Figures 108-3 to 108-5).
If the avulsion fragment is small or there is no bone involvement, nonoperative treatment is preferred. Apply a finger splint that will hold the DIP joint in neutral position or slight hyperextension and gently secure it in place with tape. Either a dorsal or a volar splint of aluminum and foam may be used. Plastic fingertip splints are manufactured in various sizes (e.g., Stax extension splints) (Figures 108-3 to 108-5).
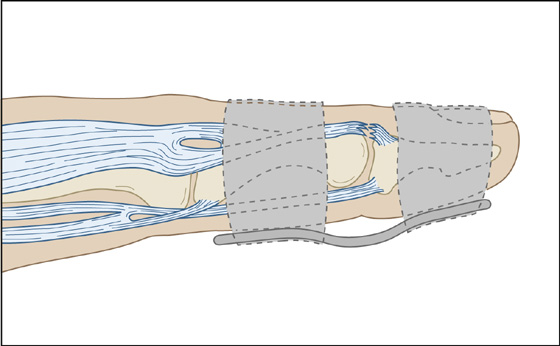
Figure 108-3 Commercial concave aluminum splint.
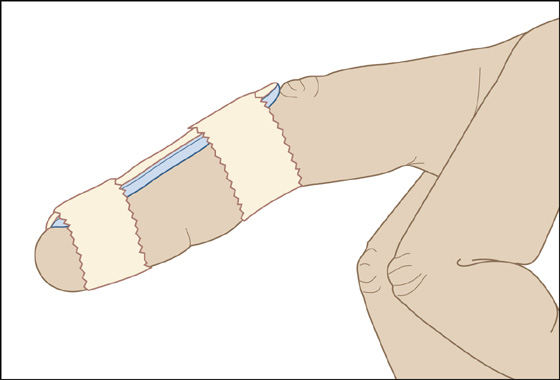
Figure 108-4 Dorsal aluminum splint.
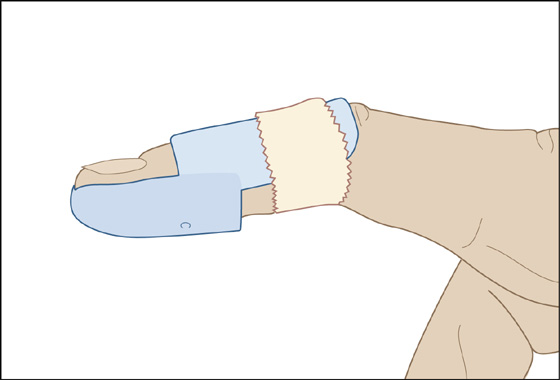
Figure 108-5 Commercial Stax extension splint.
 Instruct the patient to keep the DIP joint in full extension continuously and seek hand specialist or orthopedic follow-up care within 1 week.
Instruct the patient to keep the DIP joint in full extension continuously and seek hand specialist or orthopedic follow-up care within 1 week.
 Closed mallet fingers should be immobilized in extension full time for 8 weeks. Patients must understand that if they take the finger out to wash or air it out, they cannot let the DIP joint fall into flexion. Each time the DIP joint flexes, the treatment clock starts over again at time zero.
Closed mallet fingers should be immobilized in extension full time for 8 weeks. Patients must understand that if they take the finger out to wash or air it out, they cannot let the DIP joint fall into flexion. Each time the DIP joint flexes, the treatment clock starts over again at time zero.
 Skin breakdown can be a significant problem, and patients should be instructed to remove the splint daily while holding the joint in extension, resting the joint on a flat surface to allow the skin to dry and reduce the chance of maceration. One splint that is well tolerated and can be left on continuously (but is moderately expensive and somewhat difficult to learn how to mold) is the MEALS splint (George Tiemann & Co., Hauppauge, N.Y.).
Skin breakdown can be a significant problem, and patients should be instructed to remove the splint daily while holding the joint in extension, resting the joint on a flat surface to allow the skin to dry and reduce the chance of maceration. One splint that is well tolerated and can be left on continuously (but is moderately expensive and somewhat difficult to learn how to mold) is the MEALS splint (George Tiemann & Co., Hauppauge, N.Y.).
 An additional 6 weeks of splinting can follow if there is not a full ability to extend against resistance. After full active DIP extension is achieved, a gradual withdrawal of the splint can be instituted, with wearing of the splint only at night and with sports for another 6 weeks. Participation in sports is acceptable so long as the DIP joint is firmly immobilized in extension and is protected against further injury.
An additional 6 weeks of splinting can follow if there is not a full ability to extend against resistance. After full active DIP extension is achieved, a gradual withdrawal of the splint can be instituted, with wearing of the splint only at night and with sports for another 6 weeks. Participation in sports is acceptable so long as the DIP joint is firmly immobilized in extension and is protected against further injury.
 Prescribe an analgesic as needed.
Prescribe an analgesic as needed.
 Surgery is recommended for displaced avulsion fractures with a large articular component (more than 50% of the articular surface), volar subluxation of the distal phalanx, or failure of splinting.
Surgery is recommended for displaced avulsion fractures with a large articular component (more than 50% of the articular surface), volar subluxation of the distal phalanx, or failure of splinting.
What Not To Do:
 Do not assume that there is no significant injury if the radiograph is negative. The clue to this injury is persistent drooping of the distal phalanx and tenderness over the bony insertion of the extensor tendon. With or without a fracture, the tendon avulsion requires splinting.
Do not assume that there is no significant injury if the radiograph is negative. The clue to this injury is persistent drooping of the distal phalanx and tenderness over the bony insertion of the extensor tendon. With or without a fracture, the tendon avulsion requires splinting.
 Do not forcefully hyperextend the joint beyond the point of skin blanch or pain. This can result in ischemia and dorsal skin necrosis over the joint.
Do not forcefully hyperextend the joint beyond the point of skin blanch or pain. This can result in ischemia and dorsal skin necrosis over the joint.
 Do not unnecessarily impair the movement of the PIP joint.
Do not unnecessarily impair the movement of the PIP joint.
Discussion
Mallet finger, also known as “baseball finger” or “drop finger,” involves disruption of the extensor tendon or an avulsion fracture of the distal phalanx. The classic mechanism involves a direct blow to the tip of the finger while the DIP joint is held in extension. Although this injury is commonly caused during participation in athletic activities (e.g., by contact with a baseball, volleyball, or basketball), mallet finger may occur with household activities, such as pushing off a sock or tucking in bed sheets. Given the mechanism, it makes sense that the middle finger, the longest one, is most commonly involved, although a mallet finger may involve any of the digits, including the thumb.
Swelling and tenderness may be found on the dorsum of the DIP joint, but commonly the injury is painless, and the loss of extension may not appear for several days to weeks.
Patients may wait weeks to months before being seen and may present with a subsequent swan neck deformity. This is caused by the unopposed extensor mechanism on the middle phalanx leading to hyperextension of the PIP joint.
With a chronic mallet finger presentation without significant bone involvement, splinting in extension should still be attempted but must be done for anywhere from 2 to 3 months.
Many splints are commercially available for splinting this injury (e.g., Stax hyperextension splints, padded aluminum, and frog splints), but, in a pinch, a paper clip will do (Figure 108-6). A dorsal splint allows more use of the finger but requires more padding and may contribute to ischemia of the skin overlying the DIP joint. Figure-of-eight taping can also provide some limitation of flexion. A Cochrane review looking at interventions for treating mallet finger injuries found insufficient evidence to establish the effectiveness of different finger splints in determining when surgery is indicated. The MEAL splint noted earlier must be heated in hot water in a nonstick container before it can be molded and stretched to fit the finger. It is very comfortable for the patient, has no absorbent surfaces, and can be worn after washing without having to remove it to prevent skin maceration. (Patients have to be warned that the MEAL splint may slide off when they are showering.)
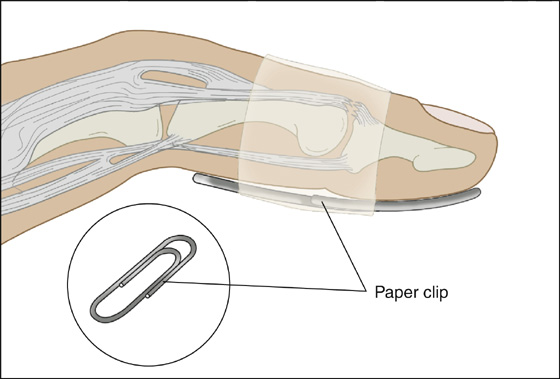
Figure 108-6 Paper-clip splint.
Mallet thumb can be treated similarly to mallet finger, with a trial of splinting in extension; however, because larger forces are required to cause mallet thumb, consider earlier surgical intervention than with the same injury in a triphalangeal digit.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



