I. INTRODUCTION
In caring for critically ill patients, it is inevitable that ethical issues will arise. Patients often have complex medical conditions, multiple providers, and uncertain prognosis or treatment plans. This can lead to conflict and moral distress among patients, family, health care providers, and support staff. We describe a proactive approach to ethical issues in the ICU. Adoption and adaptation of these measures may help minimize conflict and moral distress. Key ethical concepts and practical guidelines are provided in order to optimize care in a variety of circumstances in which ethical tensions may arise because of conflicts over values or decision-making authority. It is hoped that you will build trust and connect with your patients and their families through empathy, seeking to understand them, confronting (rather than avoiding) problems, managing expectations well, and providing optimal clinical care.
II. PROACTIVE APPROACH
A. A proactive approach to ethical issues in the ICU can minimize conflict and moral distress. Conflict is common in the ICU and is considered to be dangerous or harmful. Yet, 70% of conflicts are perceived to be preventable. Conflicts arise within teams and between staff and families. Disagreements regarding value-laden clinical decisions may be exacerbated by interpersonal tension, poor communication, mistrust, and difficult end-of-life care. The costs of unreconciled conflict are high and include misguided treatment, moral distress, staff burnout, and high job turnover. Such poor outcomes should be prevented with proactive measures designed to enhance collaborative shared decision making (see Table 42.1).
B. In these days of a heightened focus on organ systems, numbers, monitoring, and computer-based documentation, humanizing the ICU experience—for patients, family, and staff—can be challenging. Yet it is a worthy endeavor. Burnout, as mentioned above, is a consequence of unreconciled conflict. The characteristics of burnout include a detached or dehumanizing attitude and a lack of concern for others. But the essence of ethical care involves an engaged and person-focused attitude and an abundant concern for others (patients and staff). Measures to avoid burnout and promote personalized care should be taken, such as those listed in Table 42.1.
C. Another step we have taken in our ICUs is the use of Get to Know Me posters (Fig. 42.1). These 20 × 24 inch posters in the patient’s ICU rooms are filled in by the families as an opportunity for the team to get to know the patient better. The information provided by the family serves to connect the team to the (usually) voiceless patient. The interaction also helps the team develop rapport with and empathize with the family. ICU families are often under a great deal of stress—trying to maintain their home responsibilities and roles while adjusting to the ICU experience. Family members engage in multiple roles in the ICU: active presence, patient protector, facilitator, historian, coach, and caregiver. As team and family get to know each other, thus begins the process of substituted judgment: an aspect of shared decision making in which the surrogates speak the patient’s voice.
| Proactive Measures to Minimize Moral Distress and ICU Conflict | |
ICU open visitation hours
Allowing family presence during rounds
Routine proactive family meetings
Process of informed consent
Relieving patients’ distressing symptoms
Sensitivity to and respect for cultural norms
Provision of spiritual support
Interdisciplinary collaborative care
Team debriefings
Ethics rounds
ICU staff meetings
Ethics consultation
Integration of palliative care principles and practices into the ICU
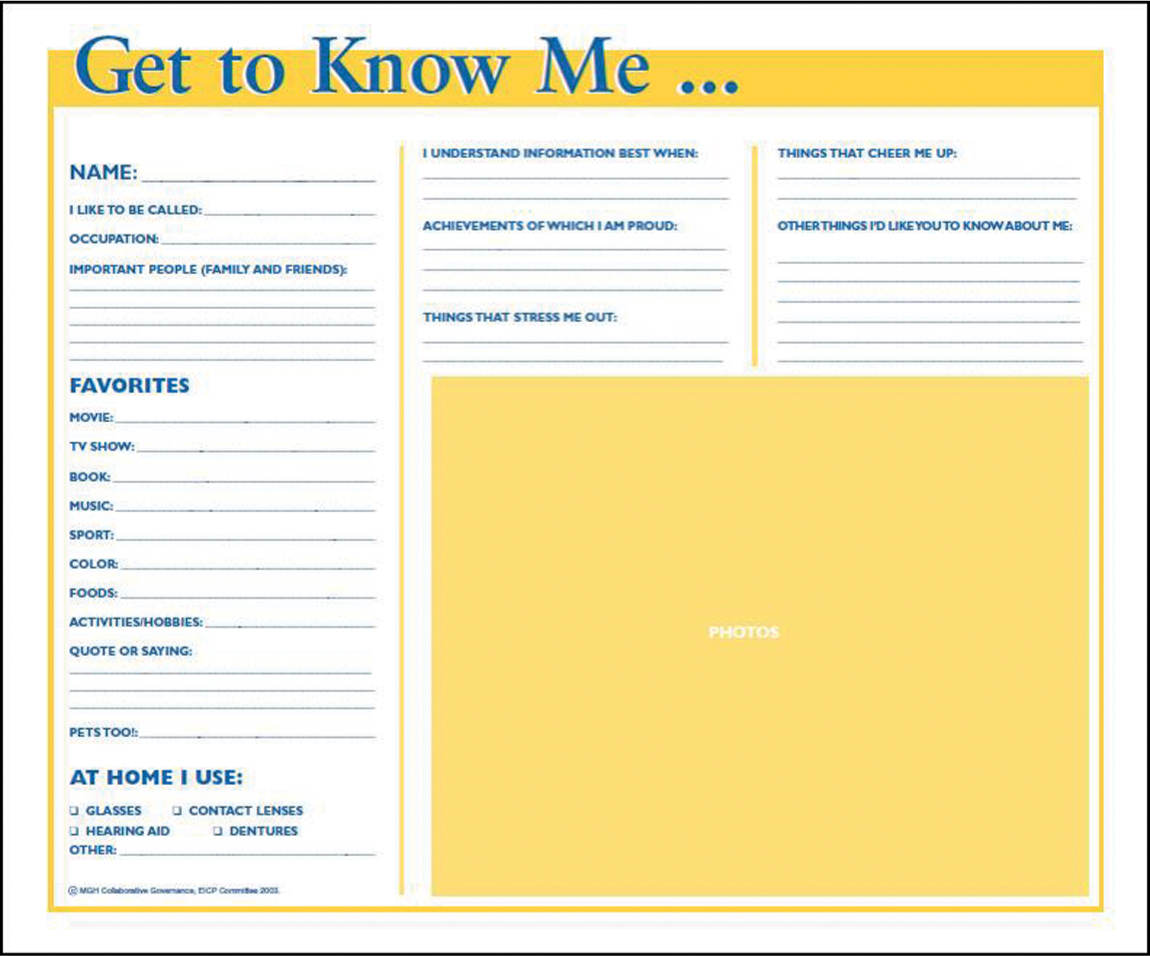
FIGURE 42.1 Get to Know Me Posters. These 20 × 24 inch posters in the patient’s ICU rooms are filled in by the families as an opportunity for the team to get to know the patient better.
D. Many ICUs are opening up visiting hours and allowing family to be present during ICU work rounds. Simple guidelines for making this work include inviting the family to rounds, making brief introductions, apologizing for medical jargon and offering to “translate” later, and inviting interruptions for errors; allow a short period for questions at the end of rounds and more private time later. The opportunity to observe the “work” of rounds and the transparency of communication help build trust and mutual respect. This also can increase the efficiency of communicating with families.
E. The structure and functioning of your ICU team may influence the prevalence of conflict in your ICU and how it is handled. How well do nurses, physicians, medical students, social workers, chaplains, physical and respiratory therapists, and other health professionals interact—among themselves and with families? Do you hold team debriefings after critical incidents, bad deaths, or great successes? Are work rounds interdisciplinary and collaborative? Do you hold ICU staff meetings and retreats to review educational content, your mission, and goals? Improving your ICU functioning is another means of optimizing the decision-making process that leads to optimal delivery of care.
III. TREATMENT DECISIONS
A. When there is conflict over value-laden clinical concerns, an optimal decision-making process is one that is fair, transparent, respectful, collaborative, and effective. Within some teams, there can be a diffusion of responsibility, such that the locus of decision-making authority becomes difficult to identify. In other teams, there might be a top-down authoritative approach in which some team or family members feel voiceless and powerless. Moral distress arises when persons feel powerless to alter what they perceive to be suboptimal care. And yet, regardless of the team structure, each member of the team is a moral agent and should possess some degree of moral accountability for the decisions made and actions taken. A shared decision-making paradigm locates the responsibility between the patient (or surrogate) and the clinicians, thus aiming to respect patient autonomy and the beneficent intentions of caregivers.
B. Communication is the key to the shared decision-making process. Good communication allows the clinicians to learn about the patient’s values and goals and allows the patient/surrogate to learn about the clinical condition and which interventions are considered reasonable to use (after review of the patient’s values and goals). The process is dynamic and allows for reassessment and adjustment of plans, on the basis of the patient’s evolving condition and goals. The attending physician has the ultimate responsibility in deciding on a reasonable clinical plan.
C. Key ethical tenets come into play on a daily basis in the ICU. These include
1. Autonomy—the right to self-govern
2. Beneficence—the obligation to promote good and prevent/remove harm
3. Nonmaleficence—the need to refrain from inflicting harm
4. Justice—an allocation principle, striving for fair distribution of resources
D. Patient autonomy, the respect for an individual patient’s right to make decisions about his or her own medical care, is a highly valued ethical principal in the United States. Ideally, autonomy is preserved by involving the patient in the decision-making process.
E. Informed consent preserves patient autonomy and is an ethical responsibility of the treating physician. The process of informed consent involves a dialogue between patient and health care provider(s) describing the risks/benefits of the proposed intervention as well as the pertinent alternative treatment options. Informed consent should be obtained for most procedures, therapies, and research. There are certain situations in which the informed consent process can be waived. These include emergency situations, situations in which a patient or state waiver is in place, and situations in which the patient does not have the capacity to consent (and, no surrogate is available).
F. Competent patients are able to accept and refuse medical treatments. Competence is a legal term. Individuals above the age of 18 are presumed competent unless deemed incompetent by a court previously. Decision-making capacity is a medical term. If a patient’s capacity to make decisions is questioned, then a physician should evaluate the patient to determine their ability to receive and understand medical information, differentiate between options presented, and choose a course of action on the basis of the information offered.
G. In the ICU, patients often lack decision-making capacity due to illness or medication effects. In these situations a surrogate, typically a family member or health care agent, should make decisions under the principle of substituted judgment. The role of a surrogate is to make the decision that the patient would make in the given situation. This may differ from what the surrogate wants for the patient and even from what the surrogate would want for him- or herself in the same situation.
H. The patient may have prepared a document to help guide decision making in the case that the patient is unable to make decisions for him- or herself. For patients with chronic illness, discussions regarding advanced care planning should start in the outpatient setting, prior to ICU admission. This allows more time to assess the patient’s understanding of their illness, clarify goals and values, and discuss reasonable clinical goals.
1. An advanced directive is a statement specifying a patient’s wishes that is designed to help guide decision making in these situations. Advance directives vary from state to state and even from institution to institution. It has been recognized that advance directives may be verbal in nature and that conversations between the patient and their loved ones may provide an acceptable framework to guide decisions.
2. A health care proxy or durable power of attorney is a legal document prepared by the patient appointing the person they wish to make health care decisions in their place in case they are unable to make decisions themselves.
3. A living will is a document describing therapies or interventions that the patient would wish to receive or refuse under specific circumstances. These documents often cover broad circumstances such as “persistent vegetative state” or “without meaningful recovery” and often do not apply to the nuanced situations that arise in the context of complex critical illness. Thus, these documents are often only marginally helpful and must be supplemented by communication with those close to the patient.
I. In some cases, a surrogate decision maker cannot be located for a patient. In these situations, as much information about the patient should be gathered as possible from friends, family, colleagues, primary care providers, and so forth. The patient’s lifestyle and values should be taken into account to approximate a substituted judgment. In some cases, such as those where conflict has arisen regarding surrogacy, a legal guardian may be appointed to serve as a surrogate decision maker.
J. The need to perform life-saving procedures can often present suddenly in the intensive care unit, and obtaining informed consent from a surrogate may delay potential life-saving interventions. For this reason, some ICUs have implemented a bundled or universal consent form. These forms often include commonly performed procedures that may be urgent in nature such as intubation, central line placement, chest tube placement, blood transfusion, and the like.
1. This type of bundled consent can serve as efficient way to educate patients and surrogates at the beginning of an ICU stay. It can also serve as opportunity to begin discussions regarding patient wishes and goals in the context of their current illness.
2. However, it is possible that presenting such a complex picture early on in treatment may be overwhelming and confusing to patients and families. They may feel pressured to consent for fear that treatments will be withheld in the future.
IV. THE FAMILY MEETING
A. Family meetings are one of the most effective means to achieve shared decision making. They can also help prevent or manage conflict that arises around decision making. Think of the meeting as being like a procedure—with its own set of skills to master. There are organizational, communication, and emotional skills to muster in order to conduct an effective meeting. As with any procedure, preparation, performance, and follow-up are key components of the family meeting (see Table 42.2).
B. Preparation: Hold a premeeting staff “huddle” to assure consensus on facts; identify areas of uncertainty, conflict, or psychosocial concern; discuss agenda and goals; and identify suitable meeting facilitator, time, and location. Assure multidisciplinary staff participation (attending physician, nurse, possibly social work, chaplain, and others). Allow for adequate family/surrogate representation. Include the bedside nurse, since he or she spends the most time at the bedside and spends more time with visiting family members. He or she knows the patient’s burden of care best and can communicate to family the patient’s ups and downs. Since RNs cover 24/7, they can provide cross-shift communication of goals of care (GOC) and treatment plans.
| Guide to ICU Family Meetings | |
1. Prepare agenda and setting
Assure team consensus on facts
Decide who comes to the meeting and who leads the discussion
2. Introduce participants
3. Assess patient/family understanding of the patient’s prior and current circumstances and what they want to know
4. Summarize the patient’s medical condition and key clinical decisions
5. What is it like for the patient now?
6. What was the patient like?
What would the patient want in such circumstances = substituted judgment
7. Explore and address family fears and concerns
8. Frame recommendations
9. Plan for follow-up
10. Document meeting and communicate content to team
C. Introductions—of participants and the purpose of meeting: Invite individuals to give their name and relationship to the patient. Identify the patient’s surrogate spokesperson. Politely establish a tone of courtesy and confidentiality. Clarify the broad purpose of the meeting: to identify reasonable goals and plans aligned with the patient’s values, beliefs, and preferences.
D. Note, in particular, the order of steps 3 and 4 (as presented in Table 42.2): The family gets to provide their summary before the team launches into a clinical summary. This order (rather than the other way around) demonstrates respect for the patient’s preferences by giving the patient/family the first opportunity to describe the situation, helps establish rapport, allows the team to learn more about the patient’s illness trajectory and the family’s perspectives and values, and allows the team to discern what knowledge gaps they need to address. We all have different communication styles—team and family members alike—so, listening to the family first affords insight into how this family communicates and their relational dynamics.
E. Steps 5, 6, and 7 deepen the opportunities to learn about this patient, his or her condition, and his or her preferences under such circumstances. It is the surrogate’s privilege and responsibility to express the patient’s voice—the patient’s substituted judgment. Exploring the family’s fears and concerns uncovers opportunities to manage expectations and to provide psychosocial support for realistic hopes and fears—or to provide correction for unrealistic ones.
F. After these steps have unfolded, the leading clinician can then frame recommendations (step 8) on the basis of the clinical details and the patient’s values and goals. This might be introduced with the words, “In light of what we’ve discussed today, I recommend….” What follows is a recommendation based on the team’s clinical expertise in conjunction with its understanding of the patient’s goals and values. If the preceding steps have been taken, one need not ask the family to decide about each diagnostic or treatment option. Rather, one can propose a plan consistent with the goals and values and give family opportunity to concur with it. Recommend a treatment plan as a therapeutic time trial aimed at specific short-term goals. State how and when you will monitor success or failure of the time trial, and plan for follow-up discussions for further shared decision making. If appropriate, this might also be the point in the meeting to address code status. By this stage, the leading clinician is better equipped to make an informed recommendation of an appropriate code status.
G. Document the meeting in the record by writing a family meeting note—similar to writing a procedure note. Include who attended the meeting, what “the findings” were, what decisions and plans were made, justifications for those plans, what uncertainties or disagreements remained unreconciled, and plans for follow-up. Consider using a family meeting template to guide and document the meeting. Verbally communicate salient points to the ICU team.
H. The guidelines described above are designed to achieve shared decision making. Holding family meetings in the ICU within 72 hours of admission have been shown to increase family satisfaction, reduce the length of ICU stay, and increase the likelihood of agreement between the providers and the family about limitations of life-sustaining treatments. Family satisfaction is higher if physicians spend a smaller proportion of time talking and more listening. Additional tips on talking with ICU families are provided in Table 42.3—these apply in formal family meetings and in less formal communications. Despite these efforts, uncertainty and/or conflict may arise. Redoubling communication efforts may solve the problems; sometimes, however, teams may need to seek additional help at resolving conflicts. This is covered in the section on GOC.
| Talking with ICU Families | |
Communicate regularly, using family meetings prophylactically. Involve the staff, especially the nurses. Be aware of family members who are nonparticipants.
Listen, listen for family understanding, affect, and how they make decisions. Establish trust. Acknowledge emotions. Avoid jargon. Lecture less and let the family guide you to further topics.
Provide psychosocial and spiritual support. Offer hope, not false hope. Bad news is a shock. Use support from the team. Culture and religion play key roles.
Inform family regularly about goals of care and how we know if goals are met.
Convey uncertainty; avoid false certainty. Describe treatment as a therapeutic time trial aimed at specific short-term goals.
Care always continues, but treatments may be withdrawn or withheld. Avoid saying we are “withdrawing care.”
Don’t ask the family to decide about each diagnostic or treatment option; ask them what the patient would want and allow them to concur with a plan consistent with patient values.
V. GOALS OF CARE
A. Goals of ICU therapy may vary on the basis of clinical reasonableness and patient’s wishes and expectations. GOC should be discussed with the patient and/or the surrogate.
1. For some patients, the goals are obvious, such as preventing imminent death, curing acute disease, relieving pain and suffering, and returning to their premorbid level of function. In some situations, the goal may be to delay the disease process. In others, it may be to prolong life long enough to allow the arrival of close relatives to pay last respects.
B. When discussing GOC, it is important to elicit and emphasize the patient’s values.
C. After discussing the disease process and prognosis (see The Family Meeting section), the patient, a surrogate, or physician may propose a “do not resuscitate” (DNR), “do not attempt resuscitation” (DNAR), or “do not intubate” (DNI) order. The purpose of a code status is to clarify which therapies will be offered to the patient in the case of life-threatening instability. It is important to emphasize that DNR/DNAR/DNI orders do not automatically signify that a patient’s condition is hopeless and to reassure that interventions to treat underlying pathology and optimize health and quality of life will continue, consistent with the patient’s goals.
1. Along these lines, it is not unusual for patients who are DNR/DNI to undergo diagnostic or therapeutic procedures. The need to reverse the DNR or DNI should be decided on a case-by-case basis. Prior to any procedure, a discussion with the patient or surrogate and providers involved is necessary. The procedure should be discussed in the context of the patient’s current health status, values, and goals. For patients undergoing elective surgical procedures requiring intubation or during which a reversible cause of cardiac arrest, unrelated to their underlying illness, may occur, it may be in line with their GOC to temporarily hold the DNR/DNI order. For severely ill patients undergoing procedures in which resuscitation would be unlikely to be effective or produce a survival consistent with their goals, they may elect to keep the DNR in place.
2. Today, patients often have multiple medical providers involved in their care and may receive treatment in multiple locations. Some states have implemented programs that provide a framework to allow patients with serious advanced illnesses to express their preferences about life-sustaining medical treatments with the purpose of relaying this information between health care providers. These are specific documents known as Physician/Medical Orders for Life-Sustaining Treatment (POLST, MOLST) or Physician Order for Scope of Treatment (POST) forms. Unlike a health care proxy or advanced directive form, these are considered to be medical order forms and are filled out by a health care professional after discussions with the patient regarding prognosis, treatments, and GOC. If a patient lacks capacity, a health care agent may sign the form on the patient’s behalf. These forms can be particularly helpful in emergency situations, when the patient or health care proxy may not be immediately available to express the patient’s wishes.
3. Conflict may arise when a family wishes to continue intensive interventions or “want everything done” but the medical team believes that some interventions are no longer warranted—or should not be offered. Under such circumstances, it is important to explore what is meant by the patient and family when they say they want “everything.” They might not mean employ every life-prolonging intervention you can. They, like you, might want to avoid some burdensome and inefficacious treatments. Explore the nuances of their preferences and follow the steps outlined above in the section on family meetings.
4. Though there is no consensus on the precise definition of futility, clinicians often experience moral distress when they believe further intervention only serves to prolong the dying process, is ineffective, wasteful, or harmful. If open communication does not resolve the situation, then the clinician may (1) attempt to transfer the patient to another caregiver, (2) seek adjudication to replace or override the surrogate, or (3) involve institutional ethics and legal consultation to discuss limitations of life-sustaining treatment despite the wishes of the family. There might be a lower threshold to adjust a code status against family wishes than to actively withdraw life-sustaining treatments. The latter sort of decision should not be made solely by individual physicians but rather with the backing of additional critical care opinion(s), formal ethics consultation, and, preferably, with institutional policy support.
5. The institutional ethics committee is usually an interdisciplinary group of professionals trained in clinical ethics consultation. Ethics consultation offers an objective analysis of the patient’s care and, drawing upon ethical principles, employs a fair process to guide the patient, clinicians, and family to a reasonable consensus or compromise. Ethics interventions have been shown to mitigate conflict and, for some, to reduce ICU length of stay, ventilator days, hospital stay, and cost (without increasing mortality).
VI. PROVIDING PALLIATIVE CARE IN THE ICU—IT’S NOT JUST FOR END-OF-LIFE
A. ICU patients are at risk for suffering a number of unpleasant sensations during routine ICU care. Their underlying illnesses and the procedures we do to diagnose and treat them can be accompanied by pain, dyspnea, anxiety, delirium, agitation, nausea, vomiting, secretions, pruritis, diarrhea, constipation, and other physical and psycho-social-spiritual discomforts. Preventing and palliating these distressing symptoms are goals shared by critical care and palliative care clinicians—whether the patient is receiving life-prolonging care or end-of-life care. Sometimes, formal palliative care consultation is warranted in the ICU, not only when patients are dying. Palliative care interventions have been shown to reduce length of stay and to improve symptom control, communication, and the quality of dying in the ICU. Social service and chaplaincy interventions can be employed as part of or separately from palliative care consultation. Patients, families, and staff are greatly supported by these services, especially under the stressful circumstances of ICU and end-of-life care.
B. General management of sedation, analgesia, and delirium is covered in Chapter 7 of this handbook. Here, we address clinical and ethical concerns related to withdrawing life-sustaining therapies from patients who are expected to die.
C. Legal and ethical opinion have established that competent individuals may refuse life-sustaining therapies, or have them withdrawn once started; they have also established that surrogates can make such decisions for patients who lack decision-making capacity. The law has evolved over time, balancing the autonomous rights of patients and the state’s interest in preserving life. For surrogate decision making, states vary in their requirements of the level of evidence needed to discern the preferences of a previously competent person. So it is important to be familiar with your local legal standards.
D. Three ethical assumptions underlie the practice of forgoing life-sustaining treatment:
1. Withholding and withdrawing treatment are considered equivalent.
2. There is a difference between “killing” and “letting die.”
3. One is permitted to use medications to relieve suffering at the end of life—even if side effects of those medications might hasten death—as long as the intent of using the medications is to relieve suffering. For patients who are terminally ill, risking the foreseen, but unintended, consequence of hastening death is justified under the “doctrine of double effect.”
a. Although some controversy surrounds these assumptions, they have been guiding principles for clinical practice and U.S. legal thought regarding end-of-life care.
VII. GUIDELINES FOR WITHDRAWING LIFE-SUSTAINING THERAPIES (LSTs)
A. Goals for the withdrawal of LSTs include the following:
1. Promoting comfort and respecting the wishes of the patient:
a. Withdrawing burdensome therapies
b. Maintaining or achieving the patient’s ability to communicate, if possible
c. Preventing or palliating distressing symptoms
2. Supporting and respecting the family
a. Physically, emotionally, spiritually—within their cultural norms
3. Allowing death to occur
B. Your intensive focus now is the provision of comfort for this patient. All clinical orders should be reexamined with a goal toward palliative and comfort care. Consider consulting palliative care, particularly if care of the patient will continue outside the ICU. Reassess the equipment in the patient’s room and remove unnecessary items in order to make room for comfortable seating for family members. Minimize monitors (and their alarms). Therapies that increase patient comfort or relieve pain, anxiety, or agitation should be continued or added (Table 42.4). Therapies directed toward supporting physiologic homeostasis or treating the underlying disease process are no longer indicated and may be discontinued. These include many of the “routine” procedures and interventions associated with being an ICU patient (Table 42.5). The benefit-to-burden ratio of each intervention should be used to determine which interventions should be eliminated. The precise order of discontinuation is tailored to the patient’s situation and reasonable family preferences. Most commonly, a stepwise approach is followed, with mechanical ventilation discontinued after the withdrawal of vasopressors, antibiotics, or enteral feedings.
| Examples of Comfort and Palliative Measures in ICU | |
Continuation of general nursing care and cleanliness
Special clothing, blankets, stuffed animals
Offering of food/water to alert patients
Playing music
Nonpharmacologic sleep-promotion strategies
Control of oral secretions
Humidified air
Analgesics
Sedatives
Anticonvulsants
Antipyretics
Nonsteroidal anti-inflammatory drugs
Prophylaxis for gastrointestinal bleeding
Antiemetics
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







