Introduction
Defibrillation is the passage of sufficient electrical current across the heart to depolarise a critical mass of myocardium, preventing the continued propagation of the fibrillatory wave fronts and allowing the natural pacemaker in the heart to resume control of the cardiac rhythm. Following the onset of VF or VT, cardiac output ceases and cerebral hypoxic injury rapidly ensues. For recovery to be possible, defibrillation with the return of a spontaneous circulation (ROSC) must be achieved as soon as possible.
Untreated, VF decays into terminal asystole as cardiac energy sources become exhausted; this process can be slowed by effective CPR. The probability of successful defibrillation declines rapidly with time: for every minute that passes between collapse and attempted defibrillation, the chance of success declines by approximately 10%.
Defibrillators
All defibrillators have features in common: a power source capable of providing electric current, a capacitor that can be charged to a pre-determined energy level and two electrodes which are placed on the patient’s chest, either side of the heart, across which the capacitor is discharged. The electrodes may also act as monitoring electrodes for the ECG rhythm.
With manual defibrillators, the operator interprets the ECG and has to decide if the rhythm is one likely to respond to a shock. This requires skill and training requirements are therefore increased.
With automated external defibrillators (AEDs; Figure 6.1) voice prompts and instructions on a screen direct the operator through the procedure. ECG analysis is automated and the machine charges and directs the operator to deliver the shock if appropriate. Modern devices are highly accurate and reliable and it is almost impossible to deliver a shock inappropriately. Prompts to perform CPR are also given. Training in the use of AEDs can be achieved much more rapidly and easily than for manual defibrillators and has extended dramatically the range of personnel who can defibrillate.
Figure 6.1 Example of an automatic external defibrillator. Reproduced by permission of Professor Charles Deakin. Copyright © 2012 Charles Deakin.

The reliability of modern AEDs has made the concept of public access defibrillation (PAD) a reality. AEDs are placed in areas of high risk (transport and sporting facilities in particular) and are used by trained laypeople working nearby to provide defibrillation prior to ambulance arrival. Survival rates of up to 74% have been reported under optimal circumstances.
Factors influencing defibrillation
Transthoracic impedance
The success of attempted defibrillation depends on sufficient current being delivered to the myocardium. The major determinant of current flow is the electrical resistance presented by the thorax, the transthoracic impedance, which in adults is normally in the range 70–80 Ohm. Defibrillation technique must be optimised to minimise this transthoracic impedance thereby maximising the current delivered to the myocardium.
Transthoracic impedance can be influenced by various factors as outlined in Table 6.1.
Table 6.1 Factors affecting transthoracic impedance.
| Chest size/inter-electrode distance | Larger chest = higher impedance |
| The energy of the shock | Higher energies reduce impedance |
| Electrode size | Larger electrodes reduce impedance |
| Electrode and chest wall interface | Couplants (gels/pastes) lower impedance |
| Shaving hairy chests improves contact | |
| Phase of ventilation | Lower at end-expiration |
| Number of shocks | Impedance falls with successive shocks |
| Electrode pressure | Firm pressure lowers impedance |
Modern biphasic defibrillators measure transthoracic impedance immediately prior to shock delivery and adjust the energy delivered to compensate and are therefore less susceptible to higher transthoracic impedance (impedance compensation).
Shock waveform
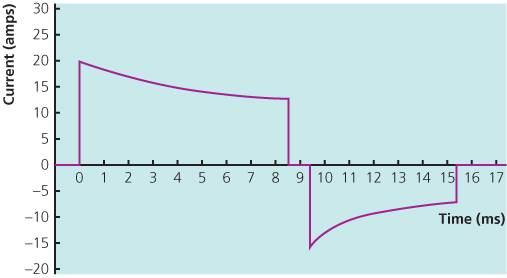
Biphasic defibrillators deliver current that flows in a positive direction for a specified duration before reversing polarity to a negative direction for the remainder of the electrical discharge. There are two main types of biphasic waveform: the biphasic truncated exponential (BTE; Figure 6.2) and the rectilinear biphasic (RLB; Figure 6.3); there is no evidence that either is more effective than the other.
Figure 6.2 Biphasic truncated exponential waveform. Reproduced from Deakin CD, Nolan JP, Sunde K, Koster RW. European Resuscitation Council Guidelines for Resuscitation 2010. Section 3: Electrical therapies. Resuscitation 2010;81:1293–1304. Copyright 2010, Elsevier.