I. INTRODUCTION
A. Common Problems and Diagnoses Requiring Neurocritical Care
1. Increased intracranial pressure (ICP) → requiring close monitoring, hyperosmolar therapy, and/or surgical intervention: related to edema (traumatic brain injury, strokes: posterior fossa or large strokes affecting the middle cerebral artery), lesions with mass effect (intracranial tumors, bleeding, and abscesses), hydrocephalus (mass or blood obstructing ventricles, disturbances in CSF homeostasis), CNS infections
2. Subarachnoid hemorrhage (SAH) → requiring close neurological and hemodynamic monitoring
3. Refractory seizures and status epilepticus → requiring intubation due to poor mental status, in the setting of sedating medications, or burst suppression
4. Infections of the CNS (meningitis, encephalitis) → requiring intubation due to poor mental status, ICP monitoring, seizure control
5. Neuromuscular disease presenting with respiratory failure (Guillain- Barré syndrome/acute inflammatory demyelinating polyneuropathy [AIDP], myasthenia gravis, amyotrophic lateral sclerosis) → requiring mechanical ventilation
6. Toxidromes: serotonin syndrome, neuroleptic malignant syndrome, benzodiazepine or alcohol withdrawal → requiring seizure control, close hemodynamic and cardiac monitoring, thermoregulation and intubation
7. Spinal cord injury → requiring close hemodynamic monitoring and management of autonomic dysregulation
8. Cardiac or pulmonary failure in the context of neurological injury
9. Impaired arousal with inability to maintain patent airways or need for mechanical ventilation
B. General Principles of Neurocritical Care: multimodal neuromonitoring (see Section II), neuroprotection, intracerebral hemodynamics
II. MONITORING
A. Neurological Examination: In general, minimize sedation and follow serial bedside exams, monitoring relevant parameters such as cortical, brainstem, and spinal cord function. In patients with status epilepticus or patients requiring sedation for elevated ICPs or pharmacological paralysis, the exam may be limited to checking brainstem reflexes.
1. Red Flags: Pupillary asymmetries (make sure patient has not been exposed to pharmacological stimuli such as atropine drops or nebulizers)—concerning for increasing ICP, ruptured posterior cerebral artery (PCA) or posterior communicating artery aneurysm; Cushing triad (combination of elevated blood pressure, bradycardia, and irregular respiration)—concerning for increasing ICP; impaired upgaze—concerning for hydrocephalus; decreasing NIFs/vital capacity or decreasing strength affecting the neck and bulbar muscles—concerning for worsening neuromuscular failure; meningismus—concerning for SAH or CNS infection; acute loss of reflexes and ascending paralysis—concerning for progressive AIDP
2. Document the exam in a simple and easily reproducible manner, and report findings in the following order: cognition (level of alertness, orientation, attention, language: ability to express and comprehend), cranial nerves, strength, sensation, deep tendon reflexes.
3. Start with a minimal stimulus and then escalate as needed (whisper before yelling, give verbal commands before pinching).
4. If the patient has a gaze preference or neglect, stand on the side that the patient’s gaze is turned towards.
5. Cortical function: In essentially all right-handed individuals and 70% of left-handed individuals, language is processed in the left hemisphere and attention in the right hemisphere. The motor cortex (precentral gyrus) controls the contralateral limbs. Sensation is processed in the postcentral gyrus of the contralateral hemisphere. The frontal eye fields direct gaze to the contralateral side, therefore a stroke (lack of stimulation on affected side) drives gaze toward the side of the injury (e.g., L-gaze deviation in a L-sided stroke) while a seizure (excessive stimulation on affected side) drives gaze toward the unaffected side (R-gaze deviation with L-sided seizure).
6. Brainstem function: The brainstem controls involuntary eye movements, pupillary function, facial sensation, and vital functions. Knowledge of its functions is critical in the evaluation of the comatose patient and the posterior circulation acute stroke syndromes (see Table 10.1).
7. Spinal cord function: In contrast to brainstem and cortical injuries, spinal cord injury often produces bilateral, symmetric impairment of the limbs but never facial weakness. Always distinguish anterior column function (strength, sensation of pin/temperature) from posterior column function (sensation of vibration, proprioception), document reflexes and sacral functions (anal sphincter tone, bulbocavernosus reflex). The aim of localization is to identify the highest level of injury.
a. Brown-Séquard syndrome of hemicord dysfunction is characterized by ipsilateral loss of motor and proprioceptive functions and contralateral loss of pain and temperature (fibers carried in the spinothalamic tract decussate at the spinal cord level).
| Common Findings in Brainstem Lesions | |
Lesion Level | Common Findings | Anatomic Pathway |
Midbrain | Midposition fixed pupils Ophthalmoplegia Hemiparesis, Babinski sign | Light reflex pathways Oculomotor nuclei Cerebral peduncles |
High pons | Pinpoint, reactive pupils Internuclear ophthalmoplegia Facial weakness Reduced corneal sensation | Sympathetic fibers Medial longitudinal fasciculus Facial nerve Trigeminal nerve |
Low pons | Horizontal reflex gaze paralysis Hemiparesis, Babinski sign | Abducens nerve, horizontal gaze center Corticospinal, corticobulbar tracts |
Medulla | Disordered breathing Hypotension, hypertension, dysrhythmias | Respiratory center Vasomotor center |
a. Anterior spinal artery syndrome is characterized by bilateral symmetric motor weakness and dissociated sensory loss, with impairments in pain and temperature sensation and preservation of proprioception and vibration (fibers for the latter are carried in the posterior column, which is supplied by the posterior spinal arteries).
b. Central cord syndrome is common in cervical spinal cord injuries and characterized by motor and sensory impairment predominantly affecting the upper extremities.
c. Cauda equina syndrome is characterized by variable degrees of bilateral lower motor neuron weakness in the legs (sparing the arms), sensory loss of the lower extremities and sacrum, and dysfunction of bowel and bladder.
B. ICP Monitoring
1. Intracranial compliance: The skull is a rigid box filled with incompressible brain parenchyma. When the volume inside the skull increases, there is evacuation of cerebrospinal fluid (CSF) into the extracranial subarachnoid space followed by a rapid rise in ICP (Fig. 10.1). ICP is normally less than 10 mmHg (5–15 mmHg); transient elevations up to 30 mmHg are usually tolerated. When ICP rises above 20 mmHg (or cerebral perfusion pressure [CPP] falls below 60 mmHg), cerebral blood flow (CBF) may be inadequate. Pressure gradients may exist between different compartments of the brain and can lead to clinical herniation even though measured or global ICP may not be significantly elevated.
2. ICP-monitoring devices and potential complications
a. The most common device is an external ventricular drain (EVD), usually placed in the right lateral ventricle. The ventricular catheter is connected to a transducer. The risks of complications include intracranial hemorrhage upon insertion and infection (the latter increases with duration of catheter presence). The great advantage is that this allows for drainage of CSF and can be recalibrated. Compared with other ICP-monitoring devices, EVDs are least susceptible to false readings over time.
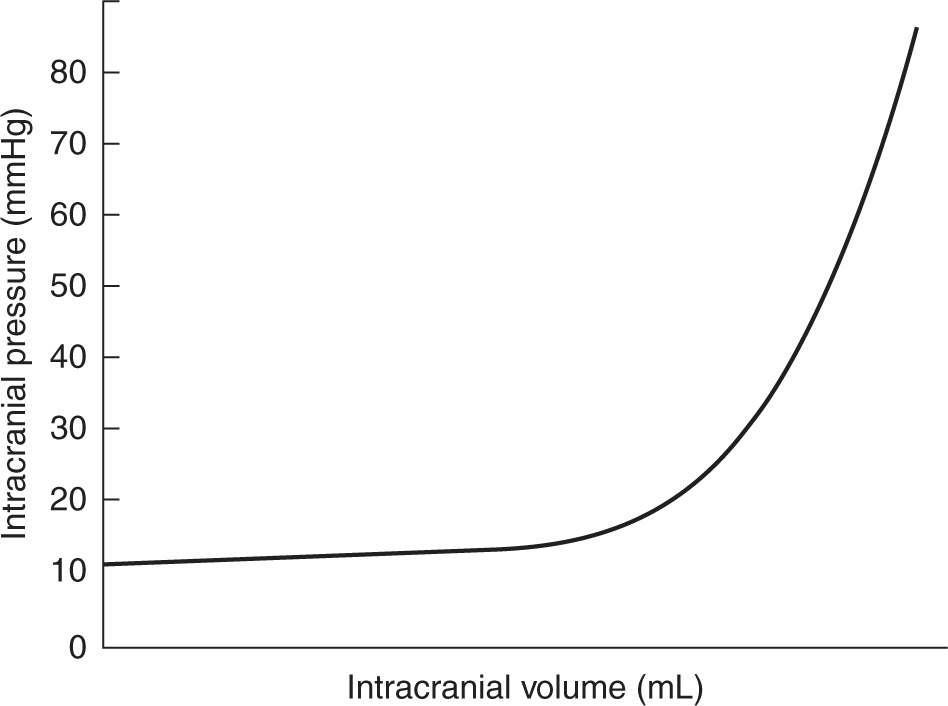
FIGURE 10.1 Intracranial compliance curve. In the normal ICP range; increases in intracranial volume produce minimal changes in ICP initially. Further small increases in intracranial volume at the “elbow” of the curve, however, can produce an abrupt increase in ICP. ICP, intracranial pressure.
b. Less invasive than EVDs are the transducer-tipped fiberoptic intraparenchymal catheters, which can be placed through a minicraniotomy. The device is placed several millimeters into the cortex but cannot be recalibrated once it has been placed. This requires special signal transducing monitors and may not be compatible with the available monitoring systems if patients are transferred between institutions. External transducers require periodic recalibration to remain accurate, sometimes called “zeroing” because of the task of zero calibrating to the level of the foramen of Monro.
c. In patients with temporal lesions, high ICPs at the level of injury might not be accurately measured by the monitoring device (which mostly capture ICPs in higher regions), so clinical judgment should be used when assessing the risk of herniation.
3. ICP waveforms:
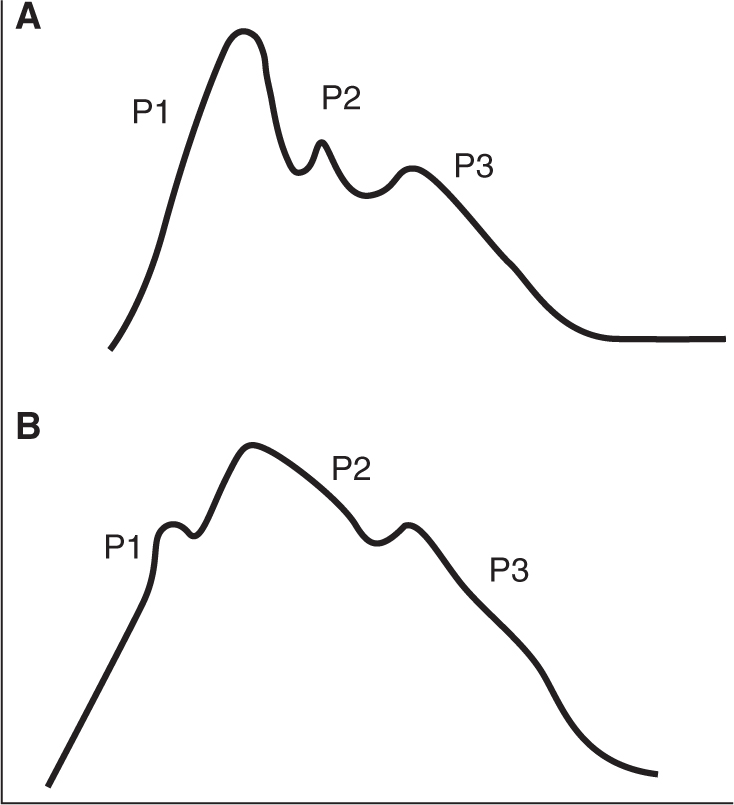
a. There are three components to an ICP wave: P1 (percussion wave) represents arterial pulsation, P2 (tidal wave) represents intracranial compliance, and P3 (dicrotic wave) represents aortic valve closure. Normally, P1 has the highest peak; if P2 > P1, there should be concern for impaired intracranial compliance and increased ICP in the appropriate clinical context (Fig. 10.2).
b. Lundberg A waves (“plateaus”) are characterized by increased ICP lasting >5 min, at times up to hours. They are pathological and strongly concerning for intracranial hypertension with the risk of herniation. Lundberg B waves are oscillations of ICP at a frequency of 0.5 to 2 waves/min. They have been noted in cerebral vasospasm and in the right clinical context can be associated with high ICP; at times they can progress to Lundberg A waves. Lundberg C waves are oscillations with a frequency of 4 to 8 waves/min. They have been noted in healthy individuals and are of unclear clinical significance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree