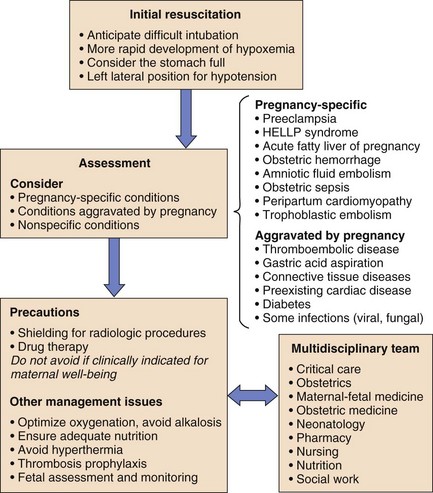
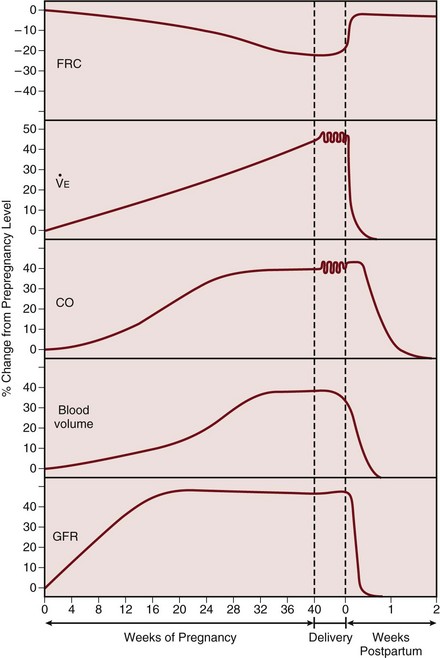
81 Management of the critically ill pregnant patient is a situation with which few intensive care physicians gain significant expertise. The usual clinical approach may be altered by the physiologic changes induced by pregnancy, by the relatively uncommon pregnancy-specific conditions, and by perceived limitations on therapy produced by the presence of a fetus (Fig. 81.1). The pregnant woman undergoes a number of physiologic changes affecting various systems relevant to critical care management. From a respiratory perspective, the upper airways develop edema and hyperemia, which may be relevant during endotracheal intubation. Changes in lung volumes occur, with a 10% to 25% decrease in functional residual capacity (FRC), whereas total lung capacity decreases only minimally as the thoracic cage widens to compensate.1 Forced expiratory volume in 1 second (FEV1) is not altered by the pregnant state. Lung compliance remains unchanged, but chest wall and total respiratory compliance are reduced.2 The rising progesterone level stimulates an increase in ventilation. Tidal volume and minute ventilation increase from the first trimester, reaching 20% to 40% above baseline by term (Table 81.1).3 A mild respiratory alkalosis is produced with compensatory renal excretion of bicarbonate (PaCO2 28 to 32 mm Hg; HCO3− 18 to 21 mEq/L). Oxygen consumption increases because of the demands of the fetus and maternal metabolic processes, reaching levels up to 33% above baseline by term. Arterial PO2 remains normal throughout pregnancy, but mild hypoxemia caused by an increased alveolar-arterial oxygen tension difference may develop in the supine position, as FRC diminishes near term. Table 81.1 Physiologic Changes in Late Pregnancy Maternal blood volume and cardiac output increase through pregnancy, reaching a peak at 30% to 50% above baseline levels by about 28 weeks (Fig. 81.2).4 Hemodynamic measurements by pulmonary artery catheter in the near-term patient demonstrate the increased cardiac output, with a reduced systemic vascular resistance and pulmonary vascular resistance (see Table 81.1).5 During labor and continuing into the immediate postpartum period, cardiac output is further augmented by the return of 300 to 500 mL of blood to the central circulation.6 Oxygen delivery to the fetus is dependent on the maternal arterial oxygen content and the uterine blood flow. Maternal hypotension, alkalosis (e.g., hyperventilation), and endogenous or exogenous catecholamines can vasoconstrict the uterine artery and adversely affect fetal oxygenation.7 Uterine blood flow is also reduced transiently by uterine contractions. Although umbilical venous blood returning to the fetus has a relatively low oxygen tension, a high oxygen content is maintained by the left shift of the oxygen dissociation curve of fetal hemoglobin. Glomerular filtration rate increases early in pregnancy, reaching a value 50% above prepregnancy levels in the second trimester, and remains elevated throughout pregnancy (see Fig. 81.2).8 The normal serum creatinine level is therefore in the range of 0.5 to 0.7 mg/dL (45 to 60 µmol/L). As pregnancy progresses, mild ureteric dilation and mild hydronephrosis may occur as a result of uterine compression and smooth muscle relaxation. The increase in plasma volume is associated with a lesser increase in red blood cell mass causing a physiologic anemia, with a hematocrit of 32% to 34% by the third trimester. A mild leukocytosis occurs with white blood cell count rising further during labor. Platelet counts are usually unchanged, although a condition of benign mild thrombocytopenia may occur.9 Procoagulant factors rise, contributing to the hypercoagulable state of pregnancy. The erythrocyte sedimentation rate (ESR) rises related to increased levels of plasma globulins. In the supine position the gravid uterus produces mechanical effects on the vena cava and aorta, reducing central venous return. This results in a decrease in cardiac output and hypotension. This “supine hypotensive syndrome” should be considered in hemodynamically unstable patients.10 Pregnant patients should be positioned on their left side, or at least with the right hip slightly elevated. Radiologic investigations are often essential for the assessment and management of the critically ill pregnant patient. Although there are potential risks of exposing the fetus to ionizing radiation, fetal well-being depends on maternal recovery, and appropriate radiologic procedures should not be avoided. Techniques such as shielding the abdomen with lead and using a well-collimated x-ray beam can effectively reduce exposure. With these precautions, estimated fetal radiation exposure can be limited to safe levels for most procedures, although investigations such as abdominal-pelvic computed tomography (CT) will obviously cause significant fetal radiation exposure (Table 81.2).11 Table 81.2 The adverse effects of fetal exposure to radiation include oncogenicity and teratogenicity. A twofold increased risk of childhood leukemia may result from fetal exposure in the range of 20 to 50 mGy (2 to 5 rads). Most intensive care unit (ICU) procedures can be carried out well below these levels of exposure to the fetus (see Table 81.2). Teratogenicity does not appear to occur at these radiation doses, requiring radiation exposure greater than 50 to 100 mGy (5 to 10 rads). Nonetheless, every effort should be made to minimize uterine exposure, particularly in the first trimester. Pharmacotherapy during pregnancy requires consideration of the altered drug clearance, metabolism, and volume of distribution of drugs in pregnancy, and the potential pharmacologic and teratogenic effects on the embryo. A detailed description of drug therapy in pregnancy is beyond the scope of this chapter. Consultation with an obstetrician and pharmacist is essential, and several excellent resources are available.12,13 Some common ICU drugs are discussed briefly as follows. Little data exist on the preferred drugs for prolonged sedation, analgesia, or neuromuscular blockade in pregnancy. Benzodiazepine use in early pregnancy has been associated with a small risk of congenital malformations, mainly cleft lip and palate. Midazolam crosses the placenta to a lesser degree than diazepam, which can accumulate in the fetus at levels greater than in the mother. Propofol has been used as an induction agent for cesarean section, but a single case report describes the development of non–anion gap acidosis in two pregnant women receiving propofol infusion for neurosurgical procedures.14 Congenital malformations have not been demonstrated with use of narcotic analgesics such as morphine, meperidine, and fentanyl. The majority of nondepolarizing neuromuscular blocking agents have been shown to cross the placenta including pancuronium, vecuronium, and atracurium, but transfer is unlikely to have clinical effects on the fetus in the short term. Nevertheless, if sedative or paralyzing agents are used in the pregnant woman, this information must be communicated to the neonatologist, who should anticipate the need for ventilatory support for the fetus. Attention to interventions aimed at optimizing fetal oxygenation is important in the management of any critically ill pregnant patient. Depending on gestational age, delivery of the fetus may be the most appropriate intervention. Uteroplacental oxygen delivery can be optimized by increasing oxygen carrying capacity—by blood transfusion, improving maternal cardiac output, and optimizing maternal oxygenation. The simple maneuver of tilting the patient to the left lateral position to increase cardiac output should always be considered.10 Failed intubation is more common in the obstetric population than in other anesthetic intubations.15 The reduced oxygen reserve caused by diminished FRC and increased oxygen consumption produces rapid desaturation in response to apnea or hypoventilation.16 Preoxygenation with 100% oxygen is beneficial, but respiratory alkalosis must be avoided. In view of the delayed gastric emptying and elevated intra-abdominal pressure, the pregnant patient should always be considered to have a full stomach and appropriate precautions should be taken. Upper airway hyperemia and edema may reduce visualization and necessitate use of a smaller endotracheal tube. The risk of bleeding is increased and nasal intubation should be avoided. The normal PaCO2 of about 30 mm Hg in late pregnancy should be considered in the interpretation of arterial blood gases when decisions are made to institute ventilatory support. Data on the prolonged mechanical ventilation of pregnant patients are limited. Hyperventilation should be avoided because this adversely affects uterine blood flow17 because of the resulting alkalemia as well as the effect of positive-pressure ventilation in reducing cardiac output. The current ventilatory approach of avoiding excessive lung stretch by pressure limitation and permissive hypercapnia has not been assessed in pregnancy. The usual pressure limits (e.g., plateau pressure of 35 cm H2O) may not be applicable in the near-term patient, in whom chest wall compliance is reduced. Transpulmonary pressures may not be elevated at a plateau pressure of 35 cm H2O, and higher ventilatory pressures may be acceptable in pregnant patients near term. Although late pregnancy is associated with a mild respiratory alkalosis, maternal hypercapnia up to 60 mm Hg in the presence of adequate oxygenation does not appear to be detrimental to the fetus.18 Maternal hypercapnia and respiratory acidosis may produce fetal acidosis, but this does not have the same ominous implications as fetal acidosis due to lactic acidosis resulting from fetal hypoxia.19 However, acidosis produces a right shift of the hemoglobin oxygen dissociation curve, which may negate the beneficial oxygen-carrying characteristics of fetal hemoglobin. If marked respiratory acidosis results from permissive hypercapnia, treatment with bicarbonate may improve maternal and fetal acidemia.
Critical Care Medicine in Pregnancy
Physiologic Changes in Pregnancy
Parameter
Change
Respiratory
Functional residual capacity
Decreased 10-25%
Minute ventilation
Increased 20-40%
Arterial partial pressure of oxygen
No change
Arterial partial pressure of carbon dioxide
Reduced to 28-32 mm Hg
Serum bicarbonate
Reduced to 18-21 mEq/L
Cardiac
Heart rate
Increased 10-30%
Pulmonary capillary wedge pressure
No change
Cardiac output
Increased 30-50%
Systemic vascular resistance
Decreased 20-30%
Pulmonary vascular resistance
Decreased 20-30%
Renal
Glomerular filtration rate
Increased 50%
Creatinine
Decreased (24-68 µmol/L; 0.29-0.77 mg/dL)
Critical Care Management
General Care
Positioning
Radiologic Procedures and Fetal Risk
Investigation
Fetal Radiation Exposure (mGy)
Chest radiograph (with abdomen shielded)
0.01
Ventilation-perfusion scan
Perfusion
0.1-1
Ventilation
0.1-0.4
CT pulmonary angiogram
0.1-4
CT scan of pelvis and abdomen
30-50
Radiation effect on fetus
Teratogenicity
50-100
Oncogenicity
20-50
Drug Therapy in Pregnancy
Sedation, Analgesia, and Neuromuscular Blockade
Fetal Oxygenation and Monitoring
Ventilatory Support
Airway Management
Mechanical Ventilation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Critical Care Medicine in Pregnancy

 , minute ventilation.
, minute ventilation. 



