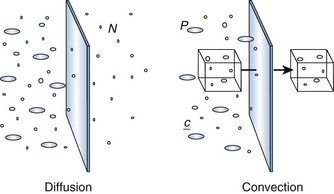
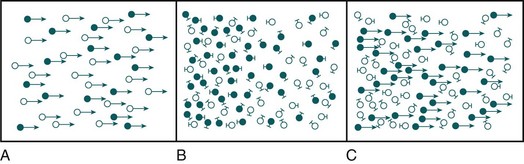
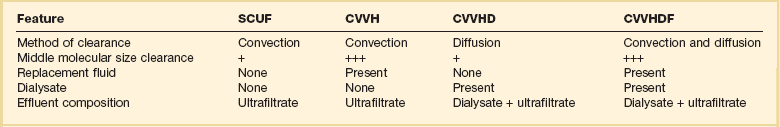
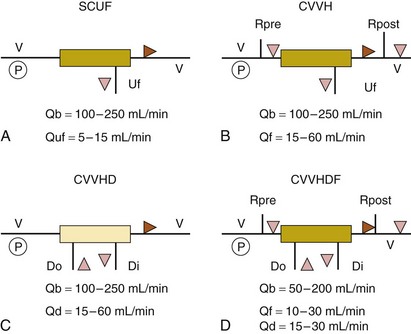
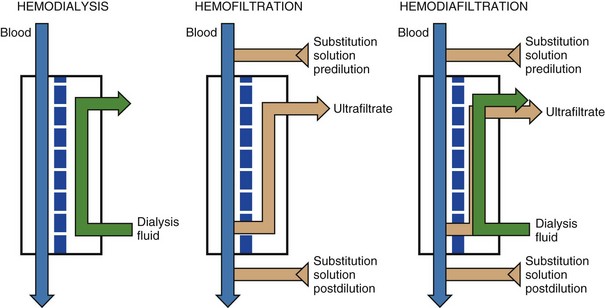
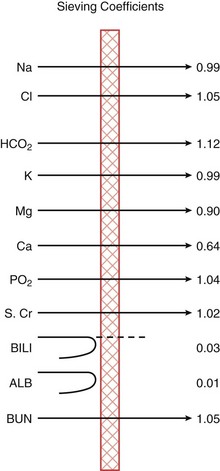
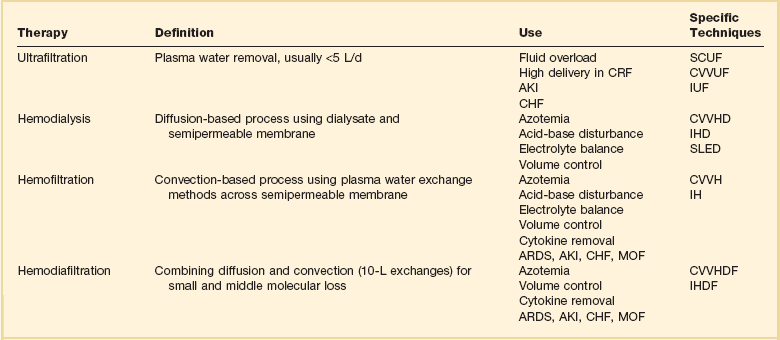
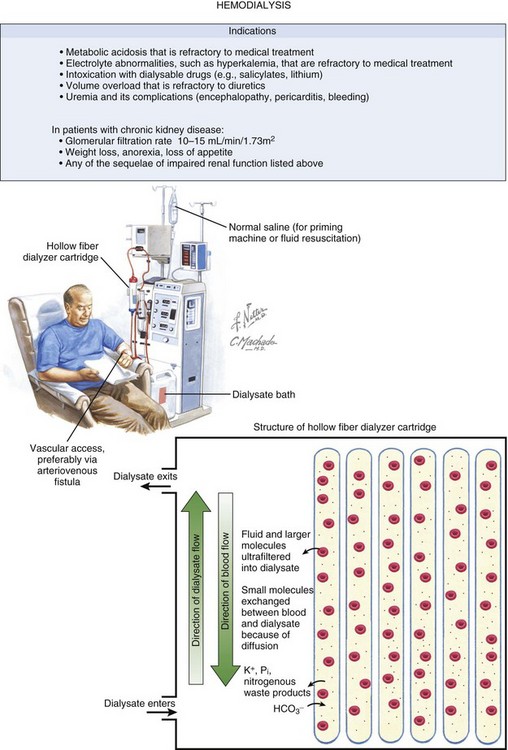
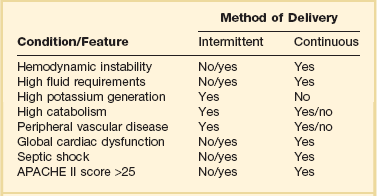
18 Acute kidney injury (AKI) is common and serious. The incidence of AKI in hospitalized patients ranges from 5% to 7% and is rising rapidly.1–4 In a multinational study of critically ill patients, the prevalence of AKI requiring dialysis was 5.7% with a mortality rate of 60.3%.5 In addition, patients with AKI have a higher risk for developing other nonrenal comorbid conditions,6 and when present in conjunction with other conditions, AKI is associated with higher mortality rate.7–9 The use of renal replacement therapy (RRT) for treatment of AKI has been ongoing over the last 60 years.10 According to Hoste and Schurgers, 200 to 300 patients per 1 million population per year develop AKI and are treated with RRT.11 Despite this, these patients still have a mortality rate of 50% to 60%.11Advances and optimization of RRT could benefit the high mortality rate associated with AKI. The establishment of continuous renal replacement therapy (cRRT) evolved as a treatment for the hemodynamically unstable patient unable to undergo standard intermittent hemodialysis (IHD). Although world trends for cRRT use show an increase in utilization, the majority of the world continues to treat AKI with IHD.12 Although cRRT offers many theoretical advantages such as better fluid balance, hemodynamic management, and renal recovery, the superiority of cRRT over IHD for RRT in the intensive care unit (ICU) remains controversial.13 Dialysis uses a semipermeable membrane to alter the molecular composition and concentration of blood to restore the body back toward homeostatic balance. Blood flows along one side of the semipermeable membrane and a wash solution, dialysate, flows on the opposite side of the membrane (Fig. 18.1). Dialysis relies upon two physical forces—diffusion and convection—either in isolation or in combination (Fig. 18.2). In diffusion, the net movement of solute is directly dependent on the diffusivity of the solute and solvent, permeability of the membrane, surface area across the membrane, and concentration gradient. Other membrane characteristics also play a role: thickness, pore size, and electrostatic charge. In order to maximize the concentration gradient between the blood and dialysate, the dialysate runs countercurrent to the flow of blood. Any substance that is in higher concentration in the blood than the dialysate flows “down” its concentration gradient and leaves the blood and flows into the dialysate. Conversely, any solute that is in higher concentration in the dialysate (e.g., bicarbonate) will leave the dialysate, cross the semipermeable membrane, and enter the blood. The movement of molecules down their concentration gradient from one solution to another continues until equilibrium is achieved in both the blood and dialysate. Diffusion is more efficient in the clearance of small-molecular-weight substances (less than 500 daltons [D]). This is particularly useful in correcting the imbalance in small molecule electrolytes (e.g., K, Ca, Mg, PO4) (see Fig. 18.1). Thus, thoughtful manipulation of dialysate allows the clinician to decide what will be removed from the blood and what will be added to the blood during a dialysis session. Figure 18.1 Hemodialysis and the filter at a microscopic level. Netter illustration from www.netterimages.com @ Elsevier Inc. All rights reserved. (Netter Plate 10-9 Membrane and Dialysis). In convection, solutes move across a membrane in response to or following solvent flux or drag: solutes are moving along with the solvent containing them (Fig. 18.3). This is similar to a wave pushing seashells onto the shore. Solvent drag is limited only by the pore size or electrostatic charge of any semipermeable membrane that is applied across the passage of the solution. In convection, the concentration of a solute is similar on either side of the membrane. Convection is more efficient at the clearance of large-molecular-weight substances (500-5000 D). Convective removal of plasma water from blood across a large-pore, semipermeable membrane results in an ultrafiltrate with a solute composition equivalent to plasma water. Fluid removal is termed ultrafiltration (UF). UF utilizes hydrostatic pressure, which is applied across a semipermeable membrane. This is a form of convective removal of solute. The clearance of molecules in UF is dependent on the volume of fluid removed. It may be applied in isolation (in volumes usually <5 L/day) or in combination with other blood clearance techniques, such as dialysis. Table 18.1 reviews the commonly used terms in cRRT. One other form of clearance of the blood is through a process called adsorption. This refers to molecules in the blood sticking or adhering to the semipermeable membrane. This process is dependent on the molecules contained in the blood and the composition of the semipermeable membrane. Adsorption is usually time dependent (i.e., as the semipermeable membrane is used over time, it will become saturated with a given molecule). The process begins anew when the membrane is changed (approximately every 72 hours). Some inflammatory cytokine clearance occurs through this process.14 The various modalities of cRRT are depicted in Table 18.1 and Figure 18.4. Dialysis may also be performed on an intermittent basis (IHD or sustained low-efficiency dialysis [SLED]) (see Fig. 18.1) or a continuous basis (Figs. 18.4 and 18.5). When performed continuously, this is known as continuous venovenous hemodialysis (CVVHD). The “venovenous” refers to the access employed and will be discussed in a later section. As described earlier, this is a diffusion-based process that primarily provides small molecule clearance. Hemofiltration (HF) relies on convective removal of plasma solute, in high fluid volumes, across a semipermeable membrane (see Fig. 18.5). Hydrostatic pressure is applied across the semipermeable membrane as a positive pressure on the blood side of the membrane or a negative pressure on the fluid collection side, or both. Fluid lost through this process is restored with replacement fluid in either a predilutional mode (before the filter containing the semipermeable membrane) or in a postdilutional mode (after the filter). The composition of the effluent fluid created by this system of plasma water exchange (hemofiltrate) depends on the membrane sieving coefficient for that particular solute and that particular semipermeable membrane. The sieving coefficient is expressed in terms of the ratio of the solute concentrations of the hemofiltrate to the plasma and is a function of membrane thickness, pore size, and electrostatic charge (Fig. 18.6). Hemofiltration is more efficient in middle-molecular-weight compound clearance, but less so for smaller solutes. When performed on a continuous basis, this is known as continuous venovenous hemofiltration (CVVH). Finally, hemodiafiltration (HDF) combines both diffusive and convective solute removal (see Fig. 18.5). When performed continuously, this is known as continuous venovenous hemodiafiltration (CVVHDF). Dialysate is used in this configuration and runs countercurrent to the blood. Concurrently, replacement solution is infused either prefilter or postfilter. This allows for both efficient low-molecular-weight and enhanced middle-molecular-weight clearances. This modality has been employed for sepsis and multiorgan failure, in which removal of cytokine mediator substances is thought to be important.15 Figure 18.4 illustrates the mechanics of each of these modalities. Any modality may be described according to its frequency (I [intermittent] versus C [continuous]) and technique (H or HF [hemofiltration], HD, HDF, or UF) as shown in Table 18.2. To date, no one modality has been shown to be superior to the others. Continuous techniques are additionally described according to their vascular access: arteriovenous (AV) or venovenous (VV) (see later discussion under “Access”). Much debate has occurred regarding the superiority of intermittent therapies versus the continuous therapies. To date, the continuous therapies have not been shown to be superior in clinical outcomes to the intermittent therapies. Although the intermittent therapies (IHD and SLED) may be less costly, the continuous modalities allow for hemodynamic stability, enhanced fluid removal, and delivered dose of dialysis.16 Postdilutional fluid replacement has the advantage of being easier to perform, with lower rates of fluid exchange compared with the predilutional system. One problem with this form of replacement is the increased oncotic pressures at the venous end of the filter. With high rates of exchange or high degrees of access recirculation, blood viscosity may be increased to the extent that clotting may occur. Therefore, fluid exchange rates may be dictated by such factors as hematocrit, blood flow, and access recirculation. Table 18.3 compares predilutional and postdilutional CVVH. Table 18.3 In CVVHD, dialysate flow rates remain the most influential factor in determining urea clearance.17 Dialysate usually is delivered via pumps at rates of 15 to 40 mL per minute. Given adequate blood flow through the circuit, one can see why the limiting factor for flow-dependent transfer is the relatively low dialysate flow rate. Blood flow and filter membrane have limited effects on the diffusion of molecules compared with the potential of dialysate flow changes. The clinical presentation and circumstances may favor either intermittent or continuous therapies (Table 18.4). There are many theoretical benefits that may favor the use of cRRT over intermittent forms of therapy, such as improved hemodynamic stability, faster resolution of fluid overload, and increased dialysis dose delivery (Table 18.5). Box 18.1 lists some nonrenal indications for using cRRT. However, clinical trials demonstrating an evidence-based assessment of these potential advantages are still lacking. Table 18.4 Clinical Considerations in Continuous versus Intermittent Renal Support in the Intensive Care Unit Definitive data to support many of the suspected advantages of cRRT are still lacking. In fact, Box 18.2 lists some of the disadvantages of cRRT. Interpretation of much of the published data has been hampered by retrospective analysis, the use of historical control groups, incomplete randomization, incomplete descriptions of patient populations and dialysis dose delivery, and study group–control group heterogeneity.
Continuous Renal Replacement Therapy
Physiologic Principles
Modalities
Principles of Hemofiltration
Feature
Predilution
Postdilution
Clearance
Less clearance per milliliter
High small solute clearance per milliliter
Efficiency
Reduced efficiency by 10-15% and reduced filtration fraction
Ultrafiltration rate limitations
Ultrafiltration rate not limited
Ultrafiltration rate limited by blood pressure and hemoconcentration
Blood viscosity
Low viscosity of the blood
High viscosity of the blood and increased risk of clotting
Principles of Hemodialysis
Continuous Renal Replacement Therapy Versus Intermittent Therapy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Continuous Renal Replacement Therapy