DEFINITION
Neurolytic blocks involve the destruction of a nerve and are commonly performed in patients with severe pain secondary to advanced cancer or occlusive vascular disease, while their use in chronic nonmalignant pain (e.g., chronic relapsing pancreatitis) is more limited. Raj recommended the following five criteria for neurolysis1: (i) the presence of severe pain, (ii) the failure of less invasive techniques to relieve the pain, (iii) the presence of well localized pain, (iv) the relief of pain with diagnostic local anesthetic blocks, and (v) the absence of undesirable effects after diagnostic blocks (Box 31-1).
BOX 31-1 Criteria for Use of Neurolytic Blockade
 Pain is severe
Pain is severe
 Pain persists after use of less invasive treatment
Pain persists after use of less invasive treatment
 Pain is well localized
Pain is well localized
 Pain is relieved with diagnostic blocks using local anesthetic
Pain is relieved with diagnostic blocks using local anesthetic
 No undesirable effects appear during local anesthetic blocks
No undesirable effects appear during local anesthetic blocks
Adapted from Raj PP. Peripheral neurolysis in the management of pain. In: Waldman SD, Winnie AP, eds. Interventional Pain Management. Philadelphia, PA: WB Saunders, 1996:392–400.
Neurolytic blockade carries significant risk of potentially devastating side effects and life-altering but predictable consequences that must be carefully weighed against the expected benefits of pain reduction. For this reason, neurolytic blocks are best suited to patients with a short life expectancy who experience severe pain despite aggressive conservative attempts to control the pain. For instance, neuraxial neurolysis can provide profound pain relief for patients with pain related to invasive tumors involving the pelvis, but this approach often also leads to loss of bowel and/or bladder function and may well also produce weakness in the lower extremities. It should also be emphasized that relief from neurolytic blocks is usually not complete, since most patients with cancer pain have multiple sources of their pain.
Neurolytic blocks can be peripheral, neuraxial, or visceral. Of the three, visceral blocks are most commonly performed, while neuraxial and peripheral neurolytic blocks are performed less frequently for several reasons. In the case of peripheral neurolytic nerve blocks, blocking mixed motor and sensory nerves can cause motor deficit leading to loss of functionality for the patient. In addition, peripheral neuritis and deafferentation pain are potential painful consequences, while the block itself is not predictably permanent.1 Finally, the patient may also be dissatisfied with the subsequent numbness of the area (Box 31-2).
BOX 31-2 Limitations of Peripheral Neurolytic Blocks
 Motor deficits are likely when mixed sensory-motor nerves are blocked.
Motor deficits are likely when mixed sensory-motor nerves are blocked.
 Neuritis/deafferentation pain may occur and can be more severe than preexisting pain.
Neuritis/deafferentation pain may occur and can be more severe than preexisting pain.
 Neurolytic blocks are not predictably long lasting or permanent.
Neurolytic blocks are not predictably long lasting or permanent.
 Sensory loss following peripheral neurolysis is often bothersome to the patient.
Sensory loss following peripheral neurolysis is often bothersome to the patient.
Adapted from Raj PP. Peripheral neurolysis in the management of pain. In: Waldman SD, Winnie AP, eds. Interventional Pain Management. Philadelphia, PA: WB Saunders, 1996:392–400.
Neuraxial neurolytic blocks, including both subarachnoid and epidural alcohol or phenol neurolytic blocks, are rarely used today because neuraxial opioids can effectively and safely be used in the treatment of cancer pain. Where an intrathecal drug delivery system can provide widespread pain relief that can be adjusted to accommodate many scenarios, a successful neurolytic block may have to be repeated with changes in pain pathology, such as the presence of new metastatic lesions. In such cases, it is impractical to perform subsequent subarachnoid neurolytic injections due to their attendant risks, while an indwelling intrathecal drug delivery system will cover new areas of pain and continue to be useful. Visceral neurolytic blocks are among the most useful neurolytic blocks and are still in common use today. The viscera are usually supplied by a plexus of sympathetic nerves (e.g., celiac plexus) that are amenable to neurolysis. Properly done, visceral neurolytic blocks have no attendant motor weakness and the effects are predictable and gratifying. This chapter reviews complications from neurolytic blocks related to the technical aspects of needle placement and those that may result from the actions of the neurolytic agent.
 COMPLICATIONS FROM NEUROLYTIC AGENTS: PHARMACOLOGY AND PATHOPHYSIOLOGY
COMPLICATIONS FROM NEUROLYTIC AGENTS: PHARMACOLOGY AND PATHOPHYSIOLOGY
The neurolytic agents commonly employed include ethyl alcohol, phenol, and, less commonly, glycerol. Ethyl alcohol causes neurolysis by extracting cholesterol, phospholipids, and cerebrosides from the nervous tissue and precipitating lipoproteins and mucoproteins.2 Its injection into a peripheral nerve results in wallerian degeneration wherein the axon and the Schwann cell are damaged.3 In wallerian degeneration, the axon breaks down and the myelin sheath retracts, forming ellipsoids of myelin.4 The axoplasm gets enclosed within the ellipsoids of myelin, followed by hydrolysis within the ellipsoids by lysosomal enzymes. Regeneration occurs during the 1st week of injury when Schwann cells start to multiply and macrophages ingest debris.4 By the end of the 1st week, Schwann cells may develop a chain within the endoneurium. Macrophages disappear after 2 weeks, whereas endoneurial tubes are filled with Schwann cells. When neurolytic agents are injected into the subarachnoid space, the changes occur in the dorsal roots, posterior portion of the spinal cord, and the Lissauer’s tract.5
Alcohol is commercially available as a 95% concentration, which is more than adequate for neurolytic blocks since studies have shown that a concentration of 33% or greater is necessary to affect neurolysis.6 Ethyl alcohol is used in a variety of neurolytic blocks, such as visceral sympathetic blocks (celiac plexus, superior hypogastric plexus), lumbar paravertebral sympathetic blocks, and injections into the subarachnoid space and the trigeminal ganglia. Some authors recommend injecting a local anesthetic before the alcohol injection, because it is an irritant and causes burning pain upon injection. Alcohol is injected undiluted when used for peripheral injections. In celiac plexus blocks, the alcohol is usually diluted with a local anesthetic to a concentration of 50% to diminish the pain upon injection. Alcohol is hypobaric with respect to the cerebrospinal fluid, and the patient has to be positioned with the painful side up when intrathecal injection is performed. Denervation and relief of pain usually occurs over a few days after injection and is complete after 1 week.1 Intravascular injection of 30 mL of 100% ethanol will result in a blood ethanol level well above the legal limit for intoxication, but below the danger of severe alcohol toxicity. Intravenous injection may cause thrombosis of the vessel.7 Complications of using ethanol for neurolytic blocks range from transient paraplegia to irreversible spinal cord damage.8,9 Of note, ethanol has been increasingly used in the rehabilitation setting to treat spasticity in post stroke patients.10,11
Phenol, also known as carbolic acid, causes neurolysis by coagulating proteins within nerve tissue. There is minimal discomfort on injection since it acts as a local anesthetic at lower concentrations. It has a strong affinity for vascular tissue, and injury to the blood vessels at or near nervous tissues may contribute to its neurotoxicity.12 For this reason, some clinicians prefer alcohol in celiac plexus blocks because the injection of phenol puts the nearby major blood vessels at risk. Five percent phenol is equivalent to 40% alcohol in neurolytic potency.13 The intrathecal injection of phenol causes changes similar to that of alcohol, and there is degeneration of fibers in the posterior columns and posterior nerve roots. The degree of damage after peripheral injection is concentration-dependent, and the changes range from segmental demyelination to wallerian degeneration.14
The concentrations of phenol used for neurolysis range from 3% to 15%. The authors use a 6% aqueous solution. At lower concentrations, it acts as a local anesthetic, and as a result, there is minimal discomfort upon injection of the drug. Phenol is relatively insoluble in water and at concentrations above 6% has to be prepared with the addition of glycerin. At these concentrations, it is fairly viscous. Phenol has a clinical biphasic action, and the initial relief is secondary to its local anesthetic effect. This relief fades within the first 24 hours, and lasting analgesia occurs 3 to 7 days after the injection secondary to the neurolytic action of the drug. Phenol is hyperbaric with respect to cerebrospinal fluid, and the patient has to be positioned with the painful side down when subarachnoid injection is performed. The intravascular injection of phenol results in convulsions secondary to an increase in the excitatory transmitter acetylcholine in the central nervous system.15 Large systemic doses of phenol (>8.5 g) cause effects similar to those seen with local anesthetic overdose: generalized seizures and cardiovascular collapse. Acute renal and pulmonary collapse requiring hemodialysis and ventilatory support has been reported with large systemic doses of phenol as well.16 Clinical doses up to 1,000 mg are unlikely to cause serious toxicity. Like ethanol, it should be noted that phenol is not only used for the management of pain but in the treatment of spasticity.17
 COMPLICATIONS FROM SPECIFIC NEUROLYTIC BLOCKS
COMPLICATIONS FROM SPECIFIC NEUROLYTIC BLOCKS
Neurolytic agents can be injected into peripheral nerves, along the neuraxis within the intrathecal or epidural spaces or adjacent to visceral sympathetic nerves. Each of these sites of injection is associated with specific complications. Peripheral neurolysis includes injection into the trigeminal ganglion, truncal, upper and lower extremities, trigger points, and neurolysis for spasticity.1
Neurolytic Blocks of the Head and Neck
Gasserian Ganglion Neurolysis
Blockade of nerves in the head and neck is performed for variety of reasons (Table 31-1). These include blockade of the trigeminal ganglion for trigeminal neuralgia that is not responsive to medical management and for relief of cancer pain secondary to invasive tumors of the orbit, maxillary sinus, and mandible; neurolysis of the pituitary for metastatic cancer (specifically breast and prostate cancer); and blockade of individual peripheral nerves in the head.
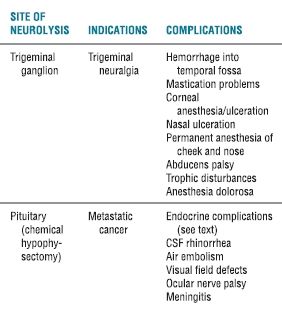
TABLE 31.1 Indications and Complications from Neurolysis in the Head
The gasserian ganglion is formed from two trigeminal roots that exit the ventral surface of the brain stem at the midpontine level.18 The roots pass forward and in a lateral direction, in the posterior fossa of the cranium, across the border of the petrous temporal bone. It then enters the Meckel’s cave in the middle cranial fossa. The gasserian ganglion contains the ophthalmic, maxillary, and mandibular divisions. A smaller motor root joins the mandibular division as it exits the foramen ovale. It should be noted that a dural pouch, the trigeminal cistern, lies behind the trigeminal ganglion. In gasserian ganglion block, the needle is inserted approximately 2.5 cm lateral to the side of the mouth and advanced, perpendicular to the middle of the eye (with the eye in the midposition), in a cephalad direction toward the auditory meatus.19 When contact is made with the base of the skull, the needle is withdrawn and “walked” posteriorly toward the foramen ovale. A free flow of CSF is usually noted, and fluoroscopy is then used to confirm correct needle placement. Very small amounts (i.e., 0.1 mL increments) of local anesthetic or neurolytic agent are injected to a total of 0.4 to 0.5 mL. Either absolute alcohol or 6.5% phenol in glycerin is employed as the neurolytic agent. Due to their different baricities, the patient remains supine if alcohol is used but placed in a sitting position with the chin on the chest prior to the injection of phenol. This maneuver localizes the phenol around the maxillary and mandibular divisions of the trigeminal nerve, avoiding the ophthalmic division and the risk of keratitis from loss of the conjunctival reflex.
The pterygopalatine space is highly vascular, and significant hematoma of the face and subscleral hematoma of the eye can occur. Veins in the subtemporal region can be punctured, causing hemorrhage in the temporal fossa. Local anesthetic injection can lead to spinal anesthesia because the ganglion lies within the cerebrospinal fluid. Blockade of the motor fibers of the trigeminal nerve can interfere with mastication.20 Oculomotor palsy, which results in diplopia and strabismus, is usually temporary. Abducens palsy is also temporary, although cases of permanent lateral rectus palsy have been reported.7 Spread of the neurolytic agent into the facial nerve results in paralysis of the facial muscles and inability of the eyelid to close, resulting in keratitis or corneal ulceration. Blockade of the greater superficial petrosal nerve may result in lack of tear formation and conjunctivitis. Blockade of the acoustic nerve may result in deafness or dizziness. The delayed effects of gasserian ganglion neurolytic block include trophic problems such as keratitis, ulcerations in the nose, and erosions in the mouth. These disturbances usually occur after trauma to the area. Another delayed complication is anesthesia dolorosa. Since the neurolytic block of the gasserian ganglion is associated with myriad devastating complications, many neurosurgeons and pain medicine practitioners choose to perform radiofrequency rhizotomy of the ganglion instead.7 The same approach is employed when radiofrequency needles are advanced to the ganglion. With stimulation, the nerve fibers coming from the region of the lancinating pain are localized and selectively destroyed with the radiofrequency current. Since no chemical neurolytic is used, spread of the neurolytic agent into the CSF and surrounding structures is not a consideration with radiofrequency rhizotomy. The complications of thermal radiofrequency rhizotomy of the trigeminal ganglion are related either to the placement of the needle or to thermal lesion to the surrounding tissue. Some common complications and their incidences include masseter weakness (18%), paresthesia/dysesthesia (20%), diplopia (1.5%), and keratitis (3%).21 Other complications include inadvertent injury to the surrounding tissue (puncture of cavernous sinus, carotid artery, jugular foramen, or foramen magnum) or oculomotor, trochlear, and abducens nerve injury.22 The incidences of the different complications with chemical neurolysis and radiofrequency rhizotomy of the gasserian ganglion are listed in Table 31-2. The technical difficulty and complications associated with gasserian ganglion block led some investigators to perform peripheral branch (supraorbital, infraorbital, and mandibular nerves) injections with 10% phenol to relieve the pain of tic douloureux.23
TABLE 31.2 Complications from Trigeminal Ganglion Neurolysis
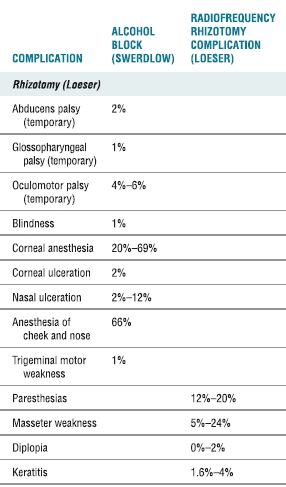
The nerve palsies were temporary.
Adapted from (a) Swerdlow M. Complications of neurolytic neural blockade. In: Cousins MJ, Bridenbaugh PO, eds. Neural Blockade in Clinical Anesthesia and Management of Pain. 2nd ed. Philadelphia, PA: JB Lippincott, 1988:719–735. (b) Loeser JD, Sweet WH, Tew JM, et al. Neurosurgical operations involving peripheral nerves. In: Bonica JJ, ed. The Management of Pain. 2nd ed. Philadelphia, PA: Lea & Febiger, 1990:2044–2066.
Pituitary Ablation
Chemical ablation of the pituitary with alcohol was widely used in the late 1970s and early 1980s, where it was recommended for the treatment of metastatic cancer pain, especially breast and prostate cancer.24,25 Among this patient population, the results seemed to be better in patients with hormone-dependent tumor. Since that time, modifications of the original technique have been proposed to simplify the approach and to decrease the incidence and severity of cerebrospinal fluid leak.24,26 The patient must be intubated and sedated for the procedure. A spinal needle is advanced, under biplanar fluoroscopic guidance, through the nose until the tip rests against the anterior wall of the sella turcica. Phenol or alcohol, in aliquots of 0.2 mL, is injected to a total of 4 to 6 mL. The pupils are monitored during the injection. Papillary dilatation indicates spillage of the drug outside the sella and blockade of the oculomotor nerve. The injection is stopped if this occurs, and the needle is reinserted to a more anterior position. Cyanomethacrylate resin 0.5 mL is injected before the needle is withdrawn to prevent CSF leak. Cryoneurolysis and radiofrequency lesions have also been described.27
Most of the complications are related to the destruction of the pituitary gland, including diabetes insipidus, adrenal insufficiency, hypothyroidism, hypothermia, and lowering of libido.24,25,28 Other complications include CSF rhinorrhea, impairment of consciousness, visual field defects, ocular nerve palsy, air embolism, and meningitis (Table 31-1). The incidences of these complications have been described by Swerdlow and Waldman29 (Tables 31-2 and 31-3). Whereas Waldman found an incidence of 1% for CSF rhinorrhea, Swerdlow7 noted a range of 1% to 20% in published reports. Swerdlow also noted an incidence of 1% to 10% for visual field defects, 1% to 32% for ocular nerve palsy, and 1% to 2% for meningitis. The endocrine complications cannot be prevented but are treated with replacement therapy. Fluoroscopic guidance and meticulous technique will help prevent some of the complications, and perioperative administration of antibiotics and sterile technique prevents the infectious complications.
TABLE 31.3 Incidence of Complications of Neuroadenolysis of the Pituitary
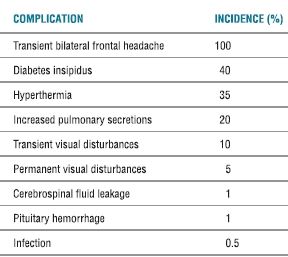
From Waldman SD. Neuroadenolysis of the pituitary: indications and technique. In: Waldman SD, Winnie AP, eds. Interventional Pain Management. Philadelphia, PA: WB Saunders, 1996:519–525 with permission.
Other Neurolytic Blocks of the Head and Neck
Neurolytic blocks of individual cranial nerves and their branches have also been performed, and complications are related to nerve location and the tissues innervated. Neurolytic block of the maxillary nerve at the foramen rotundum or of the infraorbital nerve may cause ulceration and sloughing of the ala of the nose and the cheek, ischemic necrosis of the palate, or sloughing of the posterior portion of the superior ridge of the maxilla.7 Blockade of the mandibular nerve at the foramen ovale may result in weakness of the muscles of mastication in the blocked side, whereas blockade of the facial nerve causes weakness or paralysis of the facial muscles. Blockade of the glossopharyngeal nerve is rarely performed because of proximity of the nerve to the vagus, spinal accessory, and hypoglossal nerves. The close location of the other nerves led investigators to recommend blockade of the glossopharyngeal nerve under fluoroscopic control30 or to use radiofrequency rhizotomy.31 The sensory area of innervation of the glossopharyngeal nerve includes the nasopharynx, eustachian tube, uvula, tonsil, soft palate, base of the tongue, and part of the external auditory canal.1 Paralysis of the pharyngeal muscles is a consequence of blockade of the glossopharyngeal nerve.
Stellate Ganglion Neurolysis
The cervical sympathetic trunk contains the superior, middle, and inferior cervical ganglia. In 80% of the population, the lowest cervical ganglion is fused with the first thoracic ganglion, forming the cervicothoracic (stellate) ganglion. The cervical sympathetic chain lies anterior to the prevertebral fascia, which encloses the prevertebral muscle. The sympathetic chain is enclosed within the alar fascia, a thin fascia that separates the cervical sympathetic chain from the retropharyngeal space. The carotid sheath is connected to the alar fascia by a mesothelium-like fascia. The fascial plane that encloses the sympathetic chain may be in direct communication with several spaces and structures, including the brachial plexus, vertebral artery, endothoracic fascia, and the thoracic wall muscle at T1-T2. At the C6 level, the cervical sympathetic trunk is located posterolaterally to the prevertebral fascia on the surface of the longus colli muscle.32 The carotid vessels are anterior, whereas the nerve roots that contribute to the inferior portion of the brachial plexus are lateral to the ganglion. The vertebral artery passes over the ganglion and enters the vertebral foramen posterior to the anterior tubercle of C6. The communications of the fascia covering the stellate ganglion with several structures, as noted previously, and the proximity of the stellate ganglion to the vertebral and carotid vessels, phrenic nerve, and the recurrent laryngeal nerve explain some of the potential complications of the stellate ganglion block.33
Several techniques of stellate ganglion block have been described. These include insertion of the needle at the level of C6, placement of the needle at C7, and the posterior thoracic approach.33 With C6 placement, the needle is in contact with either the C6 tubercle or the junction between the C6 vertebral body and the tubercle (Fig. 31-1). The needle is withdrawn 2 mm, an initial test dose of 0.5 to 1 mL is injected, and volumes of 5 to 10 mL have been injected. The injectate travels caudad and reaches the stellate ganglion and the upper thoracic sympathetic ganglia.34 A smaller volume of drug is adequate when the needle is placed at the level of C7. However, there is increased incidence of vertebral artery injection with this approach because the artery lies anterior to the C7 transverse process. There is also an increased risk of pneumothorax because the dome of the lung is close to the injection site. The posterior thoracic approach requires fluoroscopic guidance to identify the lamina of T1 or T2, and dye injection is recommended to document the spread of the drug. In this approach, the needle contacts the lamina of T1 or T2, is moved laterally off the lamina, and is advanced to pass the costotransverse ligament at a depth of 2 cm beyond the lamina. Either loss of resistance is used or dye is injected to confirm proper needle placement.
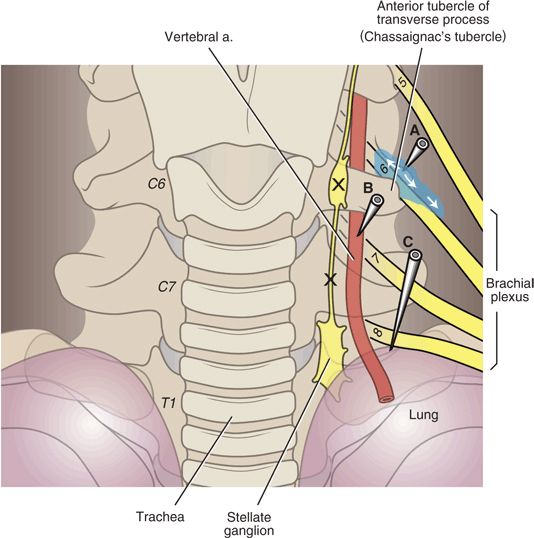
FIGURE 31-1. Complications of stellate ganglion neurolysis. The stellate ganglion conveys sympathetic fibers to and from the upper extremities and the head and neck. The ganglion is composed of the fused superior thoracic ganglion and the inferior cervical ganglion and is named for its fusiform shape (in many individuals, the two ganglia remain separate). The stellate ganglia lie over the head of the first rib at the junction of the transverse process and uncinate process of T1. The ganglion is just posteromedial to the cupola of the lung and medial to the vertebral artery, and these are the two structures most vulnerable. Stellate ganglion block is typically carried out at the C6 or C7 level to avoid pneumothorax, and a volume of solution that will spread along the prevertebral fascia inferiorly to the stellate ganglion is employed (usually 10 mL). When radiographic guidance is not used, the operator palpates the anterior tubercle of the transverse process of C6 (Chassaignac’s tubercle), and a needle is seated in the location. With radiographic guidance, it is simpler and safer to place a needle over the vertebral body just inferior the uncinate process of C6 or C7 (locations of proper needle placement are marked X). Incorrect needle placement can lead to pneumothorax, damage to the vertebral artery or intra-arterial injection, or spread of the injectate adjacent to the exiting spinal nerves where they join to form the brachial plexus. Contrast can also course proximally along the spinal nerves to the epidural space. (Modified from Rathmell JP. Atlas of image-guided intervention in regional anesthesia and pain medicine. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2012, with permission.)



