Chapter 23
Care of the Patient Infected with Human Immunodeficiency Virus Infection
HIV-Related Complications
Although HIV-related complications may occur throughout the entire spectrum of immunodeficiency, certain conditions are unusual until a patient’s CD4+ lymphocyte falls to less than a certain threshold (Tables 23.1 and 23.2). Furthermore, as the patient’s CD4+ lymphocyte counts continue to decline below these thresholds, the risk for these complications increases.
TABLE 23.1
Thresholds of CD4+ Lymphocyte Counts and Disease Manifestations for Selected Pathogens
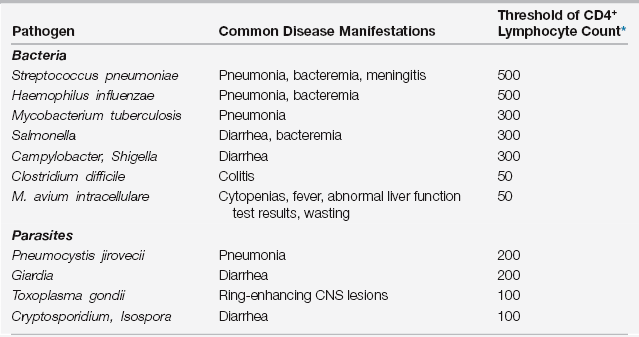
∗The CD4+ lymphocyte count (cells/μL) when each complication may be first encountered. The risk for each complication continues to increase as the CD4+ lymphocyte count declines further.
TABLE 23.2
| Complication | Common Disease Manifestations | Threshold of CD4+ Lymphocyte Count∗ |
| Immune thrombocytopenic purpura | Thrombocytopenia | 500 |
| Non-Hodgkin lymphoma | Adenopathy, wasting | 300 |
| Nephropathy | Nephrotic syndrome, renal insufficiency | 200 |
| Cardiomyopathy | Congestive heart failure | 100 |
| CNS lymphoma | Ring-enhancing CNS lesions | 50 |
∗The CD4+ lymphocyte count (cells/μL) when each complication may be first encountered. The risk for each complication continues to increase as the CD4+ lymphocyte count declines further.
Pulmonary Complications
Bacterial Pneumonias
Likewise, Haemophilus influenzae pneumonia occurs 100 times more often in HIV-infected versus non-HIV-infected patients. Because the organisms for most of these Haemophilus species cannot be typed, H. influenzae type b vaccine is also not protective. Although other pyogenic bacteria are less common causes of pneumonia in HIV-infected patients, Pseudomonas aeruginosa pneumonia may be seen in late stages of disease (usually associated with a CD4+ lymphocyte count < 100 cells/μL, cavitary lung disease, or prior treatment with broad spectrum antibiotics). In addition, Staphylococcus aureus, including methicillin-resistant strains, is an increasingly common cause of community-acquired pneumonia in HIV-infected patients and should be suspected in patients with a history of viral respiratory infection, intravenous drug use, or severe bilateral infiltrates (Chapter 65). Legionella pneumonia occurs infrequently, but its incidence is increased 40-fold in HIV-infected versus non-HIV-infected patients.
Empiric treatment of HIV patients with community-acquired pneumonia requiring ICU admission includes an intravenous (IV) beta-lactam plus either azithromycin or a respiratory fluoroquinolone (moxifloxacin or levofloxacin 750 mg daily) (Chapters 18 and 65). For patients with those risk factors for Pseudomonas pneumonia listed above, the preferred beta-lactam agents include piperacillin-tazobactam, cefepime, imipenem, and meropenem. Vancomycin or linezolid should be added to the antibiotic regimen if Staphylococcus is suspected.
Pneumocystis Pneumonia
Diagnostic Considerations
Induced sputum after ultrasonic nebulization of hypertonic saline may diagnose PCP in 15% to 90% of cases, depending on local experience and expertise. It is, however, rarely diagnosed in expectorated sputum without induction. When induced sputum testing is not available or yields a negative result, fiberoptic bronchoscopy should be performed. Specimens obtained by bronchoalveolar lavage (BAL) have a diagnostic yield of 86% to 97%, especially if BAL of both lungs is performed. BAL is more sensitive than standard bronchial washing and brushing. Transbronchial lung biopsy (TBBx) has a sensitivity similar to BAL but may detect some cases missed by BAL. When TBBx is combined with BAL, some centers report a sensitivity of 100%. Evidence suggests that BAL is not sufficient as a single modality to diagnose PCP in patients receiving aerosolized pentamidine for prophylaxis. In this setting, it should always be combined with TBBx.
Mycobacterial Infections
Reactivity to tuberculin skin testing is inversely related to CD4+ counts. Among patients with AIDS and active TB, only 10% to 30% of patients will have a skin test reaction that is greater than or equal to 10 mm of induration. Sputum is positive by microscopy for acid-fast bacilli (AFB) in 40% to 65% of HIV-infected patients with active TB, and it is positive by AFB culture in 75% to 95% of patients. For patients who have not had a diagnosis made from sputum, BAL is diagnostic by AFB smear in 7% to 20% of patients and by culture in 52% to 89% of individuals, whereas transbronchial biopsy specimens result in positive AFB smears in 10% to 39% of patients and in positive cultures in 42% to 85% of individuals.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







