Chapter 5
Sedation and Analgesia during Mechanical Ventilation 
Analgesic and sedation needs vary widely in mechanically ventilated patients. Pain thresholds, anxiety levels, and noxious exposures are highly variable among patients. Furthermore, drugs administered to ICU patients frequently exhibit a wide range of pharmacokinetics and pharmacodynamics because of renal and hepatic dysfunction, drug interactions, low protein states, and shock (Chapter 17). As a result, analgesic and sedative drugs cannot be administered with a “one size fits all” approach. Instead, they should be titrated to discernible and reproducible clinical end points. Drugs used in this context are extremely potent, so clinicians must have heightened awareness of the potential for enduring effects and are encouraged to employ strategies that maximize symptom control while minimizing risk.
Data from both observational and randomized controlled trials demonstrate that sedation strategies can significantly impact both short- and long-term patient outcomes. When executed poorly, patients may suffer from extended delirium, excessive neurologic diagnostic testing, hemodynamic instability, prolongation of assisted ventilation, complications associated with immobility (e.g., joint contractures, sacral ulcers), and higher risk for psychiatric illnesses like posttraumatic stress disorder. In contrast, protocols with standardized symptom assessments that guide drug titration (for example, see Figure 37-E4) have yielded more patient days spent awake, shortened duration of mechanical ventilation, and reduced ICU and hospital lengths of stay. Additionally, selected studies of sedation (and exercise) protocols have improved physical and cognitive recovery, psychological well-being, and potentially survival.
Distress and Agitation
Attention to dyspnea as an isolated cause for distress has intensified. Presentations span subjective complaints, elevated work of breathing, and severe ventilator asynchrony. These latter findings are particularly common in nontraditional ventilation strategies (low tidal volumes, permissive hypercapnia, and high-frequency oscillatory ventilation), which may contradict the body’s usual response to stress. Modulating inspiratory flow rates to match neural demand, augmenting respiratory rates, or changing the mode of ventilation, such as from assist-control to pressure support, may relieve dyspnea in some instances (see Chapters 2, 3, and 47). Additionally, patients may express prominent dyspnea during weaning from prolonged mechanical ventilation (Chapter 25). Unfortunately, this may be unavoidable in patients with respiratory muscle weakness and advanced lung injury. Drug administration to facilitate tolerance is common in all of these scenarios.
Delirium is defined as an acute, reversible disturbance of consciousness and cognitive function that fluctuates in severity (Chapter 37). Its characteristics include defective perception, reduced short-term memory, confusion, disorientation, and, on occasion, hallucinations. Delirium is more recognizable when manifest as agitation; drug treatment to date has focused on managing the agitated state and avoiding self-harm. Hallmarks of agitation are repetitive, nonproductive movements. It is the most obvious, and dangerous, manifestation of distress. Akin to untreated pain, agitation can exert substantial oxygen consumption, risk myocardial ischemia and tachyarrhythmias, and result in patient self-injury via removal of life-sustaining devices.
Assessment of the Patient with Distress or Agitation
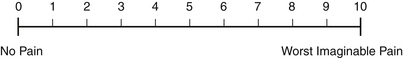
Assessing for distress and agitation should be a routine component of the bedside evaluation of patients. Semiquantitative scales, such as a visual analog pain scale (Figure 5.1), a behavioral pain scale (Table 5.1), and depth of sedation and severity of agitation (Table 5.2), should be used to facilitate communication among all ICU clinicians and to document the patient’s status on the ICU flow sheet. The implementation of a regular and systematic assessment of distress with a consistent scale has been proven to minimize the amount of sedation necessary and speeds the recovery of the patient from a sedated state.
TABLE 5.1
Behavioral Pain Scale for Assessing Pain in Noncommunicative, Mechanically Ventilated Adults
| Item | Description | Score |
| Facial expression | Relaxed Partially tightened (e.g., brow lowering) Fully tightened (e.g., eyelid closing) Grimacing | 1 2 3 4 |
| Upper limb movements | No movement Partially bent Fully bent with finger flexion Permanently retracted | 1 2 3 4 |
| Compliance with mechanical ventilation | Tolerating movement Coughing but tolerating ventilation for most of the time Fighting ventilator Unable to control ventilation | 1 2 3 4 |
Adapted from Payen JF, Bru O, Bosson JL, et al: Assessing pain in critically ill sedated patients by using a behavioral pain scale. Crit Care Med 29(12):2258-2263, 2001.
TABLE 5.2
The Richmond Agitation and Sedation Scale: The RASS∗
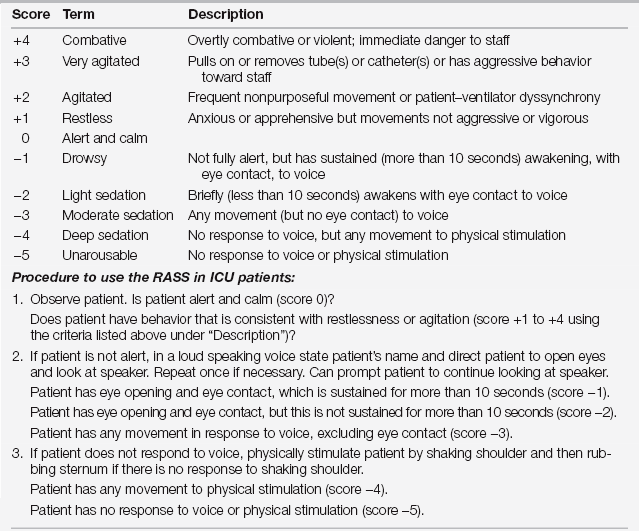
∗Modified from Sessler CN, Gosnell M, Grap MJ, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care patients. Am J Respir Crit Care Med 166:1338-1344, 2002; and Ely EW, Truman B, Shintani A, et al: Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 289:2983-2991, 2003.
In general, evaluation should begin with observation of the patient’s spontaneous interaction with the environment, including wakefulness, physical activity, and work of breathing coupled with ventilator synchrony. Intermittent mild agitation and breath stacking does not necessarily require pharmacologic suppression and can be a healthy response to avoid the dangers of strict bed rest and diaphragm passivity. Furthermore, nurses and physical therapists can harness this energy into exercise and mobilization. In contrast, severe agitation—which can be precipitous and unexpected—threatens placement of vascular catheters and access tubes. It can severely compromise respiratory and cardiovascular life support, increasing oxygen demand and generating carbon dioxide and lactic acid. Immediate assessment and intervention are necessary.
If, on examination, patients are not immediately awake, the clinician should attempt to engage them by voice alone. Should a response occur, one should briefly reassure patients of their location and inability to talk. Thereafter, one can ask the patients to follow a series of simple commands, such as opening their eyes and protruding their tongue. Facial gestures are optimal as advanced ICU-acquired weakness usually spares the facial neuromuscular axis (Chapter 48).
Further questioning should focus efforts on determining pain and other causes for distress. Use direct questions that intubated patients can answer “yes” or “no”; lip reading can be difficult and risks frustration for both the distressed patient and the clinician. Inconsistent responses and attention should prompt reassessment for delirium. If a patient is experiencing pain, anxiety, or dyspnea, the severity of distress should be evaluated on a scale of 0 to 10—for example, using a visual analog pain scale (see Figure 5.1). Quantitation of distress determines the urgency of treatment and guides drug dosing. These self-reports of pain are more reliable than the use of behavioral scales necessitated by the noncommunicative patient (Table 5.1). In contrast, vital signs are not reliable indicators for pain or control of distress, but they can guide clinicians to assess or reassess.
General Treatment Guidelines
At the outset of each day, the patient’s nurse, physician, and (ideally) ICU pharmacist should agree on a desired goal of sedation depth and pain control for the day. A reliable standardized approach to describe depth of sedation is to use the Richmond Agitation and Sedation Score (RASS) shown in Table 5.2. In the earliest days of a patient’s respiratory failure, this goal may be a moderate sedation depth—for example, a nonsustained eye opening to voice (e.g., RASS −2 to −3)—to facilitate ventilator synchrony and keep extra oxygen consumption to a minimum. As the patient recovers, a goal for an awake patient (e.g., RASS −1 to +1) is the standard. The ICU team should outline the agents for both persistent, moderate distress/agitation and optimal drug(s) for immediate rescue.
In general, in patients previously unexposed to opioids, one can begin with low-dose, intermittent fentanyl, for example, 50 μg intravenous (IV) bolus, or another opioid of preference (Table 5.3). Frequent boluses should prompt consideration for initiating an infusion. One should titrate the dose to effect by giving additional bolus doses followed by increases in the maintenance infusion rate. As the infusion dose escalates, consider adding a sedative like propofol—ideally generating synergistic effects and less toxicity from each individual agent (Table 5.4).
TABLE 5.3
Intravenous (IV) Opioids Commonly Used during Mechanical Ventilation
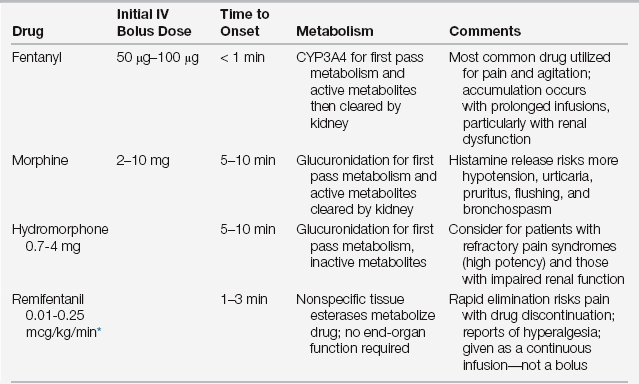
∗= 0.6-15 mcg/kg/h given as a continuous infusion (no bolus)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree