Chapter 43
Skin Rashes
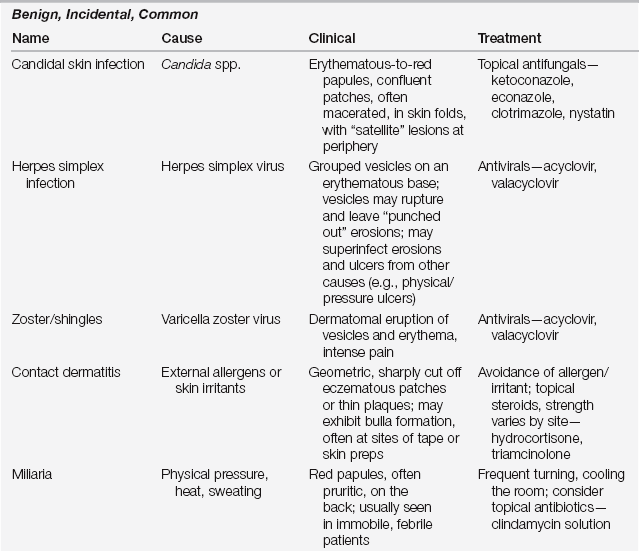
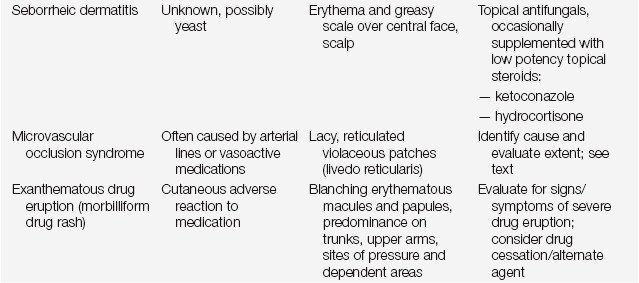
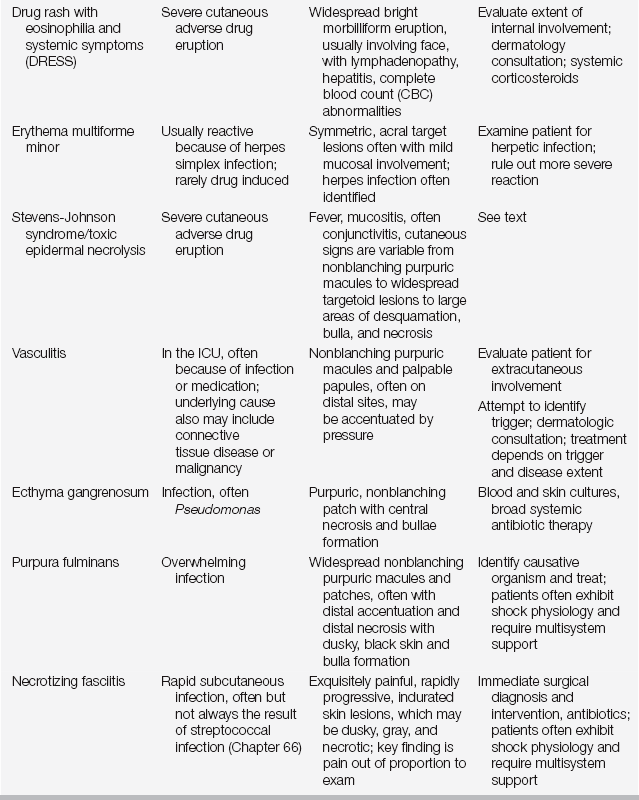
Common Benign Skin Rashes (Table 43.1)
Contact Dermatitis
Contact dermatitis occurs from the interaction of a chemical with the skin. There are two major forms: irritant and allergic. Irritant contact dermatitis accounts for 80% of cases and results from damage to the skin via a toxic effect intrinsic to the compound; these irritants react with any skin and do not require prior sensitization. Common irritants in the ICU are soaps, stool, and urine, which when left in prolonged contact with the skin cause direct toxicity. These reactions typically occur within minutes to hours of the exposure, depending on the concentration of the irritant and the integrity of the skin.
Allergic contact dermatitis, a type IV cell-mediated delayed hypersensitivity immune response (see also Table 32.1 in Chapter 32), accounts for the other 20% of cases. It is antigen specific, and the reaction requires prior sensitization. In the ICU, patients may become sensitized to a variety of topical preparations, such as iodine, topical antimicrobials, or the adhesives used in tape or electrodes.
Herpes Zoster
Herpes zoster, also known as shingles, is a vesicular eruption that occurs in a dermatomal distribution. Herpes zoster is caused by the reactivation of latent varicella zoster virus (VZV), which lays dormant in sensory neurons. Age and immunosuppression are the main risk factors for reactivation. The development of a zoster vaccine may eventually decrease cases in the elderly. Clinically, vesicles are seen on an erythematous base, distributed unilaterally in a dermatome, most commonly on the trunk (see Figure 101.1 in Chapter 101 for a discussion of sensory dermatomes). Occasionally the lesions become hemorrhagic; frequently they evolve to crusted erosions and then heal over the course of 2 to 3 weeks. Burning, stinging, itching, or pain often precedes the cutaneous manifestations. Up to 20 lesions can be found outside the affected dermatome, but a more extensive spread of lesions warrants prompt investigation for signs of disseminated varicella infection.
Initiate antiviral therapy as soon as possible, optimally within the first 72 hours of disease. Antiviral therapy promotes lesion healing and recovery, and it also decreases the risk of postzoster pain syndromes. Valacyclovir and famciclovir are preferable to acyclovir. Given that zoster is seen frequently in elderly patients, appropriate dosing for age-adjusted renal function is essential. Local therapy with heat pads, pressure, and support may provide additional relief; and gabapentin use may reduce the risk of post-zoster pain. Intravenous therapy is occasionally necessary for the immunocompromised patient and is always required for disseminated disease.
Drug Reactions
Morbilliform Drug Rash
The most common drug reaction seen is a morbilliform eruption; this morphologic pattern comprises up to 90% of all cutaneous adverse drug reactions. Classically, patients present with erythematous macules and papules. Lesions may exhibit preference for dependent areas and sites of pressure or friction such as elastic bands, adhesives, areas of skin-on-skin rubbing, and the sacral region. Mucosal surfaces should be examined for involvement, which may portend a more serious drug reaction.
This reaction typically takes place 4 to 14 days after starting a new medication and is presumed to be a type IV hypersensitivity reaction, although the immunologic pathophysiology has not been completely elucidated. A thorough query of the patient’s medication history is essential to try to determine the most likely causative agent. Because it is difficult to identify the inciting agent accurately, discontinue any nonessential drugs. In limited eruptions with no concerning features (worrisome features include involvement of mucosal surfaces, skin pain, blistering, necrosis, or progression to involve sites typically spared, such as acral surfaces) some cases of morbilliform drug eruptions can be managed conservatively, and it may be possible to continue administering the causative agent if the implicated drug is essential to the patients’ care. In the majority of cases, however, it is better to discontinue the suspect medication and note the allergy in the patient’s medical record. One should perform daily cutaneous examinations to watch for progression. The drugs most frequently associated with morbilliform eruptions include allopurinol, aminopenicillins, cephalosporins, antiepileptic drugs, and antibacterial sulfonamides (see Chapter 32).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree