Key Concepts
 Next to the supine position, the lithotomy position is the most commonly used position for patients undergoing urological and gynecological procedures. Failure to properly position and pad the patient can result in pressure sores, nerve injuries, or compartment syndromes.
Next to the supine position, the lithotomy position is the most commonly used position for patients undergoing urological and gynecological procedures. Failure to properly position and pad the patient can result in pressure sores, nerve injuries, or compartment syndromes.
 The lithotomy position is associated with major physiological alterations. Functional residual capacity decreases, predisposing patients to atelectasis and hypoxia. Elevation of the legs drains blood into the central circulation acutely. Mean blood pressure often increases, but cardiac output does not change significantly. Conversely, rapid lowering of the legs from the lithotomy or Trendelenburg position acutely decreases venous return and can result in hypotension. Blood pressure measurement should be taken immediately after the legs are lowered.
The lithotomy position is associated with major physiological alterations. Functional residual capacity decreases, predisposing patients to atelectasis and hypoxia. Elevation of the legs drains blood into the central circulation acutely. Mean blood pressure often increases, but cardiac output does not change significantly. Conversely, rapid lowering of the legs from the lithotomy or Trendelenburg position acutely decreases venous return and can result in hypotension. Blood pressure measurement should be taken immediately after the legs are lowered.
 Because of the short duration (15-20 min) and outpatient setting of most cystoscopies, general anesthesia is often chosen, commonly employing a laryngeal mask airway.
Because of the short duration (15-20 min) and outpatient setting of most cystoscopies, general anesthesia is often chosen, commonly employing a laryngeal mask airway.
 Both epidural and spinal blockade with a T10 sensory level provide excellent anesthesia for cystoscopy.
Both epidural and spinal blockade with a T10 sensory level provide excellent anesthesia for cystoscopy.
 Manifestations of TURP (transurethral resection of the prostate) syndrome are primarily those of circulatory fluid overload, water intoxication, and, occasionally, toxicity from the solute in the irrigating fluid.
Manifestations of TURP (transurethral resection of the prostate) syndrome are primarily those of circulatory fluid overload, water intoxication, and, occasionally, toxicity from the solute in the irrigating fluid.
 Absorption of TURP irrigation fluid is dependent on the duration of the resection and the pressure of the irrigation fluid.
Absorption of TURP irrigation fluid is dependent on the duration of the resection and the pressure of the irrigation fluid.
 When compared with general anesthesia, regional anesthesia for TURP may reduce the incidence of postoperative venous thrombosis. It is also less likely to mask symptoms and signs of TURP syndrome or bladder perforation.
When compared with general anesthesia, regional anesthesia for TURP may reduce the incidence of postoperative venous thrombosis. It is also less likely to mask symptoms and signs of TURP syndrome or bladder perforation.
 Patients with a history of cardiac arrhythmias and those with a pacemaker or internal cardiac defibrillator (ICD) may be at risk for developing arrhythmias induced by shock waves during extracorporeal shock wave lithotripsy (ESWL). Shock waves can damage the internal components of pacemaker and ICD devices.
Patients with a history of cardiac arrhythmias and those with a pacemaker or internal cardiac defibrillator (ICD) may be at risk for developing arrhythmias induced by shock waves during extracorporeal shock wave lithotripsy (ESWL). Shock waves can damage the internal components of pacemaker and ICD devices.
 Patients who are undergoing retroperitoneal lymph node dissection and who have received bleomycin preoperatively are at increased risk for developing postoperative pulmonary insufficiency. These patients may be particularly at risk for oxygen toxicity and fluid overload, and for developing acute respiratory distress syndrome postoperatively.
Patients who are undergoing retroperitoneal lymph node dissection and who have received bleomycin preoperatively are at increased risk for developing postoperative pulmonary insufficiency. These patients may be particularly at risk for oxygen toxicity and fluid overload, and for developing acute respiratory distress syndrome postoperatively.
 For patients undergoing renal transplantation, the preoperative serum potassium concentration should be below 5.5 mEq/L and existing coagulopathies should be corrected. Hyperkalemia has been reported after release of the vascular clamp following completion of the arterial anastomosis, particularly in pediatric and other small patients. Release of potassium contained in the preservative solution has been implicated as the cause of this phenomenon.
For patients undergoing renal transplantation, the preoperative serum potassium concentration should be below 5.5 mEq/L and existing coagulopathies should be corrected. Hyperkalemia has been reported after release of the vascular clamp following completion of the arterial anastomosis, particularly in pediatric and other small patients. Release of potassium contained in the preservative solution has been implicated as the cause of this phenomenon.
Anesthesia for Genitourinary Surgery: Introduction
Urological procedures account for 10-20% of most anesthetic practices. Patients undergoing genitourinary procedures may be of any age, but many are elderly with coexisting medical illnesses, commonly renal dysfunction. The impact of anesthesia on renal function is discussed in Chapter 30. This chapter reviews the anesthetic management of common urological procedures. Use of the lithotomy and steep head-down (Trendelenburg) positions, the transurethral approach, and extracorporeal shock waves (lithotripsy) complicates many of these procedures. Moreover, advances in surgical technique and perioperative medical and surgical management allow more patients with coexisting disease to be considered acceptable candidates for renal transplantation and for extensive tumor debulking and reconstructive genitourinary procedures involving marked physiological trespass.
Cystoscopy is the most commonly performed urological procedure, and indications for this investigative or therapeutic operation include hematuria, recurrent urinary infections, renal calculi, and urinary obstruction. Bladder biopsies, retrograde pyelograms, transurethral resection of bladder tumors, extraction or laser lithotripsy of renal stones, and placement or manipulation of ureteral catheters (stents) are also commonly performed through the cystoscope.
Anesthetic management varies with the age and gender of the patient and the purpose of the procedure. General anesthesia is usually necessary for children. Viscous lidocaine topical anesthesia with or without sedation is satisfactory for diagnostic studies in most women because of the short urethra. Operative cystoscopies involving biopsies, cauterization, or manipulation of ureteral catheters require regional or general anesthesia. Many men prefer regional or general anesthesia even for diagnostic cystoscopy.
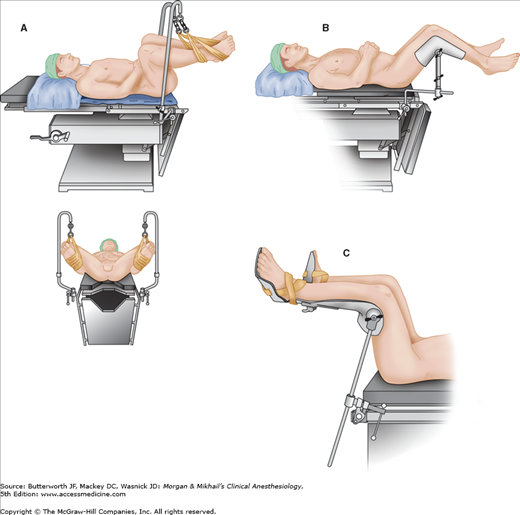
 Next to the supine position, the lithotomy position is the most commonly used position for patients undergoing urological and gynecological procedures. Failure to properly position and pad the patient can result in pressure sores, nerve injuries, or compartment syndromes. Two people are needed to safely move the patient’s legs simultaneously up into, or down from, the lithotomy position. Straps around the ankles or special holders support the legs in lithotomy position (Figure 31-1). The leg supports should be padded wherever there is leg or foot contact, and straps must not impede circulation. When the patient’s arms are tucked to the side, caution must be exercised to prevent the fingers from being caught between the mid and lower sections of the operating room table when the lower section is lowered and raised—many clinicians completely encase the patient’s hands and fingers with protective padding to minimize this risk. Injury to the tibial (common peroneal) nerve, resulting in loss of dorsiflexion of the foot, may result if the lateral knee rests against the strap support. If the legs are allowed to rest on medially placed strap supports, compression of the saphenous nerve can result in numbness along the medial calf. Excessive flexion of the thigh against the groin can injure the obturator and, less commonly, the femoral nerves. Extreme flexion at the thigh can also stretch the sciatic nerve. The most common nerve injuries directly associated with the lithotomy position involve the lumbosacral plexus. Brachial plexus injuries can likewise occur if the upper extremities are inappropriately positioned (eg, hyperextension at the axilla). Compartment syndrome of the lower extremities with rhabdomyolysis has been reported with prolonged time in the lithotomy position, after which lower extremity nerve damage is also more likely.
Next to the supine position, the lithotomy position is the most commonly used position for patients undergoing urological and gynecological procedures. Failure to properly position and pad the patient can result in pressure sores, nerve injuries, or compartment syndromes. Two people are needed to safely move the patient’s legs simultaneously up into, or down from, the lithotomy position. Straps around the ankles or special holders support the legs in lithotomy position (Figure 31-1). The leg supports should be padded wherever there is leg or foot contact, and straps must not impede circulation. When the patient’s arms are tucked to the side, caution must be exercised to prevent the fingers from being caught between the mid and lower sections of the operating room table when the lower section is lowered and raised—many clinicians completely encase the patient’s hands and fingers with protective padding to minimize this risk. Injury to the tibial (common peroneal) nerve, resulting in loss of dorsiflexion of the foot, may result if the lateral knee rests against the strap support. If the legs are allowed to rest on medially placed strap supports, compression of the saphenous nerve can result in numbness along the medial calf. Excessive flexion of the thigh against the groin can injure the obturator and, less commonly, the femoral nerves. Extreme flexion at the thigh can also stretch the sciatic nerve. The most common nerve injuries directly associated with the lithotomy position involve the lumbosacral plexus. Brachial plexus injuries can likewise occur if the upper extremities are inappropriately positioned (eg, hyperextension at the axilla). Compartment syndrome of the lower extremities with rhabdomyolysis has been reported with prolonged time in the lithotomy position, after which lower extremity nerve damage is also more likely.
 The lithotomy position is associated with major physiological alterations. Functional residual capacity decreases, predisposing patients to atelectasis and hypoxia. This effect is amplified by steep Trendelenburg positioning (>30°), which is commonly utilized in combination with the lithotomy position. Elevation of the legs drains blood into the central circulation acutely and may thereby exacerbate congestive heart failure (or treat a relative hypovolemia). Mean blood pressure and cardiac output may increase. Conversely, rapid lowering of the legs from the lithotomy or Trendelenburg position acutely decreases venous return and can result in hypotension. Vasodilation from either general or regional anesthesia potentiates the hypotension in this situation, and for this reason, blood pressure measurement should be taken immediately after the legs are lowered.
The lithotomy position is associated with major physiological alterations. Functional residual capacity decreases, predisposing patients to atelectasis and hypoxia. This effect is amplified by steep Trendelenburg positioning (>30°), which is commonly utilized in combination with the lithotomy position. Elevation of the legs drains blood into the central circulation acutely and may thereby exacerbate congestive heart failure (or treat a relative hypovolemia). Mean blood pressure and cardiac output may increase. Conversely, rapid lowering of the legs from the lithotomy or Trendelenburg position acutely decreases venous return and can result in hypotension. Vasodilation from either general or regional anesthesia potentiates the hypotension in this situation, and for this reason, blood pressure measurement should be taken immediately after the legs are lowered.
Many patients are apprehensive about the procedure and prefer to be asleep. However, any anesthetic technique suitable for outpatients may be utilized.  Because of the short duration (15-20 min) and outpatient setting of most cystoscopies, general anesthesia is often chosen, commonly employing a laryngeal mask airway. Oxygen saturation should be closely monitored when obese or elderly patients, or those with marginal pulmonary reserve, are placed in the lithotomy or Trendelenburg position.
Because of the short duration (15-20 min) and outpatient setting of most cystoscopies, general anesthesia is often chosen, commonly employing a laryngeal mask airway. Oxygen saturation should be closely monitored when obese or elderly patients, or those with marginal pulmonary reserve, are placed in the lithotomy or Trendelenburg position.
 Both epidural and spinal blockade provide satisfactory anesthesia for cystoscopy. However, when regional anesthesia is chosen most anesthesiologists prefer spinal anesthesia because onset of satisfactory sensory blockade may require 15-20 min for epidural anesthesia compared with 5 min or less for spinal anesthesia. Some clinicians believe that the sensory level following injection of a hyperbaric spinal anesthetic solution should be well established (“fixed”) before the patient is moved into the lithotomy position; however, studies fail to demonstrate that immediate elevation of the legs into lithotomy position following administration of hyperbaric spinal anesthesia either increases the dermatomal extent of anesthesia to a clinically significant degree or increases the likelihood of severe hypotension. A sensory level to T10 provides excellent anesthesia for essentially all cystoscopic procedures.
Both epidural and spinal blockade provide satisfactory anesthesia for cystoscopy. However, when regional anesthesia is chosen most anesthesiologists prefer spinal anesthesia because onset of satisfactory sensory blockade may require 15-20 min for epidural anesthesia compared with 5 min or less for spinal anesthesia. Some clinicians believe that the sensory level following injection of a hyperbaric spinal anesthetic solution should be well established (“fixed”) before the patient is moved into the lithotomy position; however, studies fail to demonstrate that immediate elevation of the legs into lithotomy position following administration of hyperbaric spinal anesthesia either increases the dermatomal extent of anesthesia to a clinically significant degree or increases the likelihood of severe hypotension. A sensory level to T10 provides excellent anesthesia for essentially all cystoscopic procedures.
Benign prostatic hyperplasia (BPH) frequently leads to bladder outlet obstruction in men older than 60 years. Although increasingly being treated medically, some men require surgical intervention. Transurethral resection of the prostate (TURP) is the most common surgical procedure performed for bladder outlet obstruction due to BPH, and indications for TURP in this setting include obstructive uropathy, bladder calculi, and recurrent episodes of urinary retention, urinary tract infections, and hematuria. Patients with adenocarcinoma of the prostate may also benefit from TURP to relieve symptomatic urinary obstruction.
TURP requires regional or general anesthesia, and patients should be evaluated for coexistent major organ dysfunction. Despite advanced age (over half of TURP patients are older than 70 years) and prevalence of significant comorbidity in over two thirds of TURP patients, perioperative mortality and medical morbidity (most frequently myocardial infarction, pulmonary edema, and kidney failure) for this procedure are both less than 1%.
The most common surgical complications of TURP are clot retention, failure to void, uncontrolled hematuria requiring surgical revision, urinary tract infection, and chronic hematuria, although other, more rare, complications may include: TURP syndrome, bladder perforation, sepsis, hypothermia, and disseminated intravascular coagulation (DIC). A blood type and screen (see Chapter 51) is adequate for most patients, although crossmatched blood should be available for anemic patients and for patients with large glands in which extensive resection is contemplated. Prostatic bleeding can be difficult to control through the cystoscope.
TURP is performed by passing a loop through a special cystoscope (resectoscope). Using continuous irrigation and direct visualization, prostatic tissue is resected by applying a cutting current to the loop. Because of the characteristics of the prostate and the large amounts of irrigation fluid often used, TURP can be associated with a number of serious complications (Table 31-1).
|
|
Transurethral prostatic resection often opens the extensive network of venous sinuses in the prostate, potentially allowing systemic absorption of the irrigating fluid. The absorption of large amounts of fluid (2 L or more) results in a constellation of symptoms and signs commonly referred to as the TURP syndrome (Table 31-2). This syndrome presents intraoperatively or postoperatively as headache, restlessness, confusion, cyanosis, dyspnea, arrhythmias, hypotension, or seizures, and it can be rapidly fatal.  The manifestations are primarily those of circulatory fluid overload, water intoxication, and, occasionally, toxicity from the solute in the irrigating fluid. The incidence of TURP syndrome is less than 1%.
The manifestations are primarily those of circulatory fluid overload, water intoxication, and, occasionally, toxicity from the solute in the irrigating fluid. The incidence of TURP syndrome is less than 1%.
|
Electrolyte solutions cannot be used for irrigation during TURP because they disperse the electrocautery current. Water provides excellent visibility because its hypotonicity lyses red blood cells, but significant water absorption can readily result in acute water intoxication. Water irrigation is generally restricted to transurethral resection of bladder tumors only. For TURP, slightly hypotonic nonelectrolyte irrigating solutions such as glycine 1.5% (230 mOsm/L) or a mixture of sorbitol 2.7% and mannitol 0.54% (195 mOsm/L) are most commonly used. Less commonly used solutions include sorbitol 3.3%, mannitol 3%, dextrose 2.5-4%, and urea 1%. Because all these fluids are still hypotonic, significant absorption of water can nevertheless occur. Solute absorption can also occur because the irrigation fluid is under pressure, and high irrigation pressures (bottle height) increase fluid absorption.
 Absorption of TURP irrigation fluid is dependent on the duration of the resection and the pressure of the irrigation fluid. Most resections last 45-60 min, and, on average, 20 mL/min of the irrigating fluid is absorbed. Pulmonary congestion or florid pulmonary edema can readily result from the absorption of large amounts of irrigation fluid, particularly in patients with limited cardiac reserve. The hypotonicity of these fluids also results in acute hyponatremia and hypoosmolality, which can lead to serious neurological manifestations. Symptoms of hyponatremia usually do not develop until the serum sodium concentration decreases below 120 mEq/L. Marked hypotonicity in plasma ([Na+] <100 mEq/L) may also result in acute intravascular hemolysis.
Absorption of TURP irrigation fluid is dependent on the duration of the resection and the pressure of the irrigation fluid. Most resections last 45-60 min, and, on average, 20 mL/min of the irrigating fluid is absorbed. Pulmonary congestion or florid pulmonary edema can readily result from the absorption of large amounts of irrigation fluid, particularly in patients with limited cardiac reserve. The hypotonicity of these fluids also results in acute hyponatremia and hypoosmolality, which can lead to serious neurological manifestations. Symptoms of hyponatremia usually do not develop until the serum sodium concentration decreases below 120 mEq/L. Marked hypotonicity in plasma ([Na+] <100 mEq/L) may also result in acute intravascular hemolysis.
Toxicity may also arise from absorption of the solutes in these fluids. Marked hyperglycinemia has been reported with glycine solutions and may contribute to circulatory depression and central nervous system toxicity. Plasma glycine concentrations in excess of 1000 mg/L have been recorded (normal is 13-17 mg/L). Glycine is known to be an inhibitory neurotransmitter in the central nervous system and has also been implicated in rare instances of transient blindness following TURP. Hyperammonemia, presumably from the degradation of glycine, has also been documented in a few patients with marked central nervous system toxicity following TURP. Blood ammonia levels in some patients exceeded 500 μmol/L (normal is 5-50 μmol/L). The use of large amounts of sorbitol or dextrose irrigating solutions can lead to hyperglycemia, which can be marked in diabetic patients. Absorption of mannitol solutions causes intravascular volume expansion and exacerbates fluid overload.
Treatment of TURP syndrome depends on early recognition and should be based on the severity of the symptoms. The absorbed water must be eliminated, and hypoxemia and hypoperfusion treated. Most patients can be managed with fluid restriction and intravenous administration of furosemide. Symptomatic hyponatremia resulting in seizures or coma should be treated with hypertonic saline (see Chapter 49). Seizure activity can be terminated with small doses of midazolam (2-4 mg). Phenytoin, 10-20 mg/kg intravenously (no faster than 50 mg/min), should also be considered to provide more sustained anticonvulsant activity. Endotracheal intubation may be considered to prevent aspiration until the patient’s mental status normalizes. The amount and rate of hypertonic saline solution (3% or 5%) needed to correct the hyponatremia to a safe level should be based on the patient’s serum sodium concentration (see Chapter 49). The rate of hypertonic saline solution administration should be sufficiently slow as to not exacerbate circulatory fluid overload.
Large volumes of irrigating fluids at room temperature can be a major source of heat loss in patients. Irrigating solutions should be warmed to body temperature prior to use to prevent hypothermia. Postoperative shivering associated with hypothermia may dislodge clots and promote postoperative bleeding, as well as add deleterious physiological stress to the patient with coexisting cardiopulmonary disease.
The incidence of bladder perforation during TURP is less than 1%. Perforation may result from the resectoscope going through the bladder wall or from overdistention of the bladder with irrigation fluid. Most bladder perforations are extraperitoneal and are signaled by poor return of the irrigating fluid. Awake patients will typically complain of nausea, diaphoresis, and retropubic or lower abdominal pain. Large extraperitoneal and most intraperitoneal perforations are usually even more obvious, presenting as sudden unexplained hypotension or hypertension, and with generalized abdominal pain in awake patients. Regardless of the anesthetic technique employed, perforation should be suspected in settings of sudden hypotension or hypertension, particularly with acute, vagally mediated bradycardia.
DIC has on rare occasion been reported following TURP and may result from the release of thromboplastins from prostate tissue into the circulation during the procedure. Up to 6% of patients may have evidence of subclinical DIC. A dilutional thrombocytopenia can also develop during surgery as part of the TURP syndrome from absorption of irrigation fluids. Rarely, patients with metastatic carcinoma of the prostate develop a coagulopathy from primary fibrinolysis due to secretion of a fibrinolytic enzyme. The diagnosis of coagulopathy may be suspected from diffuse, uncontrollable bleeding but must be confirmed by laboratory tests. Primary fibrinolysis should be treated with ϵ-aminocaproic acid (Amicar), 5 g followed by 1 g/h intravenously. Treatment of DIC in this setting may require heparin in addition to replacement of clotting factors and platelets, and consultation with a hematologist should be considered.
The prostate is often colonized with bacteria and may harbor chronic infection. Extensive surgical resection with the opening of venous sinuses can allow entry of organisms into the bloodstream. Bacteremia following transurethral surgery is common and can lead to septicemia or septic shock. Prophylactic antibiotic therapy (most commonly gentamicin, levofloxacin, or cefazolin) prior to TURP may decrease the likelihood of bacteremic and septic episodes.
Either spinal or epidural anesthesia with a T10 sensory level, or general anesthesia, provides excellent anesthesia and good operating conditions for TURP.  When compared with general anesthesia, regional anesthesia may reduce the incidence of postoperative venous thrombosis. It is also less likely to mask symptoms and signs of TURP syndrome or bladder perforation. Clinical studies have failed to show any differences in blood loss, postoperative cognitive function, and mortality between regional and general anesthesia. The possibility of vertebral metastasis must be considered in patients with carcinoma, particularly those with back pain, as metastatic disease involving the lumbar spine is a relative contraindication to spinal or epidural anesthesia. Acute hyponatremia from TURP syndrome may delay or prevent emergence from general anesthesia.
When compared with general anesthesia, regional anesthesia may reduce the incidence of postoperative venous thrombosis. It is also less likely to mask symptoms and signs of TURP syndrome or bladder perforation. Clinical studies have failed to show any differences in blood loss, postoperative cognitive function, and mortality between regional and general anesthesia. The possibility of vertebral metastasis must be considered in patients with carcinoma, particularly those with back pain, as metastatic disease involving the lumbar spine is a relative contraindication to spinal or epidural anesthesia. Acute hyponatremia from TURP syndrome may delay or prevent emergence from general anesthesia.
Evaluation of mental status in the awake or moderately sedated patient is the best monitor for detection of early signs of TURP syndrome and bladder perforation. Tachycardia or decrease in arterial oxygen saturation may be an early sign of fluid overload. Perioperative ischemic electrocardiographic changes have been reported in up to 18% of patients. Temperature monitoring is standard of care for general anesthesia, and it should also be used in cases of lengthy resections under spinal or epidural anesthesia to detect hypothermia. Blood loss is particularly difficult to assess during TURP because of the use of irrigating solutions, so it is necessary to rely on clinical signs of hypovolemia (see Chapter 51). Blood loss averages approximately 3-5 mL/min of resection (usually 200-300 mL total) but is rarely life-threatening. Transient, postoperative decreases in hematocrit may simply reflect hemodilution from absorption of irrigation fluid. Less than 2% of patients require intraoperative blood transfusion; factors associated with need for transfusion include procedure duration longer than 90 min and resection of more than 45 g of prostate tissue.
The treatment of kidney stones has evolved from primarily open surgical procedures to less invasive or entirely noninvasive techniques. Cystoscopic procedures, including flexible ureteroscopy with stone extraction, stent placement, and intracorporeal lithotripsy (laser or electrohydraulic), along with medical expulsive therapy (MET), have become first-line therapy. Extracorporeal shock wave lithotripsy (ESWL) is also utilized, primarily for 4-mm to 2-cm intrarenal stones, and percutaneous and laparoscopic nephrolithotomy for larger or impacted stones. MET has become the treatment of choice among many clinicians for acute episodes of urolithiasis: for stones up to 10 mm in diameter, administration of the α blockers tamsulosin (Flomax), doxazosin (Cardura), or terazosin (Hytrin) or the calcium channel blocker nifedipine (Procardia, Adalat) lessens the pain of acute urolithiasis and increases the rate of stone expulsion over a period of several days to several weeks.
During ESWL, repetitive high-energy shocks (sound waves) are generated and focused on the stone, causing it to fragment as tensile and shear forces develop inside the stone and cavitation occurs on its surface. Water or a conducting gel couples the generator to the patient. Because tissue has the same acoustic density as water, the waves travel through the body without damaging tissue. However, the change in acoustic impedance at the tissue-stone interface creates shear and tear forces on the stone. Subsequently, the stone is fragmented enough to allow its passage in small pieces down the urinary tract. Ureteral stents are often placed cystoscopically prior to the procedure. Tissue destruction can occur if the acoustic energy is inadvertently focused at air-tissue interfaces such as in the lung and intestine. The inability to position the patient so that lung and intestine are away from the sound wave focus is a contraindication to the procedure. Other contraindications include urinary obstruction below the stone, untreated infection, a bleeding diathesis, and pregnancy. The presence of a nearby aortic aneurysm or an orthopedic prosthetic device is considered a relative contraindication. Ecchymosis, bruising, or blistering of the skin over the treatment site is not uncommon. Rarely, a large perinephric hematoma can develop and may be responsible for a postoperative decrease in hematocrit.
Electrohydraulic, electromagnetic, or piezoelectric shock wave generators may be used for ESWL. With older electrohydraulic units, the patient is placed in a hydraulic chair and immersed in a heated water bath, which conducts the shock waves to the patient. Modern lithotriptors generate shock waves either electromagnetically or from piezoelectric crystals. The generator is enclosed in a water-filled casing and comes in contact with the patient via a conducting gel on a plastic membrane (Figure 31-2). Newer units allow both fluoroscopic and ultrasound localization. In the case of electromagnetic machines, the vibration of a metallic plate in front of an electromagnet produces the shock waves. With piezoelectric models, the waves are the result of changes in the external dimensions of ceramic crystals when electric current is applied.