Introduction
Patients requiring resuscitation often have an obstructed airway, usually caused by loss of consciousness, but occasionally it may be the primary cause of cardiorespiratory arrest. Immediate restoration of airway patency enables ventilation of the lungs and oxygenation of the blood. Without adequate oxygenation it may be impossible to restore a perfusing cardiac rhythm. There is little high-quality evidence to support the use of any specific technique for maintaining an airway in adults with cardiorespiratory arrest. Ventilation is often achieved using a self-inflating bag and a mask (‘bag-mask’), but use of supraglottic airway devices (SADs) may be more effective and reduce the risk of gastric inflation. Tracheal intubation is generally considered to be the optimal method for maintaining a clear airway but it should be attempted only when trained personnel are available to carry out the procedure with a high level of skill and competence.
Causes of airway obstruction
Airway obstruction may be partial or complete. It can occur at any level from the nose and mouth down to the level of the carina and bronchi. In unconscious patients, the commonest site of airway obstruction is at the soft palate and epiglottis and, contrary to popular belief, not the tongue. Vomit or blood, as a result of regurgitation of gastric contents or trauma, or foreign bodies can also cause airway obstruction. Laryngeal obstruction may be caused by oedema from burns, inflammation or anaphylaxis. Upper airway stimulation or inhalation of foreign material may cause laryngeal spasm. Obstruction of the airway below the larynx is less common, but may be caused by excessive bronchial secretions, mucosal oedema, bronchospasm, pulmonary oedema, or aspiration of gastric contents. Extrinsic compression of the airway may also occur above or below the larynx, for example as a result of trauma, haematoma or tumour.
Recognition of airway obstruction
Airway obstruction can be subtle. Use the look, listen and feel approach:
- LOOK for chest and abdominal movements
- LISTEN and FEEL for airflow at the mouth and nose
In partial airway obstruction, air entry is diminished and usually noisy: inspiratory stridor is caused by obstruction at the laryngeal level or above; expiratory wheeze suggests obstruction of the lower airways, which tend to collapse and obstruct during expiration.
Complete airway obstruction in a patient who is making respiratory efforts causes paradoxical chest and abdominal movement, described as ‘see-saw breathing’. During airway obstruction, accessory muscles of respiration are used; there may also be intercostal and subcostal recession and a tracheal tug.
During apnoea, when spontaneous breathing movements are absent, complete airway obstruction is recognised by failure to inflate the lungs during attempted positive pressure ventilation. Airway obstruction must be relieved rapidly otherwise brain injury will start to occur within a few minutes. Initially, give high concentration oxygen during attempts to relieve airway obstruction: as airway patency improves, arterial blood oxygen saturation (SaO2) levels will be restored more rapidly if the inspired oxygen concentration is initially high.
Choking
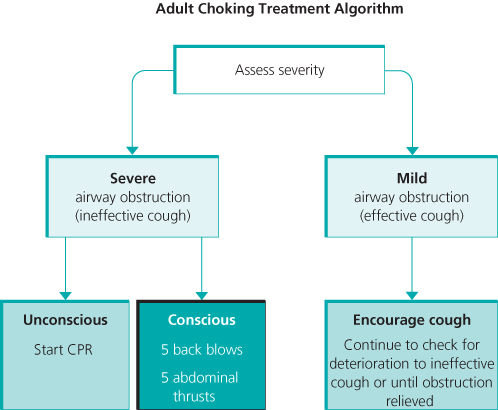
Foreign bodies can cause either mild or severe airway obstruction. The signs and symptoms of mild and severe airway obstruction are summarised in Table 7.1. The appropriate treatment is shown in the adult choking algorithm (Figure 7.1).
Table 7.1 Signs and symptoms of mild and severe airway obstruction
| General signs of choking | Attack occurs while eating Patient may clutch his neck | |
| Signs of airway obstruction | Mild | Severe |
| Response to question ‘Are you choking?’ | Speaks and answers yes | Unable to speak May respond by nodding |
| Other signs | Able to speak, cough and breathe | Unable to breathe Breathing sounds wheezy Attempts at coughing are silent May be unconscious |
Figure 7.1 Adult choking algorithm. Reproduced with the kind permission of the Resuscitation Council (UK).
Basic techniques for opening the airway
The head tilt, chin lift (Figure 7.2) and jaw thrust (Figure 7.3) can be used to relieve upper airway obstruction.
Figure 7.2 Head tilt and chin lift. Photograph reproduced with kind permission by Michael Scott and the Resuscitation Council (UK).

Figure 7.3 Jaw thrust. Photograph reproduced with kind permission by Michael Scott and the Resuscitation Council (UK).

Airway manoeuvres in a patient with suspected cervical spine injury
If spinal injury is suspected, the head, neck, chest and lumbar region are maintained in the neutral position during resuscitation. When there is a risk of cervical spine injury, establish a clear upper airway by using jaw thrust or chin lift in combination with manual in-line stabilisation (MILS) of the head and neck by an assistant. Establishing a patent airway takes priority over concerns about a potential cervical spine injury.
Adjuncts to basic airway techniques
Oropharyngeal and nasopharyngeal airways will overcome soft palate obstruction and backward tongue displacement in an unconscious patient, but head tilt and jaw thrust may also be required. The appropriate size for an oropharyngeal airway corresponds to the vertical distance between the patient’s incisors and the angle of the jaw. In patients who are not deeply unconscious, a nasopharyngeal airway is better tolerated than an oropharyngeal airway; sizes 6–7 mm are suitable for adults.
Oxygen
During CPR, the lungs are ventilated with 100% oxygen until return of a spontaneous circulation (ROSC) is achieved. After ROSC is achieved, high-flow oxygen is given until the SaO2 can be measured reliably. There are animal data indicating an association between high SaO2 (hyperoxaemia) after ROSC and worse outcome. Clinical data from observational studies are conflicting but the current recommendations are that when blood oxygen saturation can be measured reliably, oxygen saturations should be maintained between 94 and 98%; or between 88 and 92% if the patient has chronic obstructive pulmonary disease.
Ventilation
Expired air ventilation (rescue breathing) is effective but the rescuer’s expired oxygen concentration is only 16–17%, so it must be replaced as soon as possible by ventilation with oxygen-enriched air. The pocket resuscitation mask is similar to an anaesthetic face mask and enables mouth-to-mask ventilation. It has a unidirectional valve, which directs the patient’s expired air away from the rescuer. Some masks have a port for the addition of oxygen. When using masks without an oxygen port, supplemental oxygen can be given by placing oxygen tubing underneath one side and ensuring an adequate seal. Tidal volumes in the region of 6–7 ml kg−1 will provide adequate oxygenation and ventilation, while minimising the risk of gastric inflation. Each breath is delivered over approximately 1 s and to a volume that corresponds to normal visible chest movement. During CPR with an unprotected airway, give 2 ventilations after every 30 chest compressions.
Self-inflating bag
The self-inflating bag can be connected to a face mask, tracheal tube, or supraglottic airway device. When used with supplemental oxygen and a reservoir system (usually standard on modern devices) an inspired oxygen concentration of approximately 85% is achieved. Although the bag-mask apparatus enables ventilation with high concentrations of oxygen, its use by a single person requires considerable skill; therefore, the two-person technique is preferable (Figure 7.4).
Figure 7.4 Two-person technique for bag-mask ventilation. Photograph reproduced with kind permission by Michael Scott and the Resuscitation Council (UK).










