Key Concepts
 Improper face mask technique can result in continued deflation of the anesthesia reservoir bag when the adjustable pressure-limiting valve is closed, usually indicating a substantial leak around the mask. In contrast, the generation of high breathing circuit pressures with minimal chest movement and breath sounds implies an obstructed airway or obstructed tubing.
Improper face mask technique can result in continued deflation of the anesthesia reservoir bag when the adjustable pressure-limiting valve is closed, usually indicating a substantial leak around the mask. In contrast, the generation of high breathing circuit pressures with minimal chest movement and breath sounds implies an obstructed airway or obstructed tubing.
 The laryngeal mask airway partially protects the larynx from pharyngeal secretions, but not gastric regurgitation.
The laryngeal mask airway partially protects the larynx from pharyngeal secretions, but not gastric regurgitation.
 After insertion of a tracheal tube (TT), the cuff is inflated with the least amount of air necessary to create a seal during positive-pressure ventilation to minimize the pressure transmitted to the tracheal mucosa.
After insertion of a tracheal tube (TT), the cuff is inflated with the least amount of air necessary to create a seal during positive-pressure ventilation to minimize the pressure transmitted to the tracheal mucosa.
 Although the persistent detection of CO2 by a capnograph is the best confirmation of tracheal placement of a TT, it cannot exclude bronchial intubation. The earliest evidence of bronchial intubation often is an increase in peak inspiratory pressure.
Although the persistent detection of CO2 by a capnograph is the best confirmation of tracheal placement of a TT, it cannot exclude bronchial intubation. The earliest evidence of bronchial intubation often is an increase in peak inspiratory pressure.
 After intubation, the cuff of a TT should not be felt above the level of the cricoid cartilage, because a prolonged intralaryngeal location may result in postoperative hoarseness and increases the risk of accidental extubation.
After intubation, the cuff of a TT should not be felt above the level of the cricoid cartilage, because a prolonged intralaryngeal location may result in postoperative hoarseness and increases the risk of accidental extubation.
 Unrecognized esophageal intubation can produce catastrophic results. Prevention of this complication depends on direct visualization of the tip of the TT passing through the vocal cords, careful auscultation for the presence of bilateral breath sounds and the absence of gastric gurgling while ventilating through the TT, analysis of exhaled gas for the presence of CO2 (the most reliable automated method), chest radiography, or use of fiberoptic bronchoscopy.
Unrecognized esophageal intubation can produce catastrophic results. Prevention of this complication depends on direct visualization of the tip of the TT passing through the vocal cords, careful auscultation for the presence of bilateral breath sounds and the absence of gastric gurgling while ventilating through the TT, analysis of exhaled gas for the presence of CO2 (the most reliable automated method), chest radiography, or use of fiberoptic bronchoscopy.
 Clues to the diagnosis of bronchial intubation include unilateral breath sounds, unexpected hypoxia with pulse oximetry (unreliable with high inspired oxygen concentrations), inability to palpate the TT cuff in the sternal notch during cuff inflation, and decreased breathing bag compliance (high peak inspiratory pressures).
Clues to the diagnosis of bronchial intubation include unilateral breath sounds, unexpected hypoxia with pulse oximetry (unreliable with high inspired oxygen concentrations), inability to palpate the TT cuff in the sternal notch during cuff inflation, and decreased breathing bag compliance (high peak inspiratory pressures).
 The large negative intrathoracic pressures generated by a struggling patient in laryngospasm can result in the development of negative-pressure pulmonary edema even in healthy patients.
The large negative intrathoracic pressures generated by a struggling patient in laryngospasm can result in the development of negative-pressure pulmonary edema even in healthy patients.
Airway Management: Introduction
Expert airway management is an essential skill in anesthetic practice. This chapter reviews the anatomy of the upper respiratory tract: describes the necessary equipment for successful management, presents various management techniques: and discusses complications of laryngoscopy, intubation, and extubation. Patient safety depends on a thorough understanding of each of these topics.
Anatomy
The upper airway consists of the pharynx, nose, mouth, larynx, trachea, and main-stem bronchi. The mouth and pharynx are also a part of the upper gastrointestinal tract. The laryngeal structures in part serve to prevent aspiration into the trachea.
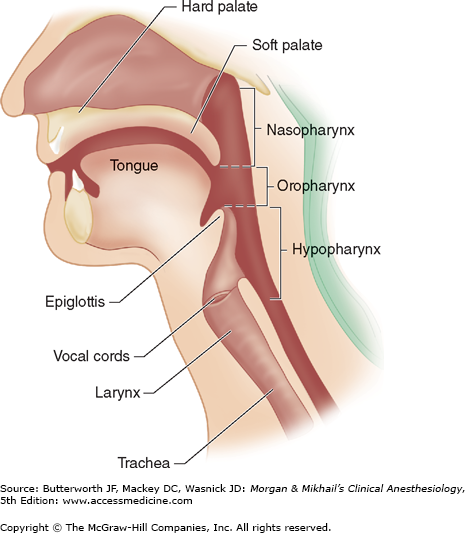
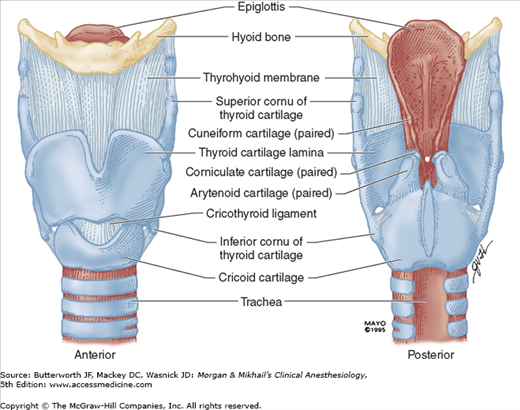
There are two openings to the human airway: the nose, which leads to the nasopharynx, and the mouth, which leads to the oropharynx. These passages are separated anteriorly by the palate, but they join posteriorly in the pharynx (Figure 19-1). The pharynx is a U-shaped fibromuscular structure that extends from the base of the skull to the cricoid cartilage at the entrance to the esophagus. It opens anteriorly into the nasal cavity, the mouth, the larynx, and the nasopharynx, oropharynx, and laryngopharynx, respectively. The nasopharynx is separated from the oropharynx by an imaginary plane that extends posteriorly. At the base of the tongue, the epiglottis functionally separates the oropharynx from the laryngopharynx (or hypopharynx). The epiglottis prevents aspiration by covering the glottis—the opening of the larynx—during swallowing. The larynx is a cartilaginous skeleton held together by ligaments and muscle. The larynx is composed of nine cartilages (Figure 19-2): thyroid, cricoid, epiglottic, and (in pairs) arytenoid, corniculate, and cuneiform. The thyroid cartilage shields the conus elasticus, which forms the vocal cords.
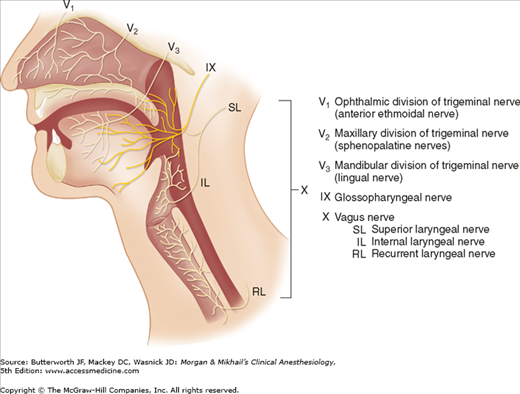
The sensory supply to the upper airway is derived from the cranial nerves (Figure 19-3). The mucous membranes of the nose are innervated by the ophthalmic division (V1) of the trigeminal nerve anteriorly (anterior ethmoidal nerve) and by the maxillary division (V2) posteriorly (sphenopalatine nerves). The palatine nerves provide sensory fibers from the trigeminal nerve (V) to the superior and inferior surfaces of the hard and soft palate. The olfactory nerve (cranial nerve I) innervates the nasal mucosa to provide the sense of smell. The lingual nerve (a branch of the mandibular division [V3] of the trigeminal nerve) and the glossopharyngeal nerve (the ninth cranial nerve) provide general sensation to the anterior two-thirds and posterior one-third of the tongue, respectively. Branches of the facial nerve (VII) and glossopharyngeal nerve provide the sensation of taste to those areas, respectively. The glossopharyngeal nerve also innervates the roof of the pharynx, the tonsils, and the undersurface of the soft palate. The vagus nerve (the tenth cranial nerve) provides sensation to the airway below the epiglottis. The superior laryngeal branch of the vagus divides into an external (motor) nerve and an internal (sensory) laryngeal nerve that provide sensory supply to the larynx between the epiglottis and the vocal cords. Another branch of the vagus, the recurrent laryngeal nerve, innervates the larynx below the vocal cords and the trachea.
The muscles of the larynx are innervated by the recurrent laryngeal nerve, with the exception of the cricothyroid muscle, which is innervated by the external (motor) laryngeal nerve, a branch of the superior laryngeal nerve. The posterior cricoarytenoid muscles abduct the vocal cords, whereas the lateral cricoarytenoid muscles are the principal adductors.
Phonation involves complex simultaneous actions by several laryngeal muscles. Damage to the motor nerves innervating the larynx leads to a spectrum of speech disorders (Table 19-1). Unilateral denervation of a cricothyroid muscle causes very subtle clinical findings. Bilateral palsy of the superior laryngeal nerve may result in hoarseness or easy tiring of the voice, but airway control is not jeopardized.
| Nerve | Effect of Nerve Injury |
|---|---|
| Superior laryngeal nerve | |
| Unilateral | Minimal effects |
| Bilateral | Hoarseness, tiring of voice |
| Recurrent laryngeal nerve | |
| Unilateral | Hoarseness |
| Bilateral | |
| Acute | Stridor, respiratory distress |
| Chronic | Aphonia |
| Vagus nerve | |
| Unilateral | Hoarseness |
| Bilateral | Aphonia |
Unilateral paralysis of a recurrent laryngeal nerve results in paralysis of the ipsilateral vocal cord, causing deterioration in voice quality. Assuming intact superior laryngeal nerves, acute bilateral recurrent laryngeal nerve palsy can result in stridor and respiratory distress because of the remaining unopposed tension of the cricothyroid muscles. Airway problems are less frequent in chronic bilateral recurrent laryngeal nerve loss because of the development of various compensatory mechanisms (eg, atrophy of the laryngeal musculature).
Bilateral injury to the vagus nerve affects both the superior and the recurrent laryngeal nerves. Thus, bilateral vagal denervation produces flaccid, midpositioned vocal cords similar to those seen after administration of succinylcholine. Although phonation is severely impaired in these patients, airway control is rarely a problem.
The blood supply of the larynx is derived from branches of the thyroid arteries. The cricothyroid artery arises from the superior thyroid artery itself, the first branch given off from the external carotid artery, and crosses the upper cricothyroid membrane (CTM), which extends from the cricoid cartilage to the thyroid cartilage. The superior thyroid artery is found along the lateral edge of the CTM.
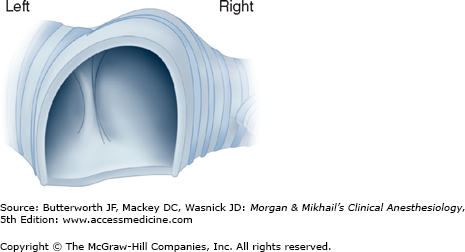
The trachea begins beneath the cricoid cartilage and extends to the carina, the point at which the right and left main-stem bronchi divide (Figure 19-4). Anteriorly, the trachea consists of cartilaginous rings; posteriorly, the trachea is membranous.
Routine Airway Management
Airway Assessment
Airway assessment is the first step in successful airway management. Several anatomical and functional maneuvers can be performed to estimate the difficulty of endotracheal intubation; however, it is important to note that successful ventilation (with or without intubation) must be achieved by the anesthetist if mortality and morbidity are to be avoided. Assessments include:
- Mouth opening: an incisor distance of 3 cm or greater is desirable in an adult.
- Upper lip bite test: the lower teeth are brought in front of the upper teeth. The degree to which this can be done estimates the range of motion of the temperomandibular joints.
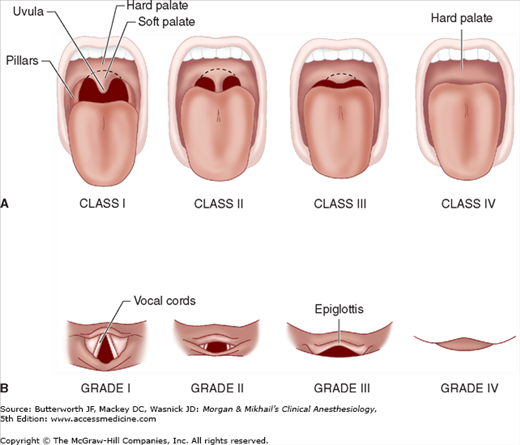
- Mallampati classification: a frequently performed test that examines the size of the tongue in relation to the oral cavity. The greater the tongue obstructs the view of the pharyngeal structures, the more difficult intubation may be (Figure 19-5).
- Class I: the entire palatal arch, including the bilateral faucial pillars, are visible down to their bases.
- Class II: the upper part of the faucial pillars and most of the uvula are visible.
- Class III: only the soft and hard palates are visible.
- Class IV: only the hard palate is visible.
- Class I: the entire palatal arch, including the bilateral faucial pillars, are visible down to their bases.
- Thyromental distance: the distance between the mentum and the superior thyroid notch. A distance greater than 3 fingerbreadths is desirable.
- Neck circumference: a neck circumference of greater than 27 in is suggestive of difficulties in visualization of the glottic opening.
Figure 19-5
A: Mallampati classification of oral opening. B: Grading of the laryngeal view. A difficult orotracheal intubation (grade III or IV) may be predicted by the inability to visualize certain pharyngeal structures (class III or IV) during the preoperative examination of a seated patient. (Reproduced, with permission, from Mallampati SR: Clinical signs to predict difficult tracheal intubation [hypothesis]. Can Anaesth Soc J 1983;30:316.)
Although the presence of these findings may not be particularly sensitive for detecting a difficult intubation, the absence of these findings is predictive for relative ease of intubation.
Increasingly, patients present with morbid obesity and body mass indices of 30 kg/m2 or greater. Although some morbidly obese patients have relatively normal head and neck anatomy, others have much redundant pharyngeal tissue and increased neck circumference. Not only may these patients prove to be difficult to intubate, but routine ventilation with bag and mask also may be problematic.
Equipment
Preparation is mandatory for all airway management scenarios. The following equipment is routinely needed in airway management situations:
- An oxygen source
- BMV capability
- Laryngoscopes (direct and video)
- Several endotracheal tubes of different sizes
- Other (not endotracheal tube) airway devices (eg, oral, nasal airways)
- Suction
- Oximetry and CO2 detection
- Stethoscope
- Tape
- Blood pressure and electrocardiography (ECG) monitors
- Intravenous access
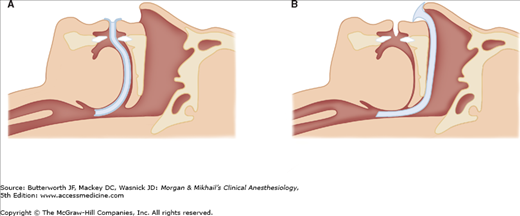
Loss of upper airway muscle tone (eg, weakness of the genioglossus muscle) in anesthetized patients allows the tongue and epiglottis to fall back against the posterior wall of the pharynx. Repositioning the head or a jaw thrust is the preferred technique for opening the airway. To maintain the opening, an artificial airway can be inserted through the mouth or nose to maintain an air passage between the tongue and the posterior pharyngeal wall (Figure 19-6). Awake or lightly anesthetized patients with intact laryngeal reflexes may cough or even develop laryngospasm during airway insertion. Placement of an oral airway is sometimes facilitated by suppressing airway reflexes, and, in addition, sometimes by depressing the tongue with a tongue blade. Adult oral airways typically come in small (80 mm [Guedel No. 3]), medium (90 mm [Guedel No. 4]), and large (100 mm [Guedel No. 5]) sizes.
Figure 19-6
A: The oropharyngeal airway in place. The airway follows the curvature of the tongue, pulling it and the epiglottis away from the posterior pharyngeal wall and providing a channel for air passage. B: The nasopharyngeal airway in place. The airway passes through the nose and extends to just above the epiglottis. (Modified and reproduced, with permission, from Face masks and airways. In: Understanding Anesthesia Equipment, 4th ed. Dorsch JA, Dorsch SE, eds. Williams & Wilkins, 1999.)
The length of a nasal airway can be estimated as the distance from the nares to the meatus of the ear and should be approximately 2-4 cm longer than oral airways. Because of the risk of epistaxis, nasal airways are less desirable in anticoagulated or thrombocytopenic patients. Also, nasal airways (and nasogastric tubes) should be used with caution in patients with basilar skull fractures, where there has been a case report of a nasogastric tube entering the cranial vault. All tubes inserted through the nose (eg, nasal airways, nasogastric catheters, nasotracheal tubes) should be lubricated before being advanced along the floor of the nasal passage.
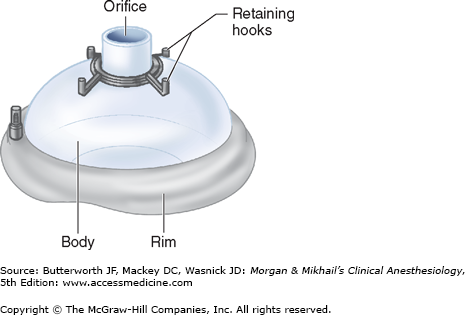
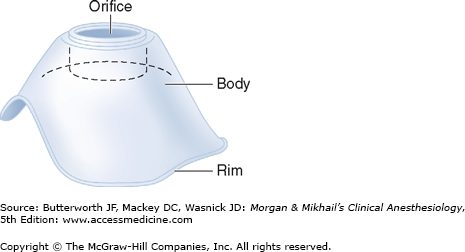
The use of a face mask can facilitate the delivery of oxygen or an anesthetic gas from a breathing system to a patient by creating an airtight seal with the patient’s face (Figure 19-7). The rim of the mask is contoured and conforms to a variety of facial features. The mask’s 22-mm orifice attaches to the breathing circuit of the anesthesia machine through a right-angle connector. Several mask designs are available. Transparent masks allow observation of exhaled humidified gas and immediate recognition of vomitus. Retaining hooks surrounding the orifice can be attached to a head strap so that the mask does not have to be continually held in place. Some pediatric masks are specially designed to minimize apparatus dead space (Figure 19-8).
Effective mask ventilation requires both a gas-tight mask fit and a patent airway.  Improper face mask technique can result in continued deflation of the anesthesia reservoir bag when the adjustable pressure-limiting valve is closed, usually indicating a substantial leak around the mask. In contrast, the generation of high breathing circuit pressures with minimal chest movement and breath sounds implies an obstructed airway or obstructed tubing.
Improper face mask technique can result in continued deflation of the anesthesia reservoir bag when the adjustable pressure-limiting valve is closed, usually indicating a substantial leak around the mask. In contrast, the generation of high breathing circuit pressures with minimal chest movement and breath sounds implies an obstructed airway or obstructed tubing.
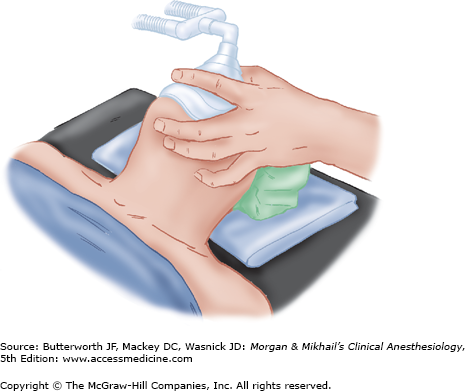
If the mask is held with the left hand, the right hand can be used to generate positive-pressure ventilation by squeezing the breathing bag. The mask is held against the face by downward pressure on the mask body exerted by the left thumb and index finger (Figure 19-9). The middle and ring finger grasp the mandible to facilitate extension of the atlantooccipital joint. This is a maneuver that is easier to teach than to describe. Finger pressure should be placed on the bony mandible and not on the soft tissues supporting the base of the tongue, which may obstruct the airway. The little finger is placed under the angle of the jaw and used to thrust the jaw anteriorly, the most important maneuver to allow ventilation to the patient.
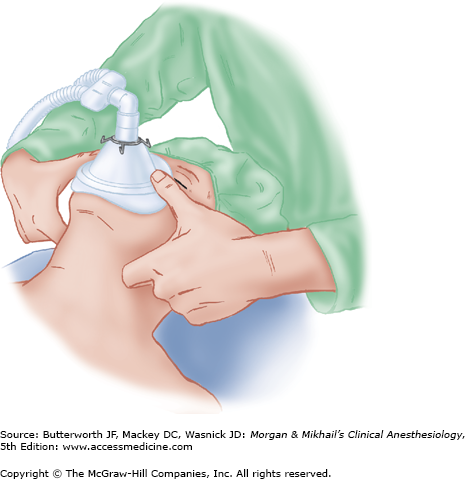
In difficult situations, two hands may be needed to provide adequate jaw thrust and to create a mask seal. Therefore, an assistant may be needed to squeeze the bag, or the machine’s ventilator can be used. In such cases, the thumbs hold the mask down, and the fingertips or knuckles displace the jaw forward (Figure 19-10). Obstruction during expiration may be due to excessive downward pressure from the mask or from a ball-valve effect of the jaw thrust. The former can be relieved by decreasing the pressure on the mask, and the latter by releasing the jaw thrust during this phase of the respiratory cycle. It is often difficult to form an adequate mask fit with the cheeks of edentulous patients. Positive-pressure ventilation using a mask should normally be limited to 20 cm of H2O to avoid stomach inflation.
Most patients’ airways can be maintained with a face mask and an oral or nasal airway. Mask ventilation for long periods may result in pressure injury to branches of the trigeminal or facial nerves. Because of the absence of positive airway pressures during spontaneous ventilation, only minimal downward force on the face mask is required to create an adequate seal. If the face mask and mask straps are used for extended periods, the position should be regularly changed to prevent injury. Care should be used to avoid mask or finger contact with the eye, and the eyes should be taped shut to minimize the risk of corneal abrasions.
Positioning
When manipulating the airway, correct patient positioning is required. Relative alignment of the oral and pharyngeal axes is achieved by having the patient in the “sniffing” position. When cervical spine pathology is suspected, the head must be kept in a neutral position during all airway manipulations. In-line stabilization of the neck must be maintained during airway management in these patients, unless appropriate films have been reviewed and cleared by a radiologist or neurological or spine surgeon. Patients with morbid obesity should be positioned on a 30° upward ramp, as the functional residual capacity (FRC) of obese patients deteriorates in the supine position, leading to more rapid deoxygenation should ventilation be impaired.
Preoxygenation
When possible, preoxygenation with face mask oxygen should precede all airway management interventions. Oxygen is delivered by mask for several minutes prior to anesthetic induction. In this way, the functional residual capacity, the patient’s oxygen reserve, is purged of nitrogen. Up to 90% of the normal FRC of 2 L following preoxygenation is filled with O2. Considering the normal oxygen demand of 200-250 mL/min, the preoxygenated patient may have a 5-8 min oxygen reserve. Increasing the duration of apnea without desaturation improves safety, if ventilation following anesthetic induction is delayed. Conditions that increase oxygen demand (eg, sepsis, pregnancy) and decrease FRC (eg, morbid obesity, pregnancy) reduce the apneic period before desaturation ensues.
Bag and Mask Ventilation
Bag and mask ventilation (BMV) is the first step in airway management in most situations, with the exception of patients undergoing rapid sequence intubation. Rapid sequence inductions avoid BMV to avoid stomach inflation and to reduce the potential for the aspiration of gastric contents in nonfasted patients and those with delayed gastric emptying. In emergency situations, BMV precedes attempts at intubation in an effort to oxygenate the patient, with the understanding that there is an implicit risk of aspiration.
As noted above, the anesthetist’s left hand supports the mask on the patient’s face. The face is lifted into the mask with the third, fourth, and fifth fingers of the anesthesia provider’s left hand. The fingers are placed on the mandible, and the jaw is thrust forward, lifting the base of the tongue away from the posterior pharynx opening the airway. The thumb and index finger sit on top of the mask. If the airway is patent, squeezing the bag will result in the rise of the chest. If ventilation is ineffective (no sign of chest rising, no end-tidal CO2 detected, no mist in the clear mask), oral or nasal airways can be placed to relieve airway obstruction secondary to redundant pharyngeal tissues. Difficult mask ventilation is often found in patients with morbid obesity, beards, and craniofacial deformities.
Supraglottic Airway Devices
Supraglottic airway devices (SADs) are used with both spontaneously and ventilated patients during anesthesia. They have also been employed as conduits to aid endotracheal intubation when both BMV and endotracheal intubation have failed. All SADs consist of a tube that is connected to a respiratory circuit or breathing bag, which is attached to a hypopharyngeal device that seals and directs airflow to the glottis, trachea, and lungs. Additionally, these airway devices occlude the esophagus with varying degrees of effectiveness, reducing gas distension of the stomach. Different sealing devices to prevent airflow from exiting through the mouth are also available. Some are equipped with a port to suction gastric contents. None offer the protection from aspiration pneumonitis offered by a properly sited, cuffed endotracheal tube.
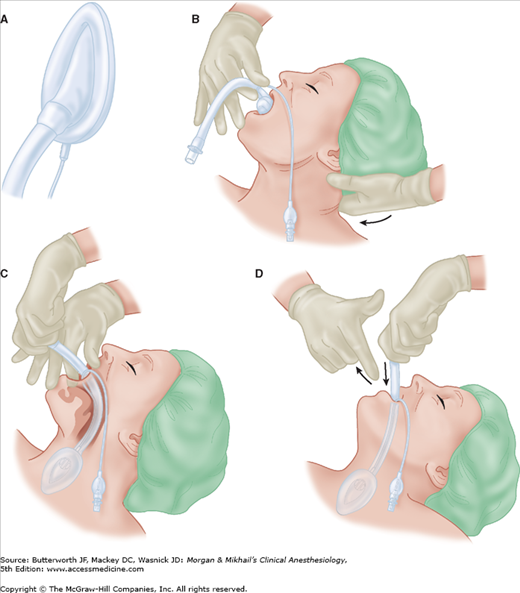
A laryngeal mask airway (LMA) consists of a wide-bore tube whose proximal end connects to a breathing circuit with a standard 15-mm connector, and whose distal end is attached to an elliptical cuff that can be inflated through a pilot tube. The deflated cuff is lubricated and inserted blindly into the hypopharynx so that, once inflated, the cuff forms a low-pressure seal around the entrance to the larynx. This requires anesthetic depth and muscle relaxation slightly greater than that required for the insertion of an oral airway. Although insertion is relatively simple (Figure 19-11), attention to detail will improve the success rate (Table 19-2). An ideally positioned cuff is bordered by the base of the tongue superiorly, the pyriform sinuses laterally, and the upper esophageal sphincter inferiorly. If the esophagus lies within the rim of the cuff, gastric distention and regurgitation become possible. Anatomic variations prevent adequate functioning in some patients. However, if an LMA is not functioning properly after attempts to improve the “fit” of the LMA have failed, most practitioners will try another LMA one size larger or smaller. The shaft can be secured with tape to the skin of the face.  The LMA partially protects the larynx from pharyngeal secretions (but not gastric regurgitation), and it should remain in place until the patient has regained airway reflexes. This is usually signaled by coughing and mouth opening on command. The LMA is available in many sizes (Table 19-3).
The LMA partially protects the larynx from pharyngeal secretions (but not gastric regurgitation), and it should remain in place until the patient has regained airway reflexes. This is usually signaled by coughing and mouth opening on command. The LMA is available in many sizes (Table 19-3).
Figure 19-11
A: The laryngeal mask ready for insertion. The cuff should be deflated tightly with the rim facing away from the mask aperture. There should be no folds near the tip. B: Initial insertion of the laryngeal mask. Under direct vision, the mask tip is pressed upward against the hard palate. The middle finger may be used to push the lower jaw downward. The mask is pressed forward as it is advanced into the pharynx to ensure that the tip remains flattened and avoids the tongue. The jaw should not be held open once the mask is inside the mouth. The nonintubating hand can be used to stabilize the occiput. C: By withdrawing the other fingers and with a slight pronation of the forearm, it is usually possible to push the mask fully into position in one fluid movement. Note that the neck is kept flexed and the head extended. D: The laryngeal mask is grasped with the other hand and the index finger withdrawn. The hand holding the tube presses gently downward until resistance is encountered. (Reproduced, with permission, from LMA North America.)
|
| Mask Size | Patient Size | Weight (kg) | Cuff Volume (mL) |
|---|---|---|---|
| 1 | Infant | <6.5 | 2-4 |
| 2 | Child | 6.5-20 | Up to 10 |
| 2½ | Child | 20-30 | Up to 15 |
| 3 | Small adult | >30 | Up to 20 |
| 4 | Normal adult | <70 | Up to 30 |
| 5 | Larger adult | >70 | Up to 30 |
The LMA provides an alternative to ventilation through a face mask or TT (Table 19-4). Relative contraindications for the LMA include patients with pharyngeal pathology (eg, abscess), pharyngeal obstruction, full stomachs (eg, pregnancy, hiatal hernia), or low pulmonary compliance (eg, restrictive airways disease) requiring peak inspiratory pressures greater than 30 cm H2O. Traditionally, the LMA has been avoided in patients with bronchospasm or high airway resistance, but new evidence suggests that because it is not placed in the trachea, use of an LMA is associated with less bronchospasm than a TT. Although it is clearly not a substitute for tracheal intubation, the LMA has proven particularly helpful as a life-saving temporizing measure in patients with difficult airways (those who cannot be ventilated or intubated) because of its ease of insertion and relatively high success rate (95% to 99%). It has been used as a conduit for an intubating stylet (eg, gum-elastic bougie), ventilating jet stylet, flexible FOB, or small-diameter (6.0-mm) TT. Several LMAs are available that have been modified to facilitate placement of a larger TT, with or without the use of a FOB. Insertion can be performed under topical anesthesia and bilateral superior laryngeal nerve blocks, if the airway must be secured while the patient is awake.
| Advantages | Disadvantages | |
|---|---|---|
| Compared with face mask |
|
|
| Compared with tracheal intubation |
|
|
Variations in LMA design include:
- The ProSeal LMA, which permits passage of a gastric tube to decompress the stomach
- The I-Gel, which uses a gel occluder rather than inflatable cuff
- The Fastrach intubation LMA, which is designed to facilitate endotracheal intubation through the LMA device
- The LMA CTrach, which incorporates a camera to facilitate passage of an endotracheal tube
Sore throat is a common side effect following SAD use. Injuries to the lingual, hypoglossal, and recurrent laryngeal nerve have been reported. Correct device sizing, avoidance of cuff hyperinflation, and gentle movement of the jaw during placement may reduce the likelihood of such injuries.