Abdominal Compartment Syndrome
Patrick González Jr.
Lawrence Lottenberg
Joseph A. Layon
CASE SUMMARY
A 19-year-old male adolescent was standing in the back of a pickup truck that collided with a tree. The patient arrived in the trauma resuscitation bay with a surgical airway, hypotension, chest wall crepitus, and fixed, dilated pupils after more than 20 minutes in transport. Bilateral chest tubes were inserted to treat hemopneumothoraces, and a Foley catheter was inserted and was noted to be draining frank blood. Radiologic studies ruled out pelvic fractures. Focused abdominal sonography for trauma revealed the presence of intra-abdominal fluid. Primary resuscitation was unsuccessful using crystalloids and blood products, with refractory hypotension that was reversed with continuous volume infusion. The patient was transported to the operating room for emergent exploration of his abdomen.
Perioperatively, the patient received a massive resuscitation including crystalloids, blood products, and activated recombinant factor VII. A damage control celiotomy revealed a large hemoperitoneum, which was evacuated. A lacerated spleen was removed, and a large, nonexpanding, left-sided retroperitoneal hematoma was identified. The patient was coagulopathic, acidotic, and hypothermic. The distended bowel prohibited definitive closure of the abdominal wall; the abdomen was left open and packed with surgical lap pads. During temporary abdominal closure, using a sterile adhesive drape and intra-abdominal drain catheters connected to continuous suction, the patient developed sudden cardiac arrest. This event responded to the Advanced Cardiac Life Support protocol. Immediate reexploration was performed. The left retroperitoneal space was noted to be enlarging and was now leaking frank blood. A left nephrectomy was performed. No further surgical bleeding was identified.
The abdominal cavity was dressed as noted earlier. A postoperative computerized tomography scan of the head showed severe closed head injury with uncal herniation. The patient was taken to the intensive care unit, and secondary resuscitation for correction of hypothermia, acidosis, and coagulopathy was continued. After a rocky hemodynamic course, the family requested withdrawal of life support, and the patient expired.
This clinical scenario is an example of abdominal compartment syndrome (ACS) associated with organ dysfunction.
What Is the Abdominal Compartment Syndrome?
ACS occurs from increased intra-abdominal pressure. Richardson described elevated end-inspiratory pressures and hypoperfusion secondary to a low cardiac output (CO) associated with ACS.1 Impaired venous return and high peak inspiratory pressure with hypercarbia were present, causing hypoperfusion and severe pulmonary dysfunction. Early surgical decompression is mandatory, and a better outcome is associated with early detection. Release of the restrictive abdominal pressure will result in the correction of organ dysfunction. Oliguria is an early sign of ACS, but the most reliable clinical indicator is progressive failure of ventilation. A typical case of ACS has a peak inspiratory pressure in the range of 85 cm H2O, with a rise in PaCo2. A decompressive celiotomy is indicated in the presence of abdominal distention, hypercarbia, and high peak inspiratory pressures. This procedure may be performed either at bedside or in the operating room.
The surgical technique performed for damage control is a continuum that includes primary resuscitation, damage control celiotomy, secondary resuscitation, and delayed reconstruction.2 Patients in extremis usually do not tolerate reconstruction. In summary, ACS is a surgical emergency that requires the damage control technique to prevent organ dysfunction. If ACS is recognized late or goes unrecognized, it can lead to multiple organ failure and death.
What Makes Up the Intra-Abdominal Compartment?
The boundaries of the intra-abdominal compartment consist of the diaphragm, pelvic floor, retroperitoneum, chest, and abdominal wall. Abdominal compartment compliance decreases with an increase in intra-abdominal pressure, with resultant direct impact upon the contents of the abdominal cavity. The contents of the abdominal compartment consist of the gastrointestinal tract, solid organs (liver, spleen, etc.), nerves, arteries, and veins. The diaphragm has direct impact on the lungs and heart. An increase in the intra-abdominal pressure is associated with increased peak inspiratory pressures, as well as hypercarbia.
The retroperitoneum harbors the kidneys, ureters, and the major abdominal vessels. This area is at risk for major hemorrhage that can result in ACS. Retroperitoneal hemorrhage rarely causes compression of the ureters. Rather, a prerenal state occurs with decreased CO secondary to decreased venous return. The pelvic organs, such as the urinary bladder and the pelvis itself, may also be major sources of blood loss. Monitoring of abdominal compartment pressure is critical. In severe cases of pancreatitis, this organ may be an etiologic factor for ACS.
The abdominal wall provides the ventral covering of the abdominal cavity and allows for limited expansion of the intra-abdominal contents. Hypoperfusion of the abdominal wall due to intra-abdominal hypertension is associated with an increase in wound complications. Ascites may also cause intra-abdominal hypertension when massive amounts of fluid accumulate in the abdomen. The gastrointestinal tract consists of the stomach, the small bowel, and colon. Significant amounts of fluid and/or air can accumulate in these structures, causing intra-abdominal hypertension. Bowel perforation with peritoneal contamination is associated with diffuse peritonitis, another etiologic factor of ACS.
How Is “Normal” Intra-Abdominal Pressure Measured?
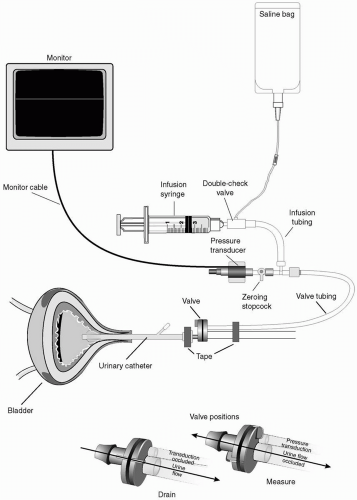
Intra-abdominal pressure is that pressure concealed within the abdominal cavity, which varies with respiration. A normal intra-abdominal pressure is approximately 5 mm Hg, but may be higher with obesity. Intra-abdominal pressure should be expressed in mmHg and measured at end-expiration with the patient in the supine position, without abdominal contractions. The pressure transducer should be zero-referenced to the level of the midaxillary line. Direct intra-abdominal measurement is obtained with direct needle puncture and transduction of the pressure within the abdominal cavity. Indirect intra-abdominal pressure measurement is accomplished through transduction of the pressure within the bladder. Bladder pressure may be measured by injecting 50 to 100 mL of sterile saline into the aspiration port of the Foley drainage tube. The catheter is then clamped distal to the aspiration port, and a 16-gauge needle is used to connect a pressure transducer to the aspiration port of the catheter. The top of the symphysis pubis (or the midaxillary line) is used as the zero point on the supine patient.
For continuous, indirect intra-abdominal pressure measurement, a balloon-tipped catheter in the stomach or a continuous bladder irrigation method is recommended (see Fig. 40.1). The ACS is not seen, as long as the intra-abdominal pressure is normal. The group at Denver Health Medical Center has proposed a grading system based on urinary bladder pressure measurements3 (see Table 40.1). A pressure of 25 mmHg or higher is associated with organ dysfunction and considered clinical intra-abdominal hypertension. At or above this pressure, surgical decompression is justifiable.
How Does the Abdominal Compartment Syndrome Develop?
Many clinical scenarios may be associated with ACS. Any pathologic process that causes an increase in the intra-abdominal pressure can lead to ACS. Accumulation of fluid in the abdominal cavity may be associated with a marked decrease in the compliance of the abdominal wall, with associated intra-abdominal hypertension. Excessive air in the gastrointestinal tract can increase pressure, but rarely causes ACS unless associated with a primary pathologic process that requires massive fluid resuscitation. Diffuse peritonitis, major hemorrhage, and massive ascites are also associated with ACS.
ACS may be prevented through the early identification of risk factors and diagnosis. A high index of suspicion is necessary for prevention. Liberal use of surgical decompression is strongly recommended when critical intra-abdominal pressure is reached,4 or when the clinical scenario is present. High peak inspiratory pressures (>85 cm H2O), hypercarbia, and oliguria are all clinical signs of ACS.5 The change in pressure is a function of the rate of fluid accumulation and the compliance of the abdominal cavity. The pressure-volume curve for the abdominal cavity is nonlinear.6
How Does the Abdominal Compartment Syndrome Present?
A variety of conditions, both surgical and nonsurgical, increase the risk of developing the ACS. The common
denominator in each of these conditions appears to be the need for large volume resuscitation. For example, patients presenting with acute major abdominal hemorrhage are at very high risk for ACS. Other conditions include “nonmajor” intraperitoneal hemorrhage, intra-abdominal catastrophes, abdominal trauma, hemorrhagic pancreatitis, severe ascites, hepatic transplantation, and ovarian tumors. In the presence of one of the high-risk conditions, the risk of ACS may be heightened by hypothermia, acidosis, and/or coagulopathy due to the volume replacement that may be required for resuscitation. Other factors to be considered include:7,8,9,10,11,12,13,14,15,16,17
denominator in each of these conditions appears to be the need for large volume resuscitation. For example, patients presenting with acute major abdominal hemorrhage are at very high risk for ACS. Other conditions include “nonmajor” intraperitoneal hemorrhage, intra-abdominal catastrophes, abdominal trauma, hemorrhagic pancreatitis, severe ascites, hepatic transplantation, and ovarian tumors. In the presence of one of the high-risk conditions, the risk of ACS may be heightened by hypothermia, acidosis, and/or coagulopathy due to the volume replacement that may be required for resuscitation. Other factors to be considered include:7,8,9,10,11,12,13,14,15,16,17
Retroperitoneal bleeding
Use of pneumatic antishock garments
Abdominal wall fascial closure under tension in a high-risk patient
Persistent surgical intra-abdominal bleeding
Damage control celiotomy using laparotomy pad packing for bleeding control
Patients without abdominal injury that require massive fluid resuscitation for conditions like major burns or severe acute pancreatitis
TABLE 40.1 Grading of the Abdominal Compartment Syndrome | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
ACS may be subdivided into primary, secondary, and tertiary variants:
PRIMARY: Primary ACS is associated with an injury or disease in the abdominopelvic region that frequently requires early surgical or angioradiologic intervention, or a condition that develops after abdominal surgery. Examples are damage control surgery, secondary peritonitis, bleeding pelvic fractures, other causes of massive retroperitoneal hematoma, liver transplant, and nonoperative management of solid organ injury.
SECONDARY: Secondary ACS is associated with conditions that do not originate from the abdomen, yet develop clinical findings of ACS. Examples are conditions such as sepsis and capillary leak, major burns, and other conditions requiring massive fluid resuscitation.
TERTIARY: Tertiary (or recurrent) ACS occurs when ACS develops after prophylactic or therapeutic surgical or medical treatment of primary or secondary ACS, when there is persistence of ACS after decompressive laparotomy, or development of a new ACS episode after definitive abdominal wall closure. The clinical manifestations of ACS are the result of multiple organ dysfunction, affecting the respiratory, renal, cardiovascular, and neurologic systems.16
Respiratory manifestations are related directly to the effect of intra-abdominal hypertension, which elevate the hemidiaphragms, with an associated decrease in intrathoracic volume and compliance. Elevated peak airway pressures and pulmonary vascular resistance will most often be present. In ACS, ventilatory support becomes difficult, and relatively sophisticated strategies of mechanical ventilation are often necessary to stabilize and improve the respiratory mechanics. Respiratory deterioration, if it occurs, may lead to development of severe hypercarbia, worsening acidosis, and hypoxemia.
The changes in cardiovascular parameters are due to increased intrathoracic pressure from intra-abdominal hypertension.1,18,19,20,21 Cardiovascular changes include an increase in central venous and pulmonary artery wedge pressures, and systemic vascular resistance. CO decreases progressively with increases in intra-abdominal pressure, and is dependent on the intravascular volume status. Kashtan et al. showed that changes in CO were demonstrable in the setting of ACS. Hypovolemic animals developed a 53% decline in CO, compared with a 17% decline in the euvolemic group and a 50% increase in the hypervolemic group.19 Patients with ACS may have an increase in CO with intravascular volume replacement, but fluid alone cannot correct the renal dysfunction and decrease in splanchnic blood flow associated with ACS.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree