CHAPTER 26. Infectious and Communicable Diseases
Russell D. MacDonald
Transport personnel routinely encounter patients with infectious disease or suspected infectious disease. This encounter may be in the form of a sudden illness in the community setting or the transfer of a critically ill patient from one institution to a higher level of care. These emergencies put transport personnel at risk because the type, extent, and severity of these illnesses are not yet known. The Occupational Safety and Health Administration (OSHA) identifies more than 1.2 million community-based first-response personnel, including law enforcement, fire, and emergency medical service personnel, at risk for infectious exposure. 7 This large number highlights the need to protect these personnel against such exposures.
In the past, infectious and communicable disease preparation may not have been a priority. However, the 2003 severe acute respiratory syndrome (SARS) outbreaks made this preparation a priority. Medical personnel who cared for patients at the onset of the SARS outbreaks in Toronto8 and Taipei4 were exposed to or contracted SARS in significant numbers, and one paramedic died of SARS. More importantly, the loss of personnel from work because of exposure, illness, and quarantine impacted the ability to maintain staffing during the outbreak and highlighted the need to adequately prepare and protect the workforce from potential exposure. 3,5,9
This chapter addresses communicable and infectious disease in a manner relevant to transport agencies and their personnel. The chapter is divided in two parts. The first is transport personnel and patient centered and describes the basics of communicable disease transmission and prevention, general approach to the patient with a suspected infectious or communicable disease, and specific disease conditions outlined by presenting symptom. The second is provider oriented and outlines occupational health and safety issues necessary to protect responding transport personnel.
TRANSPORT PERSONNEL AND THE PATIENT
Communicable Disease Transmission and Prevention
The Occupational Safety and Health Administration defines occupational exposure as “a reasonably anticipated skin, eye, mucous membrane, or parenteral contact with blood or other potentially infectious material that may result from the performance of the employee’s duties.”7 Infection control practices are designed to prevent exposure to blood or potentially infectious material, including cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, amniotic fluid, peritoneal fluid, and any other body fluid, secretion, or tissue.
Universal precautions is the term formerly used to describe aspects of the methods used to prevent exposure, but this term is no longer used by healthcare workers. The more favored terms are routine practices and additional precautions. These terms indicate the same basic minimal level of precaution taken for all patients.
Infection is defined by the Association for Professionals in Infection Control and Epidemiology1 as an invasion and multiplication of microorganisms in or on body tissue that causes cellular damage through the production of toxins, multiplication, or competition with host metabolism. Infectious agents capable of causing disease include bacteria, viruses, fungi and molds, parasites, and prions. These five types of microorganisms can be differentiated by their appearance on microscopic examination, reproductive cycle, chemical structure, growth requirements, and other detailed criteria. Although bacteria and viruses are the most common causes of illness in the developed world, parasites are more prevalent in other settings.
As shown in Figure 26-1, numerous factors are directly related to the ability of a microorganism to cause an infection. The dose is the amount of viable organism received during an exposure. Infection occurs with the presence of a large enough number to overwhelm the body’s own defenses. Virulence refers to the ability of a microorganism to cause infection, and pathogenicity refers to the severity of infection. Additional factors determine the likelihood of transmission. Incubation and communicability periods are the intervals between the organism entering the body and the appearance of symptoms and the time during which the infected individual can spread the disease to others, respectively. The host status and resistance refer to the host’s ability to fight infection, which can be influenced by immune function and immunization status, nutritional state, and presence of comorbid illness.
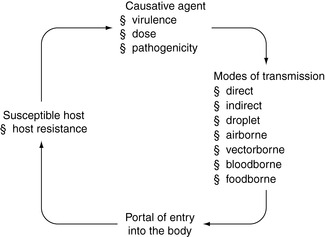 |
| FIGURE 26-1 The infectious disease process. |
An infectious disease results from the invasion of a host by disease-producing organisms, such as bacteria, viruses, fungi, or parasites. A communicable (or contagious) disease is one that can be transmitted from one person to another. Not all infectious diseases are communicable. For example, malaria is a serious infectious disease transmitted to the human bloodstream by a mosquito bite, but malaria is infectious, not communicable. On the other hand, chickenpox is an infectious disease that is also highly communicable because it can be easily transmitted from one person to another.
The mode of transmission is the mechanism by which an agent is transferred to the host. Modes of transmission include contact transmission (direct, indirect, droplet), airborne, vector-borne, or common vehicle (food, equipment). Contact transmission is the most common mode of transmission in the transport medicine setting and can be effectively prevented with routine practices. Table 26-1 contains a summary of disease transmission.
| Type and Definition of Transmission | Examples of Diseases Transmitted |
|---|---|
Contact transmission:Direct contact occurs between the infected colonized individual and a susceptible host. Indirect contact occurs with passive transfer of infections agents such as those left on a surface. | HIV Methicillin-resistant S. aureus (MRSA) Norwalk virus C. difficile |
| Droplet transmission: Large droplets generated from the respiratory tract of a patient when the patient sneezes or during invasive procedures such as suctioning. | Meningitis Influenza Rhinovirus Respiratory syncytial virus and SARS |
| Airborne transmission: Spread of disease via the airborne route. | Measles Varicella Tuberculosis |
| Vector-borne transmission: Disease is spread by means of an insect or animal (vector). | Rabies West Nile virus |
| Common vehicle transmission: Spread of an infectious agent by a single contaminated source to multiple hosts. | Water sources (E. coli) Contaminated food (Salmonella) Contaminated medical equipment |
General Approach and Patient Assessment
The risk of communicable disease is not as apparent as other physical risks, such as road traffic, power lines, firearms, or chemical agents. Transport personnel must use the same level of suspicion and precaution when approaching a patient before the risk of communicable disease is known. The use of routine practices, as a minimum, is necessary for every patient encounter to mitigate this risk.
The risk assessment begins with information from a dispatch or communication center, before patient contact is made. Call-taking procedures must include basic screening information to identify potential communicable disease threats and provide this information to all responding personnel. The screening information can identify patients with symptoms of fever, chills, cough, shortness of breath, or diarrhea. The call-taking can also identify whether the patient location, such nursing home, group home, or other institutional setting, poses a potential risk to the responding personnel. This information helps responding personnel determine what precautions are necessary before they make contact.
When patient contact is made, personnel can identify the patient at risk for a communicable disease. A rapid history and physical examination can raise suspicion for a communicable disease. The following screening questions help assess whether the patient has a communicable disease:
▪ Do you have a new or worsening cough or shortness of breath?
▪ Do you have a fever?
▪ Have you had shakes or chills in the past 24 hours?
▪ Have you had an abnormal temperature (>38 °C)?
▪ Have you taken medication for fever?
A screening physical examination also identifies obvious signs of a communicable disease. These signs may include any new symptom of infection (fever, headache, muscle ache, cough, sputum, weight loss, and exposure history), rash, diarrhea, skin lesions, or draining wounds.
All personnel must take appropriate precautions when a patient has any signs or symptoms suspected to be the result of an infectious or communicable disease. All transport medicine agencies must provide appropriate training that enables personnel to identify at-risk patients and appropriate use of personal protective equipment (PPE). The levels of PPE needed based on perceived disease threat are addressed in detail in subsequent sections of this chapter.
Specific Disease Conditions by Presenting or Chief Symptom
Respiratory Infections
Respiratory infections may be suspected with symptoms that classically include any combination of cough, sneeze, shortness of breath, fever, chills or shakes. Infections above the epiglottis are classified as upper respiratory tract infections, and those below the epiglottis are classified as lower respiratory tract infections. Upper respiratory infections may be suspected when patients present with “cold” symptoms such as rhinorrhea, sneezing, lacrimation, or coryza. More localized and possibly more serious upper respiratory infection may present with symptoms such as throat pain, fever, odynophagia, dysphagia, drooling, stridor, or muffled voice. Lower respiratory infections typically present with fever, shortness of breath, pleural pain, cough, sputum, or generalized symptoms such as chills, rigors, myalgia, arthralgia, malaise, and headache. More atypical symptoms of respiratory infection may be found in children, the elderly, and patients with immunocompromise. Children with respiratory infection may have gastrointestinal symptoms such as nausea, vomiting, abdominal pain, and diarrhea. The elderly and patients with immunocompromise may not have a fever with respiratory infection.
Respiratory infections are spread when people cough or sneeze and the aerosolized respiratory secretions directly come in contact with the mouth, nose, or eyes of another person. Because microorganisms in droplets can survive outside the body, indirect transmission can also occur when hands, objects, or surfaces become soiled with respiratory discharges. When respiratory infections are suspected in patients, providers should use droplet precautions and apply them to a patient.
Febrile Respiratory Illness
Febrile respiratory illness should be suspected when a patient has any combination of fever, new or worse cough, and shortness of breath. The elderly and patients with immunocompromise may not have a febrile response to a respiratory infection.
Cough
Pneumonia
In addition to cough, shortness of breath, and fever, patients with pneumonia may also have additional symptoms of tachypnea, increased work of breathing, chest or upper abdominal pain, and cough productive of phlegm, sputum, or blood. Generalized systemic symptoms such as myalgia, arthralgia, malaise, and headache may also be present. Gastrointestinal symptoms such as nausea, vomiting, and diarrhea may be associated with pneumonia.
Evidence indicates that the signs and symptoms traditionally associated with pneumonia are actually not predictive of pneumonia, whereas diarrhea, dry cough, and fever are more predictive of pneumonia. In elderly patients, the diagnosis of pneumonia is more difficult because both respiratory and nonrespiratory symptoms are less commonly reported by this patient group.
Infectious agents that typically cause pneumonia include Streptococcus pneumoniae, Mycoplasma pneumoniae, Chlamydia trachomatis, Chlamydia pneumoniae, Pneumocystis carinii, and Haemophilus influenzae. The incubation period from initial contact with the microorganism to development of symptoms is generally not well known for these organisms. For S. pneumoniae, it may be 1 to 3 days; M. pneumoniae may range from 6 to 32 days. P. carinii may appear 1 to 2 months after initial contact for those with immunosuppression. S. pneumoniae can be transmitted up to 48 hours after treatment is initiated. However, M. pneumoniae can be transmissible for up to 20 days, and the organism may remain in the respiratory tract for up to 13 weeks after treatment. For the other organisms, the time period for transmission is unknown.
Pertussis
Pertussis should be included in the differential diagnosis of a patient with chronic cough. Pertussis presents in three stages: first, a catarrhal stage that lasts 1 to 2 weeks; next, a paroxysmal stage that lasts 1 to 6 weeks; and finally, a convalescent stage that lasts 2 to 3 weeks. In the first stage, pertussis is virtually indistinguishable from any other respiratory illness; it is characterized by runny nose, sneezing, low-grade fever, and mild cough. The provider may suspect pertussis in the second, paroxysmal, stage when the patient has bursts of rapid coughs. The cough usually ends with a long high-pitched inspiratory effort described as a whoop, or it may end with vomiting. The third state is the period of recovery in which the cough becomes less paroxysmal. In adolescents, adults, and those who are vaccinated, pertussis is milder and thus may be indistinguishable from other respiratory illnesses, even in the paroxysmal stage.
Pertussis is caused by the Bordetella pertussis bacterium and transmitted via the respiratory route with airborne droplets. Thus, respiratory and contact precautions should be undertaken with known or suspected cases of pertussis. Unfortunately, routine precautions are not always sufficient because pertussis is most infectious during the nonspecific catarrhal period and the first 2 weeks of the paroxysmal phase. The time from infection to the development of symptoms is usually 7 to 10 days.
Complications from pertussis most often occur in young infants. The major complication and most common cause of pertussis-related death is bacterial pneumonia.
With the introduction of routine pertussis vaccination, pertussis rates had declined from about 140 cases per 100,000 population in the 1940s to about 1 per 100,000 population in the 1980s. However, since the 1980s, pertussis rates have been steadily increasing. In 2002 in the United States, a rate of 3 cases per 100,000 population was seen. Most cases were in children under 6 months of age, the age group most at risk of pertussis-related complications.
Influenza
Influenza classically presents with the abrupt onset of fever (usually 38 °C to 40 °C), sore throat, nonproductive cough, myalgia, headache, and chills. Unfortunately, only about half of infected persons have the classic symptoms of influenza infection. From those classic symptoms, studies have attempted to identify the signs and symptoms most predictive of influenza. Unfortunately, these clinical decision rules are no better than clinician judgment alone.
Influenza is caused by a virus with three subtypes: influenza A, B, and C. Influenza A causes more severe disease and is mainly responsible for pandemics. Influenza A has different subtypes determined by surface antigens H (hemagglutinin) and N (neuraminidase). Influenza B causes more mild disease and mainly affects children. Influenza C rarely causes human illness and has not been associated with epidemics.
Influenza transmission occurs primarily through airborne spread when a person coughs or sneezes but may also occur through direct contact of surfaces contaminated with respiratory secretions. Hand washing and shielding of coughs and sneezes help prevent spread. Influenza is transmissible from 1 day before symptom onset to about 5 days after symptoms begin and may last up to 10 days in children. Time from infection to development of symptoms is 1 to 4 days.
Individuals at high risk of influenza complications include young children, people over age 65 years, those with immunosuppression, and those with chronic medical conditions. Complications of influenza include pneumonia, either the more common secondary bacterial pneumonia or rare primary influenza viral pneumonia; Reye’s syndrome in children taking aspirin; myocarditis; encephalitis; and death. Death occurs in about 1 per 1000 cases of influenza, mainly in persons older than age 65 years. Providers should be immunized annually, typically in October.
Four antiviral drugs are available for prevention and treatment of influenza in the United States. Amantadine and rimantadine belong to a class of drugs, adamantanes, which are active against influenza A; oseltamivir and zanamivir belong to the class of neuraminidase inhibitors, which are active against influenza A and B. When used for prevention of influenza, they can be 70% to 90% effective. When used for treatment, antiviral medications can reduce influenza illness duration by 1 day and attenuate the severity of illness. Antiviral agents should be used as an adjunct to vaccination but should not replace vaccination. The Centers for Disease Control (CDC) recommends influenza antiviral medications for individuals who have not as yet been vaccinated at the time of exposure or who have a contraindication to vaccination and are also at high risk of influenza complications. Also, if an influenza outbreak is caused by a variant strain of influenza not controlled with vaccination, chemoprophylaxis should be considered for healthcare providers who care for patients at high risk of influenza complications, regardless of vaccination status. Since the 2005 to 2006 influenza season, a high proportion of influenza A viruses are resistant to the adamantanes. As a result, the CDC has recently recommended against the use of adamantanes for treatment and prophylaxis of influenza. The neuraminidase inhibitors continue to be recommended as a second line of defense against influenza. For prophylaxis, the neuraminidase inhibitors should be taken daily until the exposure no longer exists or until immunity from vaccination develops, which can take about 2 weeks. For treatment, these antiviral medications should be started as soon as influenza symptoms develop, but no later than 48 hours after symptoms start, and treatment should continue for 5 days. In the setting of an influenza outbreak, transport agencies and systems may opt to restrict duties for providers who are not immunized or who have not yet received prophylactic antiviral therapy in attempt to prevent spread of the outbreak.
Avian Influenza
Influenza A virus infects humans and also can be found naturally in birds. Wild birds carry a type of influenza A virus, called avian influenza virus, in their intestines and usually do not get sick from them. However, avian influenza virus can make domesticated birds, including chickens, turkeys, and ducks, quite ill and can lead to death. The avian influenza virus is chiefly found in birds, but infection in humans from contact with infected poultry has been reported since 1996. A particular subtype of avian influenza A virus, H5N1, is highly contagious and deadly among birds. In 1997, in Hong Kong, an outbreak of avian influenza H5N1 occurred not only in poultry but also in 18 humans, six of whom died. In subsequent infections of avian influenza H5N1 in humans, more than half of those infected with the virus have died. In contrast to seasonal influenza, most cases of avian influenza H5N1 have occurred in young adults and healthy children who came in contact with poultry infected or surfaces contaminated with H5N1 virus. As of the end of 2007, 346 human infections with influenza H5N1 and 213 deaths (62%) were documented. Although transmission of avian influenza H5N1 from human to human is rare, inefficient, and unsustained, concern exists that the H5N1 virus could adapt and acquire the ability for sustained transmission in the human population. If the H5N1 virus gains the ability to transmit easily from person to person, a global influenza pandemic could occur. No vaccine for H5N1 current exists, but vaccine development is underway. The H5N1 virus is resistant to the adamantanes but likely sensitive to the neuraminidase inhibitors.
Tuberculosis
Tuberculosis (TB) is caused by the Mycobacterium tuberculosis complex. Most active TB is pulmonary (70%); the remainder is extrapulmonary (30%). Patients with active pulmonary TB typically have cough, scant amounts of nonpurulent sputum, and possibly hemoptysis. Systemic signs such as weight loss, loss of appetite, chills, night sweats, fever, and fatigue may also be present. Clinically, the provider is unable to distinguish pulmonary TB from other respiratory illness; however, certain risk factors may alert the provider to the possibility of tuberculosis. These risk factors are immigration from a country with a high prevalence rate, homelessness, exposure to active pulmonary TB, silicosis, HIV infection, chronic renal failure, cancer, transplantation, or any other state of immunosuppression.
Active pulmonary TB is transmitted via droplet nuclei from people with pulmonary tuberculosis during coughing, sneezing, speaking, or singing. Procedures such as intubation or bronchoscopy are high risk for the transmission of TB. Respiratory secretions on a surface lose the potential for infection. About 21% to 23% of individuals in close contact with persons with infectious TB become infected through inhalation of aerosolized bacilli. The probability of infection is related to duration of exposure, distance from the case, concentration if bacilli in droplets, ventilation in the room, and the susceptibility of the host exposed. Effective medical therapy eliminates communicability within 2 to 4 weeks of start of treatment.
If infected with TB, an individual may have development of active TB with symptoms or latent TB, which is asymptomatic. Time from infection to active symptoms or positive TB skin test results is about 2 to 10 weeks. The risk of development of active TB is greatest in the first 2 years after infection. Latent TB may last a lifetime, with the risk that it may later progress to active TB. About 10% of patients with latent TB have progression to active TB in their lifetime.
With transport of a patient who is known or suspected of having TB, respiratory precautions should be undertaken by the provider (in particular, a submicron mask). Patients should cover their mouth when coughing or sneezing or wear a surgical mask. In the event of suspected exposure to a patient with active pulmonary tuberculosis, the case and the exposure should be reported to the transport agency or public health authority. Close contacts should be monitored for the development of active TB symptoms. Two tuberculin skin tests should be performed, based on public health recommendations, on those closely exposed to patients with active TB. Because the incubation period after contact ranges from 2 to 10 weeks, the first test is typically done as soon as possible after exposure, and the second test is typically done 8 to 12 weeks after the exposure. If the provider or contact develops either active TB with symptoms or latent asymptomatic TB, as diagnosed with a new positive TB skin test, treatment should be sought.
Treatment for latent TB is typically isoniazid (INH) for 6 to 9 months. This single-drug regimen is 65% to 80% effective. For active TB, a four-drug regimen is typically used for 2 months: isoniazid, rifampin, pyrazinamide, and ethambutol. This regimen is followed by INH and rifampin for an additional 4 months. Several forms of multi–drug-resistant (MDR) TB and extensively drug-resistant (XDR) TB have been identified. These forms necessitate an aggressive multidrug regimen for prolonged periods of time and are dependent on the organism’s patterns of drug sensitivity and resistance. In all cases, a physician skilled in management of TB must initiate and monitor treatment and provide suitable follow-up. Public health officials must also be notified.
Severe Acute Respiratory Syndrome
Severe acute respiratory syndrome (SARS) is difficult to distinguish from other respiratory infections because patients have symptoms that are similar to other febrile respiratory illnesses. On initial presentation, reliance on respiratory symptoms alone is not sufficient to distinguish SARS from non-SARS respiratory illness. Fever is the most common and earliest symptom of SARS and is often accompanied by headache, malaise, or myalgia. In patients with SARS, high fever, diarrhea, and vomiting were more common as compared with other patients with other respiratory illnesses. Cough occurred later in the course of disease, and patients were less likely to have rhinorrhea or sore throat as compared with other lower respiratory tract illness. Because clinical features alone cannot reliably distinguish SARS from other respiratory illnesses, knowledge of contacts is essential. Contact with patients with known SARS, contact with SARS-affected areas, or linkage to a cluster of pneumonia cases should be obtained in the history.
Severe acute respiratory syndrome was first recognized in 2003 after outbreaks occurred in Toronto, Singapore, Vietnam, Taiwan, and China. The illness is caused by a coronavirus. The incubation period ranges from 3 to 10 days, with an average of 4 to 5 days from contact to symptom onset. About 11% of those with SARS eventually die, usually of respiratory failure. The risk of mortality is highly dependent on the patient’s age and presence of comorbid illnesses. The case fatality rate is less than 1% for SARS patients less than age 24 years and up to 50% for those age 65 years and greater or those with comorbid illness.
The coronavirus is found in respiratory secretions, urine, and fecal matter. Transmission is via droplet spread from respiratory secretions, with high-risk transmission during intubation and procedures that aerosolize respiratory secretions. Transmission can also occur from fecal or urine contamination of surfaces. There have been no confirmed cases of transmission from asymptomatic cases. Preliminary studies show that transmission likely occurs after the development of symptoms, with the peak infectious period 7 to 10 days after symptom onset and a decline to a low level after day 23 from onset of symptoms.
If SARS is suspected, providers must use all routine practices and additional precautions. Transport agencies may also elect to limit or avoid any procedures that may increase risk to personnel, including tracheal intubation, deep suctioning, use of noninvasive ventilatory support (continuous positive airway pressure [CPAP], bilevel positive airway pressure [BiPAP]), administration of nebulizer medication, and any other procedure that may aerosolize respiratory secretions. During the SARS outbreaks in Toronto, emergency medical services (EMS) medical direction modified directives such that paramedics did not intubate patients or deliver nebulized therapy in the prehospital setting. 10 Finally, personnel and systems must also notify the receiving facility of a patient suspected of SARS, which permits staff to have appropriate PPE in place and a suitable isolation room prepared for the patient.
Rash
Methicillin-Resistant Staphylococcal aureus
Skin infections with onset in the community or hospital may be caused Staphylococcus aureus. S. aureus is a bacterium that normally secretes beta-lactamases, rendering them normally resistant to antibiotics such as ampicillin and amoxicillin. Methicillin, a type of beta-lactam antibiotic, developed in 1959, was not broken down by these bacterial beta-lactamase enzymes. However, in the 1960s, infections of S. aureus were found to be resistant to methicillin and other beta-lactam antibiotics, resulting in the emergence of methicillin-resistant Staphylococcal aureus (MRSA).
In addition to skin and soft tissue infections, MRSA may less commonly cause severe and invasive infections such as necrotizing pneumonia, sepsis, and musculoskeletal infections, such as osteomyelitis and necrotizing fasciitis. MRSA skin infections typically present as necrotic skin lesions and are often confused with spider bites. The severity of MRSA skin infections may range from mild to severe. Unfortunately, no reliable clinical or risk factor criteria distinguish MRSA skin and soft tissue infections from those caused by other infectious agents.
Transmission of MRSA is mainly through hand contact from infected skin lesions, such as abscesses or boils. About 1% of the healthy population is also colonized with MRSA, mainly in the anterior nares but also in the pharynx, axilla, rectum, and perineum. Therefore, autoinfection may also be a route of infection. The transmissible period lasts as longs as skin lesions continue to drain or as long as the carrier state remains. Newborns, the elderly, and persons with immunosuppression are most susceptible.
Transmission of infection is prevented with routine precautions. Draining wounds should be covered with clean dry bandages. Contaminated surfaces should be cleaned with disinfectants effective against S. aureus, such as a solution of dilute bleach or quaternary ammonium compounds. One study has shown that ambulances may have a significant degree of MRSA contamination, highlighting the need for proper cleaning and decontamination of all equipment and the vehicle itself after every patient transport.
No data support the routine use of decolonization of MRSA with antiseptic agents or nasal mucopirocin. Decolonization may be considered in select circumstances, with multiple recurrent infections of MRSA or ongoing transmission in a well-defined group of close contacts. Little data are available on effective decolonization agents, but topical chlorhexidine gluconate or diluted bleach (3.4 g of bleach diluted in 3.8 L of water) is suggested.
With skin or soft tissue infections, any drainage should be cultured. Abscesses should be incised and drained. Antibiotic therapy may be considered with signs of cellulitis, systemic illness, associated immunosuppression, extremes of age, facial infection, or failure of initial incision and drainage. The choice of therapy should be dictated by local susceptibility patterns. Clindamycin, doxycycline, and trimethoprim-sulfamethosaxole (TMP-SMX) are considerations for treatment of CA-MRSA skin and soft-tissue infections. HA-MRSA may be resistant to many more classes of antibiotics, and vancomycin or linezolid may be necessary.
Measles
Measles is a viral disease that initially presents with a 2-day to 4-day prodrome of fever, cough, runny nose, and possibly conjunctivitis. In the prodrome stage, the provider is unable to clinically distinguish measles from any other viral upper respiratory illness. A measles rash follows, beginning on the hairline and then involving the face and neck, and over 3 days, proceeding downward and outward to the hands and feet. The rash produces discrete red maculopapular (flat and raised) lesions initially, which may become confluent. Initially, the lesions blanch and after 3 to 4 days become nonblanchable spots, which appear within 1 to 2 days before or after the maculopapular rash. Koplik spots, punctuate blue-white spots on the red buccal mucosa of the mouth, are pathognomonic for measles and alert the provider to the presence of measles.
Measles is transmitted via aerosol or droplet spread and is communicable from 4 days before appearance of the rash to 4 days after appearance. Providers likely encounter the patient in the transmissible stage and should use routine practices to prevent spread of disease.
The incubation period is approximately 10 days. Persons who have not been immunized or have never had measles (born after 1957) are susceptible to infection if exposed.
Rubella
Rubella is a viral disease with a prodrome that precedes rash. Clinical diagnosis alone is unreliable. The prodrome, which consists of fever, upper respiratory symptoms, and prominent lymphadenopathy, lasts 1 to 5 days and mostly presents in older children and adults. During the prodrome, rubella is clinically indistinguishable from any other viral URTI. A maculopapular rash that appears 14 to 17 days after exposure and lasts 3 days typically follows the prodrome. Like measles, the rash starts on the face and progresses downward. In contrast to a measles rash, the rash from rubella is fainter, does not coalesce, and is more prominent after a hot shower or bath. Associated symptoms may include arthralgia or conjunctivitis. Confirmation of rubella infection is with laboratory diagnosis of virus or antibody.
Rubella is transmitted from respiratory secretions via airborne transmission or droplet spread, with an incubation period of 14 to 17 days. Although rubella is most contagious when the rash is present, it may transmitted by subclinical or asymptomatic cases of rubella, and 7 days before the onset of rash.
Life-threatening complications of rubella include encephalitis and hemorrhagic disease, but these are uncommon. The main objective of immunization is prevention of congenital rubella syndrome (CRS), the main complication of rubella. No specific treatment exists for rubella, only preventative vaccination. Rubella immunization is part of the routine childhood vaccinations, administered as a live vaccine along with measles and mumps as “MMR.”
With exposure to patients later diagnosed with rubella, immunity of the contact should be assessed. Subsequent immunization of the nonimmunized contact does not prevent infection or illness. In adults, rubella is generally a mild febrile disease, and control measures are aimed at prevention of spread to nonimmunized pregnant women. In the case of spread, patients suspected of having rubella should be isolated with routine precautions in place.
Varicella
Like measles and rubella, varicella starts with a prodrome that subsequently leads to a rash. In children, the prodrome of fever and malaise may be absent. Unlike measles and rubella, varicella infection, chickenpox, can be clinically diagnosed by the provider based on a more pathognomonic rash. The pruritic rash progresses from macules to papules and then to vesicles, which later crust over. The vesicles are unilocular and collapsible, in contrast to the multilocular and noncollapsible vesicles of smallpox. Lesions start on the scalp, progress to the trunk, and later move to the extremities.
Varicella virus infection that leads to chickenpox typically lasts 3 to 4 days, with an incubation period of 14 to 16 days. Transmission is via airborne droplets from the respiratory tract or via inhalation of aerosolized vesicular fluid from skin lesions. Chickenpox is transmissible 1 to 2 days before the onset of rash until all papules become crusted.
Complications in children include secondary bacterial skin infections, pneumonia, and dehydration. Nonimmunized adults may have more severe complications, including encephalitis, transverse myelitis, hemorrhagic varicella, and even death. In the United States, only 5% of the reported cases of varicella are from adults, but 35% of the mortality occurs in adults. The case fatality rate is 1 per 100,000 cases in children aged 1 to 14 years but 25.2 per 100,000 cases in adults aged 30 to 49 years.
Maternal varicella 5 days before to 48 hours after delivery may result in neonatal infection and subsequent mortality rates as high as 30%. Varicella infection in the mother at 20 weeks of gestation can lead to congenital varicella syndrome, which includes skin scarring, extremity atrophy, and eye and neurologic abnormalities.
Cases of chickenpox should be excluded from public places until the vesicles become dry. In the hospital, strict isolation measures should be undertaken to avoid contact with susceptible persons with immunocompromise. Articles soiled by discharges from the nose and throat should be disinfected.
If exposed to chickenpox, contacts should assess susceptibility based on immune status. If previously infected or vaccinated, contacts are immune. Susceptible nonimmune contacts have three choices to prevent infection: vaccination, varicella zoster immunoglobulin, or antiviral drugs. Varicella vaccine can prevent illness or attenuate severity if used within 3 days of contact. Vaccine is recommended in susceptible individuals. Varicella zoster immunoglobulin (VZIG) is recommended for newborns, persons with immunocompromise, and pregnant women and can also modify severity or prevent illness if given within 96 hours of exposure. Antiviral drugs such as acyclovir, if used within 24 hours of onset of rash, can reduce the severity of disease. These drugs are not recommended for routine postexposure prophylaxis but can be considered in persons over 13 years of age and those with immunocompromise.
Bites
Bites necessitate treatment for the physical injury itself and for the infectious disease exposure from the bite. Infection rates from bites mainly depend on the animal that has caused the bite and the site of injury. Cat bites can have an infection rate of up to 50%; about 10% of dog bites become infected. Bites on the face, scalp, hand, wrist, foot, or joints have the highest rate of infection. Hands are the most common site of human, dog, and cat bites. Bite infections may cause cellulitis, osteomyelitis, abscess, septic arthritis, or even septicemia. In addition to antibiotic therapy, bites may also necessitate treatment with rabies prophylaxis, tetanus prophylaxis, and HIV and hepatitis B prophylaxis. Prophylactic antibiotic treatment for bites depends on the specific infectious agents most commonly associated with the particular animal. Finally, personnel should also be aware of the risk of transmission of hepatitis C from human bites.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





