CHAPTER 17. Thoracic Trauma
Reneé Semonin Holleran
Competencies




1. Identify clinical indications of thoracic injuries.
2. Recognize signs and symptoms of life-threatening thoracic injuries.
3. Perform appropriate critical interventions to manage a thoracic injury.
Thoracic injuries present a demanding challenge for patient transport. Thoracic injury remains second only to central nervous system injury as the leading cause of all trauma deaths. 1 In the pediatric population, with the exception of lung contusions, serious injuries to vital thoracic structures are associated with a mortality rate of more than 60%. 15 An understanding of the severity and mechanism of injury, management concerns of specific thoracic injuries, and special transport considerations aid the transport team in providing care.
Thoracic trauma is classified by either the mechanism of injury or the degree to which the injury is life threatening. Classification of thoracic trauma by mechanism of injury encompasses two categories: blunt and penetrating traumas. Blunt trauma is associated with motor vehicle crashes, compression injuries, falls, and assaults. Penetrating trauma occurs as a result of gunshot wounds, stab wounds, and impalement.
Thoracic injuries may also be categorized as life-threatening or potentially life-threatening conditions. Life-threatening thoracic conditions are airway obstruction, tension pneumothorax, massive hemothorax, open pneumothorax, flail chest, cardiac tamponade, aortic rupture, and myocardial rupture. Potentially life-threatening conditions are myocardial contusion, pulmonary contusion, aortic disruption, tracheobronchial disruption, esophageal rupture, and diaphragmatic disruption. Because many of the thoracic injuries are life threatening, rapid transport to a regional trauma center or tertiary care setting may be indicated. 5,13,18
Special considerations for in-flight care of the patient with thoracic trauma relate to altitude changes and gas expansion. As previously discussed in transport physiology, gases expand with increasing altitude. Because of this expansion, a patient with an untreated pneumothorax or a nonfunctioning chest tube may be at great risk for development of a tension pneumothorax. 1,18,25 As part of the anticipatory planning and management of care during transport, the way changes in altitude may affect a patient with thoracic injuries must be considered.
The greatest threat in the management of a patient with a thoracic injury is hypoxia. 1,18,25 In addition to thoracic injury, the contributing causes of hypoxia may be decreased blood volume, failure to ventilate the lungs, ventilation-perfusion mismatches, or pressure changes within the intrapleural space. The ABCDEs of resuscitation serve as a framework for management of each injury. The ABCDE framework assists in quick detection of life-threatening injuries and implementation of rapid interventions.
LIFE-THREATENING THORACIC INJURIES
Tension Pneumothorax
Etiologic Factors
Both blunt and penetrating thoracic traumas cause tension pneumothorax. A tension pneumothorax can also occur as a complication of the treatment of an open pneumothorax. Air progressively accumulates under pressure, and the flap of the injured lung acts as a one-way valve; air is allowed to enter the pleural space on inspiration but not allowed to escape on expiration.
Pathophysiologic Factors
Ventilation is inadequate because the air entering the pleural space increases the intrapleural pressure with each inspiration, which causes collapse of the ipsilateral lung and a mediastinal shift to the opposite side, leading to compression of the contralateral lung (Figure 17-1). Perfusion becomes inadequate because of decreased venous return to the heart as a result of the increased intrapleural pressure and shift of mediastinal structures.
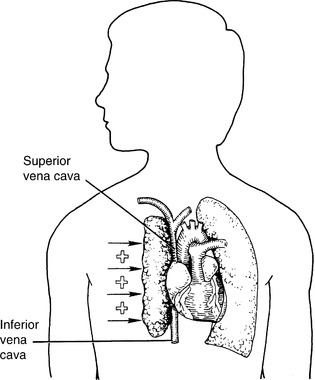 |
| FIGURE 17-1 Tension pneumothorax. (From Sheehy SB: Emergency nursing: principles and practice, ed 4, St Louis, 1992, Mosby.) |
Assessment
The mechanism of injury establishes a high index of suspicion. The patient with a tension pneumothorax has severe respiratory distress, dyspnea, and cyanosis. Agitation and anxiety are common. 1,11,16,19 Clinical evidence of shock may be present. Breath sounds are either decreased or absent over the involved hemi-thorax. The trachea should be assessed because a shift to the unaffected side occurs as intrapleural pressure increases. As air passes into the tissues, subcutaneous emphysema can be palpated, causing decreased preload into the heart. Jugular venous distention, a late sign, occurs because of the increased intrapleural pressure. Constant observation of the patient’s chest excursion is important during transport because auscultation is next to impossible.
Interventions
The immediate life-saving intervention is rapid decompression of the pleural space. To release the intrapleural pressure, a large-bore needle should be placed into the pleural space, specifically into the second intercostal space, two-finger breadths lateral to the sternal border on the affected side. The needle should then be placed superior to the rib margin to avoid the intercostal artery. The anterior site is used for avoidance of the internal mammary vessels. 5,6,16,19 If a tension pneumothorax is present, a rush of air may be heard. This rush of air probably is not appreciated during transport. Instead, immediate improvement of the patient symptoms and a return to hemodynamic stability should be seen.
Evaluation
Constant reevaluation of the patient’s cardiopulmonary status is warranted. If a chest tube is placed and a persistent air leak occurs, the presence of a tra-cheobronchial disruption must be considered.
Massive Hemothorax
Etiologic Factors
Massive hemothorax develops as a result of blunt or penetrating injuries of intrathoracic organs or laceration of an intercostal artery. The rapid and massive accumulation of blood and fluid in the pleural space can result in severe hemodynamic compromise.
Pathophysiologic Factors
The compliant lung offers little resistance to a large amount of blood becoming sequestered in the pleural space (Figure 17-2), and hypovolemic shock results. Compression of the ipsilateral lung occurs from the accumulation of blood, and a mediastinal shift can occur from compression of the contralateral lung. In this way, ventilation-perfusion mismatches happen.
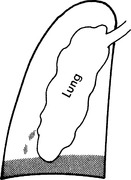 |
| FIGURE 17-2 Hemothorax. (From Sheehy SB: Emergency nursing: principles and practice, ed 4, St Louis, 1992, Mosby.) |
Assessment
The mechanism of injury is vital to the initial assessment of a suspected massive hemothorax. Because of the decrease in blood volume, manifestations of hypovolemic shock may appear. Altered mentation, decrease in blood pressure, increase in heart rate, and signs of peripheral vasoconstriction are common. Breath sounds are decreased or absent over the involved hemothorax, and chest excursion on the affected side is decreased. Unlike the symptoms of cardiac tamponade, the trachea is generally in the midline, and the neck veins are flat unless a hemopneumothorax is present. 5,21
Interventions
Restoration of lost blood volume is of primary importance, and an initial response is to achieve intravenous access with at least two large-bore catheters and to administer crystalloids or colloids. Supplemental oxygen should be administered. Endotracheal intubation may be necessary. Emergent management involves placement of a tube thoracostomy.
Fluid resuscitation must be carefully monitored. The transport team must also be cognizant that excessive fluid resuscitation, particularly in penetrating thoracic trauma, can be detrimental and lead to hypoxemia or worsening of hemothorax or cardiac tamponade.
In cases of massive hemothorax, the transport team may consider autotransfusion. 3,4 The use of autotransfusion in thoracic trauma has been greatly debated because of the potential effect of anticoagulants and abdominal contaminants. 2,12 Considerations related to autotransfusion are transport delay during supply setup and space limitation during transport. In situations of prolonged transport times, isolated chest trauma, conflicting religious beliefs, or cross-matching difficulty, autotransfusion may serve as a bridge until definitive care is provided.
Many transport programs today have access to blood and blood products that can be used when autotransfusion is not available, the wound is potentially contaminated, or time is an issue. In any resuscitation situation in which bleeding is actively occurring, the patient must be closely monitored to prevent additional bleeding. Resuscitation should occur cautiously until bleeding is controlled. 12 Rapid transport to definitive care should be one of the primary focuses of the team. 6
Evaluation
Transport team members must constantly reassesses the ventilator neurologic and hemodynamic status of the patient and monitor the parameters of the patient’s response to volume replacement.
Open Pneumothorax
Etiologic Factors
A penetrating object causes an open pneumothorax, or sucking chest wound. Air enters the pleural space through the opening or defect in the chest wall (Figure 17-3).
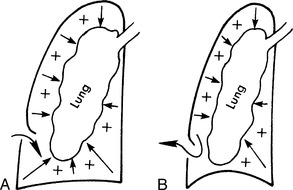 |
| FIGURE 17-3 Sucking chest wound. A, Inspiration. B, Expiration. (From Sheehy SB: Emergency nursing: principles and practice, ed 4, St Louis, 1992, Mosby.) |
Pathophysiologic Factors
If the diameter of the chest-wall defect is greater than the diameter of the patient’s trachea, air moves through the chest wound rather than through the trachea and airways. The defect in the thoracic wall leads to an equilibration of atmospheric and pleural pressure. The result is loss of the negative intrathoracic pressure, which leads to respiratory insufficiency. Air in the pleural space promotes collapse of the ipsilateral lung and a mediastinal shift to the unaffected side. The mediastinal shift and loss of normal negative intrathoracic pressure produce decreased venous return to the heart and cardiac insufficiency.
Assessment
A penetrating injury to the thorax should lead the transport team to closely assess the thorax to determine whether a sucking chest wound is present. The patient is in respiratory distress, with tachypnea and grunting, and as air enters and leaves the pleural space through the chest-wall defect, a sucking noise may be heard during respiration. Clinical manifestations of shock occur as a result of intermittent obstruction of venous return. 4.5. and 6.12,14,19,21
Interventions
In the prehospital setting, the wound should be covered, but not sealed, with an occlusive dressing. A dressing taped on three sides creates a flutter-valve effect; air is prevented from entering the chest on inspiration but is not prevented from leaving the chest on expiration. If an occlusive dressing is used and a defect in the lung exists, a tension pneumothorax may develop because the air is not allowed to escape from the pleural space.
If a tension pneumothorax develops, the occlusive dressing should be immediately removed. The patient may need the placement of a chest tube to treat the underlying lung defect. 5,25 If the patient’s ventilation and oxygenation continue to deteriorate, the team should immediately prepare to intubate. Maintenance of intravenous access is also imperative as a route for volume resuscitation and medication administration.
Evaluation
Evaluation must consist of continuous monitoring of the patient’s cardiopulmonary status. Assessment parameters for expanding pneumothoraces are limited during transport because of the background noise levels. Astute evaluation of the patient’s chest pain, tachycardia, increasing dyspnea, tracheal deviation, and development of subcutaneous emphysema and neurologic status prompts the transport nurse to begin hemodynamic compromise. 1,25
Flail Chest
Etiologic Factors
A flail chest usually occurs as a result of blunt thoracic trauma. Multiple rib fractures cause separation of a portion of the rib cage and loss of stability of the chest wall. The flail segment usually involves the anterior or lateral chest wall because heavy posterior muscles and the scapula protect the posterior chest wall.
Pathophysiologic Factors
Paradoxical chest movement interferes with the normal “bellows” function of the thoracic cage, causing inadequate gas exchange. The underlying pulmonary contusion causes progressive respiratory insufficiency. The instability of the chest wall and the pain from the fracture sites lead to hypoventilation and subsequent hypoxemia.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






