CHAPTER 19. Orthopedic Trauma
Reneé Semonin Holleran
Competencies




1. Perform an assessment of an injured extremity before and during transport.
2. Appropriately apply the immobilization device needed for patient transport.
3. Identify and treat potential complications related to musculoskeletal emergencies.
A simple fracture or dislocation can become a devastating injury and result in severe permanent disability. Even a moderate sprain, if inadequately treated, can result in an unnecessarily extended disability and can lead to recurrent injuries.
The hands of a pianist, the elbow of a pitcher, the legs of a dancer are all vital to each of these people. Although musculoskeletal injuries are rarely fatal, they often result in long-term disability that accounts for millions of dollars lost to the economy each year. 14 The first care provided to a patient with a fracture, dislocation, or severe sprain often determines the ultimate results that occur as a consequence of the injury. 8 The transport team can often prevent permanent disability with a prompt temporary measure, such as immobilization or splinting, especially in patients with multiple traumas when more definitive management must be postponed until life-threatening injuries have been taken care of adequately.
MUSCULOSKELETAL SYSTEM
A basic understanding of the composition and function of the musculoskeletal system is essential to proper management of orthopedic emergencies and ultimately to the welfare of the patient as a whole. The musculoskeletal system is composed of bones, ligaments, muscles, joints, tendons, blood vessels, and nerves. The function of the musculoskeletal system is to allow movement, provide support, and protect internal organs. 1.2.3.4. and 5.
Bone is a living structure with its own neurovascular innervation and capacity to heal. Bone is a specialized connective tissue with a calcified collagenous intercellular substance and is either cancellous or compact. The calcium content of bone depends on many factors such as parathyroid hormone and estrogen, dietary intake, and stress. An acid-base balance with a slight decrease in pH can cause bone demineralization. 1.2.3.4. and 5.
DEFINITION
An orthopedic injury, a trauma to the axial skeleton, is rarely considered an emergency. However, it does require urgent care. In terms of orthopedic involvement with underlying organs, emergencies can exist. An example is the fracture or dislocation of the knee or elbow. These are extremely painful injuries, and they also can cause permanent damage to nerves and vessels distal to the injury if not taken care of immediately. Table 19-1 lists various orthopedic injuries with possible complications.
| Injury | Possible Complications |
|---|---|
| Clavicle fractures | Brachial plexus compression or damage; pneumothorax or hemothorax |
| Humerus fractures | Injury to brachial artery or radial nerve |
| Pelvic fractures | Injury to bladder, urethra, rectum |
| Distal femoral shaft fractures | Femoral or popliteal vessel injury |
| Proximal tibia fractures | Compression of the anterior tibial compartment; tibial nerve injury |
| Clavicular head dislocation | Compression of trachea, subclavian, and carotid arteries |
| Posterior elbow dislocation | Compression of brachial artery |
| Posterior hip dislocation | Aseptic necrosis of the femoral head and sciatic nerve damage |
| Knee dislocation | Compression of the popliteal vessel |
| Ankle dislocation | Compression of the pedal artery |
CLASSIFICATION OF ORTHOPEDIC INJURIES
When force is applied to a limb, the energy of the impact dissipates to deform supporting structures. An excessive amount of force may damage more than one structure in the line of force. 6,11 This type of stress to the axial skeleton and its supporting structures can cause various types of injuries, including fractures, dislocations, sprains, tendon injuries, and strains.
Fractures
A fracture is defined as any break in the continuity of the bone or cartilage, and it may be either complete or incomplete, depending on the line of fracture through the bone. 1.2.3.4. and 5. Fractures generally are classified as closed or open. If the skin is unbroken, the fracture is technically closed, regardless of the number of fractures; if the skin is broken, the fracture is open, although it may be simple and minor in nature. Any broken skin in the area of a fracture must be included in the report. An open fracture is more serious because of the risk of infection. Figure 19-1 illustrates nine different types of fractures as defined by radiographic appearance.
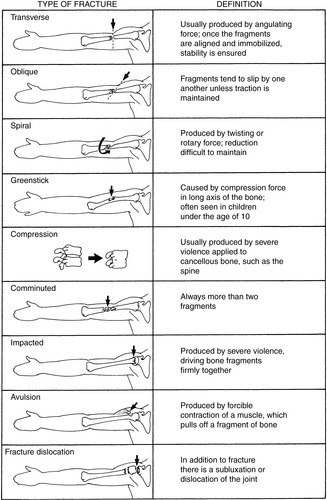 |
| FIGURE 19-1 Fractures according to radiographic appearance. |
Fractures of the long bone may produce steady slow bleeding and can result in 750 mL of blood loss from the humerus or tibia and 1500 mL of blood from each femur. 1.2.3.4. and 5. These patients must be watched closely for shock, and the long bone fracture should be immobilized for comfort. Another risk associated with fractures, even uncomplicated ones, is that of fat embolism, which can cause varying degrees of respiratory distress, including respiratory failure. Signs and symptoms of fat embolism are petechial rash, diffuse pulmonary infiltrates, hypoxemia, confusion, fever, tachycardia, and tachypnea. Patients at highest risk of fat embolism are those with long bone fractures of the lower extremity. 1.2.3.4. and 5.
Dislocations
A dislocation is the displacement of the normal articulating ends of two or more bones. A complete dislocation causes a tearing of the ligaments. A dislocation may also be described as compound when the joint is exposed to the outside air. Joints that are frequently dislocated are shoulders, elbows, fingers, hips, and ankles. Less frequently seen are dislocated wrists or knees. A dislocation is referred to as subluxated when the displacement is incomplete.
MECHANISMS OF INJURY
Multiple mechanisms may cause injury to the musculoskeletal system, including motor vehicle collisions (one of the most common); falls, particularly to the elderly; sports, such as football and soccer; and routine activities, such as cleaning around the house. Either accelerating or decelerating forces may cause injury to bones, muscles, ligaments, and their surrounding nerves and blood vessels. An important point to remember is that when a force is applied to the musculoskeletal system and causes an injury, the surrounding tissue and organs may be injured along with the bones and muscles. 1,7,12,13
ASSESSMENT OF AN ORTHOPEDIC INJURY
In patients with multiple trauma, musculoskeletal injuries are rarely life threatening. Thus, before assessing possible fractures, the nurse should evaluate for life-threatening injuries. The evaluation should begin with attention to airway, breathing, and circulation (the ABCDEs). Only when the patient has been fully evaluated and the condition is judged stable should an attempt be made to treat an injured limb. For adequate assessment data, a good history is important. This information can be obtained by talking to the first respondents on the scene or by reading the medical record. As previously discussed, an injury can often be anticipated by knowing the mechanism of injury and the circumstances under which it was sustained. To document a musculo-skeletal assessment, certain orthopedic terms may be used. Box 19-1 lists common orthopedic terms.
BOX 19-1
Common Orthopedic Terms
Abduction: Movement of a body part away from the body’s mid line.
Adduction: Movement of a body part toward the mid line.
Ankylosis: Decreased range of motion caused by stiffening of the joint.
Dorsiflexion: Movement of the hand or foot upward.
Eversion: Movement of the ankle outward.
Extension: Movement of the joint to open it or to maximally increase its angle.
External rotation: Outward rotation.
Flexion: Bending of the joint.
Hyperextension: Extension past neutral.
Internal rotation: Inward rotation.
Inversion: Movement of the ankle inward.
Kyphosis: Round back; increased flexion of the spine.
Lordosis: Sway back; increased hyperextension of the spine.
Plantar flexion: Movement of the foot downward.
Pronation: Movement of the forearm to place the palm downward.
Rotation: Movement of one bone turning on another.
Scoliosis: Lateral curvature of the spine.
Supination: Movement of the forearm to place the palm upward.
Torsion: Twisting of the bone on its axis.
Valgus: Deformity that causes an outward turning of the foot or toe (e.g., genu valgus or knock kneed).
Varus: Deformity that causes an inward turning of the foot or toe (e.g., genu varus or bow legged).
Open fractures produce greater blood loss and risk of infection than closed fractures and so demand more immediate attention. However, closed fractures must be carefully monitored, too. 18 The examination for fractures should be organized by body areas, with observation first for obvious deformities. If conscious, the patient should be asked to try to move each extremity. If a fracture or dislocation exists, movement or attempted movement is almost always painful, or extremely limited with a dislocation. Range of motion, or lack of it, needs to be recorded. The extremities should be palpated proximally to distally, with evaluation for pain, displacement, crepitus, and decreased or absent pulses. The transport team should gently press laterally inward on the iliac crests and also press gently down on the symphysis pubis to assess for increased pain and to determine pelvic stability6 and on the sternum and rib cage to determine stability of the ribs.
The classic signs of musculoskeletal trauma include deformity, localized swelling, pain, pallor, diminished or absent pulses, paresthesia, and paresis or paralysis. 6 If the patient is conscious, the transport team can ask about the patient’s pain and its location. Peripheral pulses (especially those distal to the fracture site) should be checked bilaterally for presence and quality. Paresthesia should be checked in the conscious patient by touching or pinching the affected extremity and assessing for altered sensation. Always compare patient responses on each side.
Capillary refill should be monitored and skin temperature noted. 16,18 Paralysis at the time of the injury or ensuing paralysis on repeated examination may influence the transport location.
Joints above and below the fracture site or point of injury need to be evaluated. Neurovascular status assessments of the affected extremity should be done frequently, but especially before and after transport.
Children need special consideration in evaluation for musculoskeletal injuries. Because their bones are more flexible than those of adults, greater force is often necessary to cause a fracture. Therefore, a child who has sustained even minor rib fractures must be assumed to have sustained serious internal injuries. The transport team should suspect splenic or diaphragmatic injury in a child with low rib fractures. Injury to the flexible skeleton of the young child may cause different results than in the adult patient. 1.2.3.4. and 5.
MANAGEMENT OF ORTHOPEDIC INJURIES
Improper handling of a patient with an injury to the musculoskeletal system may convert a simple problem into a much more serious one. The closed wound may become an open one, a clean wound may become grossly contaminated, or blood vessels and nerves may be seriously injured. The five basic principles for management of fractures and dislocations are: (1) avoid unnecessary handling; (2) immobilize; (3) apply clean dressings to wounds; (4) control hemorrhage with direct pressure; and (5) check for the “5 Ps” distal to the injury—pain, pulselessness, paresthesia, pallor, and paralysis. 1,16.17. and 18.
Wound Management
Local wound care is initiated by assessing the wound for evidence of severe hemorrhage or debris and the presence of bone ends protruding through the skin. These findings should be noted on the chart, and a dry sterile dressing should be applied. So that circulation is not further impaired, no attempt should be made at wound cleansing or pulling the bones back beneath the skin. Severe hemorrhage is generally controllable with direct pressure over the wound or over the arteries just proximal to the wound. 7 Good wound care is as important to a positive outcome as is good splinting. This technique should not be overlooked. Tetanus status should be noted at some point during patient care.
Splinting
Good emergency care rendered to a patient with any type of orthopedic injury decreases hospital stay, speeds recovery, and lessens the chance of serious complications. Because the extent of injury is difficult to assess initially, the best method is to assume a fracture is present and immobilize it until further evaluation can be made with radiography.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





