Vertebroplasty and Kyphoplasty
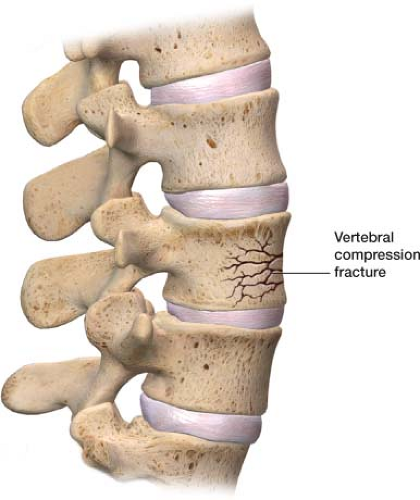
Vertebral compression fractures (VCFs) are a significant problem. In the United States, more than 700,000 age-related osteoporotic compression fractures occur per year. One in two women and one in four men aged 50 years and older will have an osteoporosis-related fracture in their remaining lifetime.1 The lifetime risk of VCFs is 16% in women and 5% in men.2 VCFs are of significant importance; they can lead to chronic pain and kyphotic deformity, which can decrease pulmonary function and impair mobility.3
VCFs occur for a number of reasons, the most common being osteoporosis. The second most common cause of VCFs is tumors, both benign and metastatic. Cancers that tend to metastasize to the bone originate in the breast, lung, thyroid, kidney, and prostate. The bones in the axial skeleton, ribs, pelvis, and spine are normally the first involved. In breast cancer, pathologic fractures are common because of the lytic nature of the lesions. In lung cancer, they are uncommon because of patient’s short lifespan, and in prostate cancer, they are rare, because the lesions tend to be osteoblastic rather than lytic. The third most common cause of VCFs is trauma.
Patients with VCFs present with deep focal pain at the level of the fracture. Activity exacerbates the pain, and lying down relieves it. Any palpation over the area elicits pain. New onset of back pain in a patient with known history of cancer warrants evaluation for compression fracture from metastatic disease. Plain x-rays can confirm a fracture.
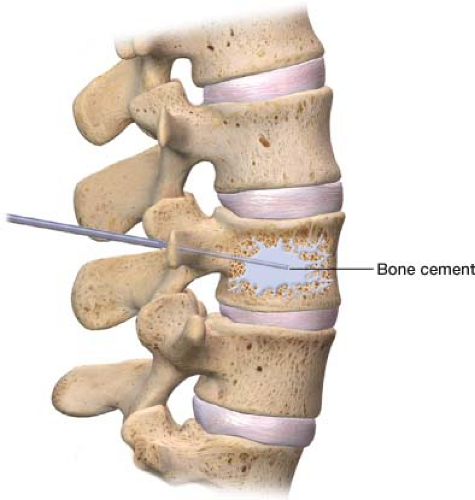
Vertebroplasty and kyphoplasty are two minimally invasive procedures used to treat pain from VCFs (Fig. 25-1). Both procedures also prevent further pain and functional decline because of instability stemming from the fractured vertebral body. Vertebroplasty, which was initially developed for the treatment of aggressive spinal hemangiomas, was first performed in France in 1984 and was introduced in the United States in 1993. Kyphoplasty was later introduced in 1998. Both procedures involve injecting a cement-like substance, polymethyl methacrylate, into a fractured vertebral body via a large bore needle under fluoroscopy (x-ray guidance). They significantly reduce pain and improve mobility in patients with VCFs.4 Kyphoplasty, which is slightly more invasive than vertebroplasty, involves inflation of a balloon, creating a cavity prior to the injection of bone cement. Kyphoplasty also poses a lower risk of bone cement leakage. Both procedures
are performed on an outpatient basis (Figs. 25-2 and 25-3).
are performed on an outpatient basis (Figs. 25-2 and 25-3).
When to use
Vertebroplasty and kyphoplasty are used for stability, pain relief, and to improve mobility in patients with VCFs because of a variety of reasons such as osteoporosis, benign tumors, multiple myeloma, metastatic tumors, and trauma.5 Patients who are likely to benefit are those with a well-localized, deep, intense pain associated with imaging of a new or progressive compression fracture.6 It has been reported that 95% of people treated with these two procedures immediately experienced partial or complete relief from their pain.7 In 91% of patients receiving these treatments, required significantly less daily oral analgesic.8 However, recent studies have challenged the merits of these two procedures.
Magnetic resonance imaging (MRI) is the gold standard for imaging VCFs. An MRI allows for the evaluation of the central spinal canal and neuroforamen, and makes possible identification of other potential sources of pain. When ordering an MRI to investigate a VCF, sagittal short tau inversion recovery (STIR) images should be requested. STIR distinguishes new or unhealed fractures from healed fractures. New or unhealed fractures show hyperintense signals within the bone marrow.
Treatment of VCFs varies. Initial noninterventional conservative treatment includes a nonsteroidal anti-inflammatory drug, a waiting period, and a back brace as needed. Even with medical management, 33% patients with VCFs have persistent pain. Bed rest is often useful for pain reduction but can result in increased bone loss caused by inactivity, further increasing the risk of vertebral fracture.9 In addition, medical management does not prevent the development of kyphotic deformity. Although surgery is an option, many people who develop VCFs are elderly and not ideal surgical candidates. The poor bone quality of osteoporotic fractured vertebrae, when fixated with screws, is a primary reason that surgical fixation often fails.10 Patients with cancer who have metastatic VCFs may also be poor surgical candidates. Those who are
suitable surgical candidates may not want to go through the postsurgical recovery process.
suitable surgical candidates may not want to go through the postsurgical recovery process.
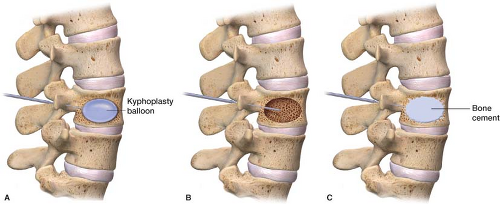 Figure 25-3 A. Kyphoplasty: A balloon is inflated to create a cavity before bone cement is injected. B. Cavity in which the bone cement is to be injected. C. Bone cement placed into the cavity for pain relief and stabilization of the VCF.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|