Abdominal Pain
Establishing a proper differential diagnosis, ordering a workup, making a diagnosis, then medically or surgically treating the underlying cause of a patient’s abdominal pain is reserved for general medicine texts and is beyond the scope of this book. This chapter will focus on symptom-oriented chronic pain management. How to analyze symptoms, and how to treat those symptoms. The focus of this section is not to help you diagnose the many causes of abdominal pain but rather to help you understand the painful symptoms. History taking and thorough examination are critical in understanding the nature of those painful symptoms that can be tied to a diagnosis and those that can not.
The pain can best be addressed by careful characterization of the symptoms. A pain history includes the PQRST:
|
Teasing out the aggravating and relieving factors is critically important, especially in chronic abdominal pain. Patients with chronic abdominal pain may have an exacerbation of their symptoms with certain types of food or medication. Certain activities may trigger the patient’s abdominal pain. Stressful life events often precede an exacerbation of symptoms. Stress, which is defined as an acute threat to homeostasis, shows both short- and long-term effects on the functions of the gastrointestinal tract. Stress leads to an alteration of the brain–gut interactions (“brain–gut axis”), ultimately contributing to the development of a broad array of gastrointestinal disorders. Major effects of stress on gut physiology include (1) alterations in gastrointestinal motility; (2) increase in visceral perception; (3) changes in gastrointestinal secretion; (4) increase in intestinal permeability; (5) negative effects on regenerative capacity of gastrointestinal mucosa and mucosal blood flow; and (6) negative effects on intestinal microbiota.1 Aggravating factors should be targeted in the treatment plan.
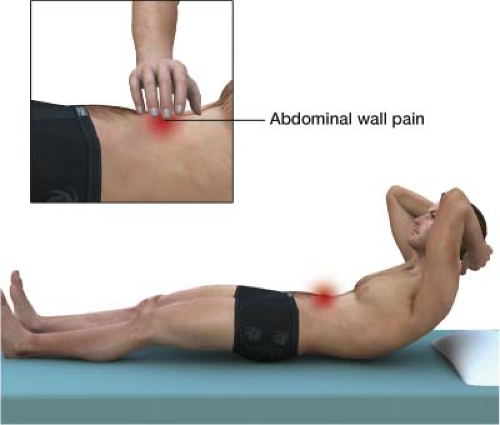
When the symptoms of abdominal pain have been worked up and there is still no known diagnosis, the goal of examination is to determine if the pain is visceral or somatic. In Carnett test, the site of maximal abdominal pain is identified. The patient is asked to tense the abdominal musculature by attempting to sit up. Increased pain with tension of the abdominal musculature suggests abdominal wall etiology (Fig. 4-1). In one common scenario, patients develop abdominal wall neuromas after surgery. There is no diagnostic imaging test for abdominal wall neuromas.
The principles provided here will give you the tools to alleviate your patient’s pain without hindering your ability to treat the disease generating it. Primary care doctors, GI specialists, urologists, and general surgeons are trained to evaluate the causes of abdominal pain and treat the underlying condition. The goal will be to correct the root of the underlying problem while managing the patient’s pain. Statistically, there are a number of chronic cases you will encounter for which we currently do not have the ability to establish a cause-and-effect diagnosis. Despite the best diagnostic tools available, the cause of a patient’s chronic abdominal pain often remains unclear. Chronic abdominal pain is
less likely than acute abdominal pain to reveal underlying organic pathology. In those cases, we understand the nature of the symptoms and can employ treatment modalities that work well for those symptoms. Be forewarned, however, that some chronic abdominal pain—such as that of unknown etiology despite full medical workup—is difficult to treat. Abdominal pain caused by cancer is covered in Chapter 3, Cancer Pain.
less likely than acute abdominal pain to reveal underlying organic pathology. In those cases, we understand the nature of the symptoms and can employ treatment modalities that work well for those symptoms. Be forewarned, however, that some chronic abdominal pain—such as that of unknown etiology despite full medical workup—is difficult to treat. Abdominal pain caused by cancer is covered in Chapter 3, Cancer Pain.
There are four basic sources of abdominal pain. They are visceral, somatic, chronic pain post abdominal surgery and referred.
Visceral
Visceral abdominal pain is pain that comes from an organ. Organs that are hollow—like the intestine—are much more likely to generate pain than a solid organ, like the liver. Unlike pain in other parts of your body, cutting a visceral organ—like the intestines—during surgery is not painful. Visceral pain is elicited with distension, compression, or torsion of an organ. Visceral pain is not well localized and often described as dull and achy. This is because there are a small number of visceral afferent nerves covering a large area. In contrast to this, when a painful sensation is felt at the pad of a finger it is sharp and detailed; in the finger there are a large number of nerves to cover a small area. A larger visceral area, such as the liver, has many less afferent nerves to help the body localize the pain.
Somatic
Somatic structures are the underlining support structures of the abdominal cavity—for example, the fascia, muscles, and peritoneum. Somatic pain is often well localized, and typically described as sharp and focal. A common aggravating factor is movement. An example of somatic abdominal pain is an abdominal wall neuroma, which is entrapment of a branch of the anterior cutaneous nerve as it courses through the abdominal wall muscle. A good example of the interplay of visceral and somatic pain is appendicitis. When the appendix is inflamed, the visceral pain is not well localized. The pain may be described as deep and dull. As the abdominal wall later comes in contact with the inflamed appendix, the pain becomes sharp and localized (Fig. 4-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree