Postoperative Pain
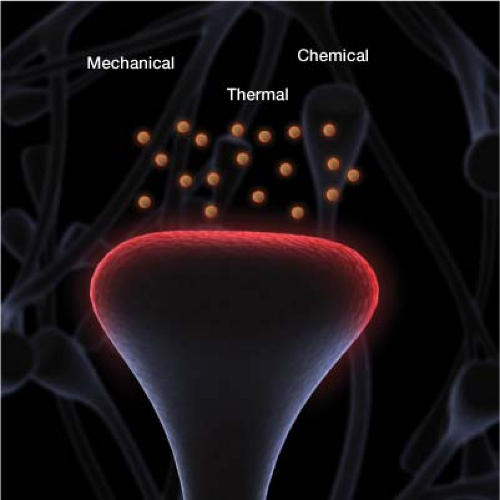
Pain after surgery is primarily derived from acute tissue manipulation. During surgery, inflammatory factors such as prostaglandins, bradykinin, and substance p are released. These increase the sensitivity of tissue pain receptors known as nociceptors (Fig. 8-1). Nociceptors are triggered by intense mechanical, chemical, or thermal noxious stimuli. For the most part, postsurgical pain is nociceptive.
In some cases, there can also be neuropathic pain, which occurs when a nerve is damaged. When a nerve is cut, it is engulfed by inflammatory molecules. Molecules such as tumor necrosis factor alpha act on injured nerve axons to pathologically increase their electrical activity until it becomes aberrant.1 When an injured nerve fires spontaneously and irregularly, this is neuropathic pain. It is often felt as a burning, electric, shooting pain. Patients with nerve damage simultaneously experience increased pain, and sensory loss.
Pain is an individual, multifactorial experience influenced by culture, previous pain episodes, beliefs, mood, and ability to cope. Before surgery it is important to identify which patients are more likely to experience high levels of postoperative pain. Risk stratification preoperatively can be helpful. Some risk factors for higher postoperative pain levels include the following.
Patients already taking opioids, have baseline pain requirements and higher tolerances.
Smokers, who tend to metabolize analgesics considerably faster than nonsmokers.
Men, as they require more analgesics than women (probably because of differences in the neuroendocrine mechanism of pain relief).
The procedure, for example, a multilevel spine fusion, is more painful than an appendectomy.
Anxiety, for example, patients with neurosis, suffer greater postoperative pain than those without neurosis.
Taking a history in which you gauge the patient’s anxiety level before surgery is essential. In one study, 65 patients between 12 and 18 years of age reported their anxiety and expected levels of postoperative pain before surgery. Patient-controlled anesthesia use was then
recorded through the end of the second postoperative day. Preoperative scores (anxiety and anticipated pain) predicted postoperative pain scores and number of PCA injections.5
recorded through the end of the second postoperative day. Preoperative scores (anxiety and anticipated pain) predicted postoperative pain scores and number of PCA injections.5
In the postoperative period, you need to determine the patient’s pain intensity. When possible, the visual analog pain scale from 0 to 10 should be used. The immediate postoperative examination may be limited based on the type of procedure the patient has undergone.
Effects of Postoperative Pain
It is critically important to control postoperative nociceptive pain and, when present, postoperative neuropathic pain. Uncontrolled postoperative pain can lead to many deleterious effects.
Physiologic Effects
Significant postoperative pain increases the catabolic demands of the body. This results in poor wound healing, weakness, and muscle breakdown. There is also increased sympathetic activity, leading to tachycardia and decreased intestinal motility. Patients with coronary artery disease are at higher risk because of uncontrolled sympathetic activity. Special care should be taken with these patients to prevent pain-induced tachycardia as well as hypertension, and emotional distress.
Functional Effects
Intense pain with any movement may cause an increased risk of postoperative deep vein thrombosis (DVT). Increased risk of atelectasis because of poor lung expansion secondary to pain is of particular worry in patients who have had procedures performed in the thoracic and upper abdominal regions. After surgery there is poor compliance with physical therapy with high pain levels.
Psychological Effects
Patients with high postoperative pain levels experience increased anxiety and depression. The best way to address anxiety is in the preprocedural office visit, where the practitioner can explain the questions and answers of the procedure and curb anxiety.
Chronic Pain Effects
Prolonged pain can lead to neuroplastic changes and the development of chronic pain when not properly treated during the acute postoperative period. Neuronal changes exist long after the offending stimulus has ended and the wound has healed. Chronic pain is pain lasting beyond what is typically expected based on the type of surgery. The intensity of acute postoperative pain correlates with the risk of developing a persistent pain state.2 After surgery there is functional reorganization in the dorsal horn of the spinal cord. Altered gene transcription in sensory neurons and in the spinal cord occurs hours after tissue injury (Fig. 8-2). These alterations include the reduction of inhibitory pain neurotransmitters.3,4 Further neuroplastic alteration takes place in the cortex. Maladaptive neuroplastic changes may cause a hyper-responsiveness to pain, with amplification of pain signaling. Unfortunately, if not controlled early, these neuroplastic changes can lead to chronic pain.
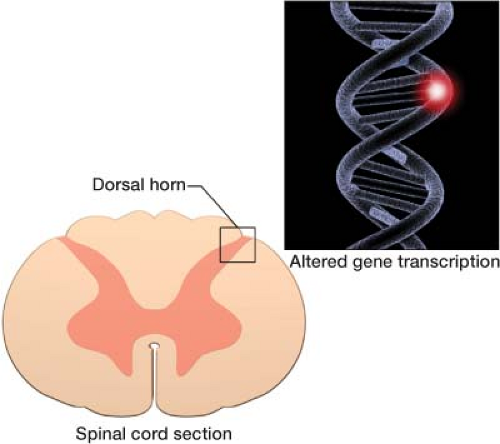 Figure 8-2 Alterations at the gene level occur in the spinal cord and brain after tissue injury from surgery.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|