Epidural Steroid Injections
Most people think of an epidural injection as what is administered to a woman for pain control before she delivers her baby. The word epidural simply refers to the epidural space. It is the outermost space in the spinal canal, lying outside the dura mater inside the surrounding vertebrae (Fig. 19-1). The superior limit of the epidural space is the foramen magnum, where the spine meets the skull. The inferior limit is the end of the sacrum. The epidural space is important because it is where the nerve roots can be accessed to provide pain relief. There are multiple approaches to this space and different medications that can be injected into it. A catheter may be placed into the epidural space to deliver continuous local anesthetic infusion, which is what the expectant mother receives. After delivery, the infusion is stopped and the catheter is taken out. This chapter addresses epidural steroid injections—injecting steroid into the epidural space to reduce inflammation and decrease pain.
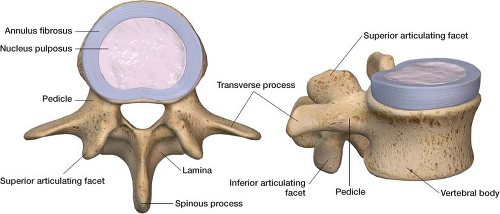
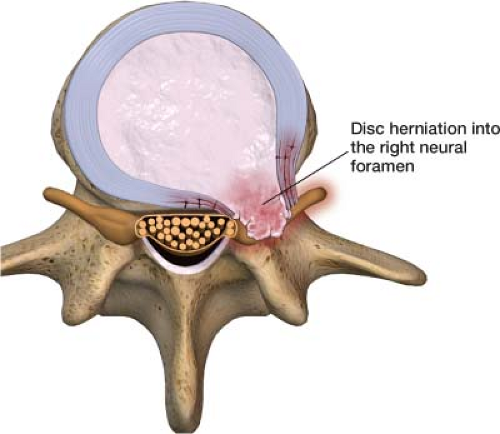
A vertebral disc is built like a jelly doughnut. The inner jelly part is the nucleus pulposus and the outer layer is the anulus fibrosus (Fig. 19-2). The anulus fibrosis can become weak, allowing the nucleus pulposus to herniate into it, and in some cases through it. This herniation of disc material out of its normal position causes compression and irritation of the adjacent nerve root (Fig. 19-3). This is referred to as radicular pain or radiculopathy (irritation of a nerve root). When a nerve root is irritated, it sends an aberrant signal up to the brain, which interprets this as pain along that entire nerve. The brain is tricked into thinking the entire nerve is affected. Furthermore the nucleus pulposus contains inflammatory factors that can leak out through the anulus fibrosus and bathe the nerve root in an inflammatory matrix. Steroids suppress the autoimmune response triggered by glycoproteins from the nucleus pulposus and exert membrane-stabilizing effects on injured nerve segments, reducing ectopic discharges from the affected nerve roots.1,3 The combination of both inflammation and physical protrusion of a disc herniation may eventually put pressure on the epidural venous plexus, causing venous obstruction.1 When the venous side is backed up, it can lead to decreased perfusion of the nerve root from the arterial side. Prolonged irritation and poor blood circulation appear to make these nerve roots hypersensitive,2 further contributing to prolonged radicular pain.
The disc that lies between the body of the fourth and fifth lumbar vertebral bodies (L4–L5) and the disc that lies between the fifth lumbar vertebral body and the sacrum (L5–S1) are where 90% of disc herniations occur in the lumbar spine. This is a matter of physics. The greatest range of motion in the spine is at the L4–L5 and L5–S1 levels, which makes these discs most vulnerable to herniation. This phenomenon can also occur in the cervical spine. Cervical discs can herniate, causing cervical radiculopathy with paresthesia (a skin sensation of tingling or prickling) radiating down the arm. The location with the greatest range of motion in the cervical spine is at the C5–C6 and C6–C7 levels.
When to use
The two most common indications for epidural steroid injections are lumbar and cervical radiculopathy. Another condition that may respond to a series of
epidural steroid injections is spinal canal stenosis. The injections alleviate pressure stemming from the inflamed tissue. Other common indications include postlaminectomy syndrome, vertebral compression fractures, sacral fractures, degenerative disc disease, and postherpetic neuralgia. In postherpetic neuralgia, an epidural steroid injection consisting of a local anesthetic and steroid mixture can help to stabilize an aberrant firing dorsal root ganglion.
epidural steroid injections is spinal canal stenosis. The injections alleviate pressure stemming from the inflamed tissue. Other common indications include postlaminectomy syndrome, vertebral compression fractures, sacral fractures, degenerative disc disease, and postherpetic neuralgia. In postherpetic neuralgia, an epidural steroid injection consisting of a local anesthetic and steroid mixture can help to stabilize an aberrant firing dorsal root ganglion.
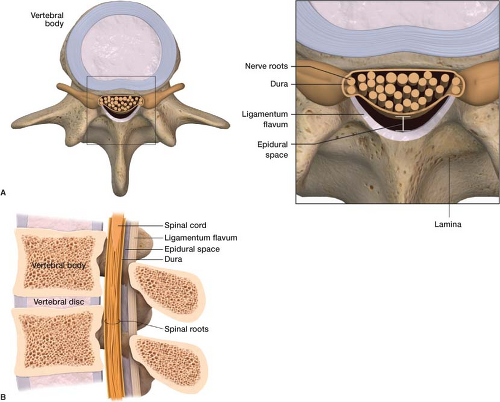 Figure 19-1 The epidural space lies outside the dura mater inside the surrounding vertebrae. A. Axial view of the epidural space. B. Sagital view of the epidural space. |
Epidural steroid injections remain a conservative traditional alternative to surgery. They can be used in combination with oral medication or as an alternative. Epidural steroid injections deliver a concentrated steroid dose directly to the level of pathology in lower quantities than would be needed via oral or intravenous administration. Theoretically, the epidural steroids are more effective within the first 3 months of radiculopathy, and may help prevent chronic fibrosis and adhesions around the nerve root.
The pain from most disc herniations resolves on its own in around a year. However, with an epidural steroid injection, the patient may not have to spend as much as a year waiting for the symptoms to dissipate. By decreasing pain levels the patient can remain active, avoiding the risk of deteriorating physical condition and missing work. An epidural steroid injection can eliminate the need for pain medications that often have to be taken every day, can have side effects, and may not be effective. For radiculopathy, trying an epidural steroid injection before prescribing narcotic medication is highly appropriate.
Table 19-1 Equivalent Doses of Other Steroids to Kenalog 40 mg | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
In the past physicians performed epidural steroid injections blindly without fluoroscopy (x-ray guidance), and this necessitated injecting a substantial amount of medication. Now that the use of fluoroscopy with epidural steroid injections are routinely used, the doses used have dropped substantially. Patients currently on average can have four injections per year (not three injections in a lifetime, a common misconception) without disrupting the pituitary adrenal axis.
As frequently as these injections are performed, there is no consensus as to what steroid to inject and how much should be injected. I use Kenalog (triamcinolone acetonide) for my injections; reasonable Kenalog doses are provided in the examples to follow. But if you decide to use Depo-Medrol, Celestone, or any other steroid, their proper dose can easily be calculated—for example, 40 mg of Kenalog is equivalent to 6 mg of Celestone (Table 19-1).
The physicians should be sure to tell the patient that steroids take time to work, pain relief may not be noted until 4–7 days post injection, and more than one injection may be necessary to achieve a compounding effect.
How to Perform the Procedure
The two most common forms of the epidural steroid injection are the interlaminar and transforaminal approaches; sometimes it is necessary to use a caudal approach.
Interlaminar Epidural Steroid Injection
It is essential that the procedure be completely explained to the patient, that all questions are answered, and that informed consent obtained.
After the patient is brought to the fluoroscopy suite, he or she should lie on the fluoroscopic table in the prone position (face down). A “time out” is performed
prior to the procedure including verbal confirmation of correct patient, procedure & procedural site. Noninvasive hemodynamic monitors and pulse oximetry are placed.
prior to the procedure including verbal confirmation of correct patient, procedure & procedural site. Noninvasive hemodynamic monitors and pulse oximetry are placed.
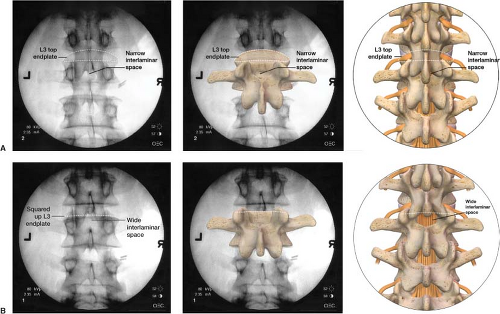
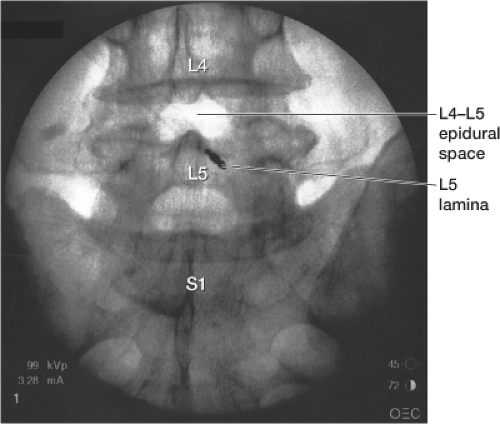
To begin, the skin over the lower back is prepped with Betadine and drapes are placed over the area in standard sterile fashion. The fluoroscope is placed in the anteroposterior (AP) position, tilting it if necessary in a cephalad to caudad motion to “square up” the end plates of the vertebral bodies (Fig. 19-4). Patients with prominent lordosis may require a significant tilt of the fluoroscope. The epidural space of interest is visualized. Using a metal marker and a felt tip marking pen, an “X” is placed on the skin overlying the inferior lamina of the epidural space of interest (Fig. 19-5).
The skin and subcutaneous tissue is anesthetized with 2% lidocaine using a 1.5-in, 25G needle. After the skin is anesthetized, a Tuohy epidural needle
(Fig. 19-6) is placed through the “X” in a perpendicular fashion to the skin and parallel to the fluoroscope (Fig. 19-7). The Tuohy needle is advanced until the lamina is contacted; the needle is then slightly retracted and advanced superiorly and medially toward the center of the epidural space. The needle then enters the ligamentum flavum, a typically thick ligament that “grabs” the needle as you enter it. At this point, the stylet of the Tuohy needle is removed and a glass syringe is attached to the Tuohy needle. I
fill the glass syringe with 3 mL of preservative free saline; some doctors use air. When the needle is in the ligamentum flavum, the saline stays in the syringe despite applying light pressure to the plunger. As the needle pushes through the ligamentum flavum the saline is sucked into the epidural space by negative pressure indicating proper position (Fig. 19-8). This is known as the loss-of-resistance technique. Once
this occurs, a 3-mL syringe with tubing containing contrast is connected to the Tuohy needle. Tubing is used so that you can see the contrast being injected under live x-ray without having your hand obscure the image while simultaneously protecting your hand from radiation exposure. Contrast is injected to make sure that there is proper spread into the epidural space (Fig. 19-9). You can also confirm proper contrast spread on a lateral view (Fig. 19-10).
(Fig. 19-6) is placed through the “X” in a perpendicular fashion to the skin and parallel to the fluoroscope (Fig. 19-7). The Tuohy needle is advanced until the lamina is contacted; the needle is then slightly retracted and advanced superiorly and medially toward the center of the epidural space. The needle then enters the ligamentum flavum, a typically thick ligament that “grabs” the needle as you enter it. At this point, the stylet of the Tuohy needle is removed and a glass syringe is attached to the Tuohy needle. I
fill the glass syringe with 3 mL of preservative free saline; some doctors use air. When the needle is in the ligamentum flavum, the saline stays in the syringe despite applying light pressure to the plunger. As the needle pushes through the ligamentum flavum the saline is sucked into the epidural space by negative pressure indicating proper position (Fig. 19-8). This is known as the loss-of-resistance technique. Once
this occurs, a 3-mL syringe with tubing containing contrast is connected to the Tuohy needle. Tubing is used so that you can see the contrast being injected under live x-ray without having your hand obscure the image while simultaneously protecting your hand from radiation exposure. Contrast is injected to make sure that there is proper spread into the epidural space (Fig. 19-9). You can also confirm proper contrast spread on a lateral view (Fig. 19-10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree