Ventricular arrhythmias
Ventricular arrhythmias originate in the ventricles below the bifurcation of the bundle of His. These arrhythmias occur when electrical impulses depolarize the myocardium using a different pathway from normal impulse conduction.
Ventricular arrhythmias appear on an ECG in characteristic ways. The QRS complex in most of these arrhythmias is wider than normal because of the prolonged conduction time through, and abnormal depolarization of, the ventricles. The deflections of the T wave and the QRS complex are in opposite directions because ventricular repolarization, as well as ventricular depolarization, is abnormal. The P wave in many ventricular arrhythmias is absent because atrial depolarization doesn’t occur. If the P wave does occur, it usually doesn’t have any relationship to the QRS complex.
When electrical impulses come from the ventricles instead of the atria, atrial kick is lost and cardiac output can decrease by as much as 30%. This decrease is one reason why patients with ventricular arrhythmias may show signs and symptoms of heart failure, including hypotension, angina, syncope, and respiratory distress.
Although ventricular arrhythmias may be benign, they’re generally considered the most serious arrhythmias because the ventricles are ultimately responsible for cardiac output. Rapid recognition and treatment of ventricular arrhythmias increases the chances of successful resuscitation. Ventricular arrhythmias include premature ventricular contractions, idioventricular rhythm, ventricular tachycardia, ventricular fibrillation, and asystole.
Life-Threatening
Premature ventricular contractions
Premature ventricular contractions (PVCs) are ectopic beats that originate in the ventricles and occur earlier than expected. PVCs may occur in healthy people without being clinically significant. When PVCs occur in patients with underlying heart disease, however, they may herald the development of lethal ventricular arrhythmias, including ventricular tachycardia (VT) and ventricular fibrillation (VF).
PVCs may occur singly, in pairs (couplets), or in clusters. PVCs may also appear in patterns, such as bigeminy or trigeminy. (See Recognizing PVCs.) In many cases, PVCs are followed by a compensatory pause. (See Compensatory pause.)
PVCs may be uniform in appearance, arising from a single ectopic ventricular pacemaker site, or multiform, originating
from different sites or originating from a single pacemaker site but having QRS complexes that differ in size, shape, and direction. PVCs may also be described as unifocal or multifocal. Unifocal PVCs originate from the same ventricular ectopic pacemaker site, whereas multifocal PVCs originate from different ectopic pacemaker sites in the ventricles.
from different sites or originating from a single pacemaker site but having QRS complexes that differ in size, shape, and direction. PVCs may also be described as unifocal or multifocal. Unifocal PVCs originate from the same ventricular ectopic pacemaker site, whereas multifocal PVCs originate from different ectopic pacemaker sites in the ventricles.
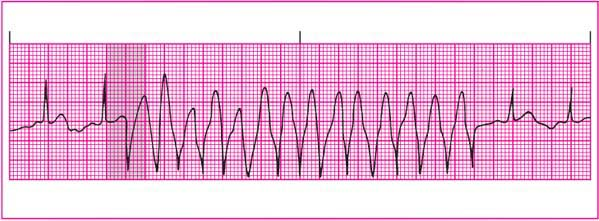
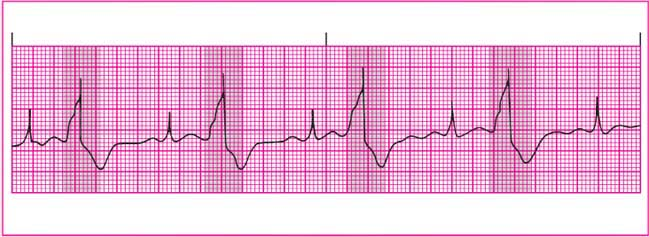
Recognizing PVCs
To help you recognize premature ventricular contraction (PVC), review this sample rhythm strip. On this strip, PVC occurs on beats 1, 6, and 11.
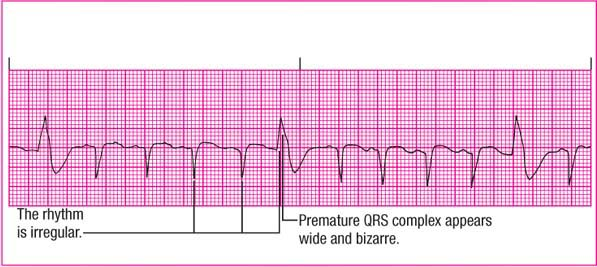 |
Rhythm: Irregular
Rate: 120 beats/minute
P wave: Absent with PVC but present with other QRS complexes
PR interval: 0.12 second in underlying rhythm
QRS complex: Early with bizarre configuration and duration of 0.14 second in PVC; 0.08 second in underlying rhythm
T wave: Normal; opposite direction from QRS complex with PVC
QT interval: 0.28 second with underlying rhythm
Other: Underlying rhythm sinus tachycardia
Compensatory pause
You can determine if a compensatory pause exists by using calipers to mark off two normal P-P intervals. Place one leg of the calipers on the sinus P wave that comes just before the PVC. If the pause is compensatory, the other leg of the calipers will fall precisely on the P wave that comes after the pause.
Causes
PVCs are usually caused by enhanced automaticity in the ventricular conduction system or muscle tissue. The irritable focus results from a disruption of the normal electrolyte shifts during cellular depolarization and repolarization. Possible causes of PVCs include:
anesthetics
electrolyte imbalances, such as hypokalemia, hyperkalemia, hypomagnesemia, and hypocalcemia
enlargement or hypertrophy of the ventricular chambers
hypoxia
increased sympathetic stimulation
infection
irritation of the ventricles by pacemaker electrodes or a pulmonary artery catheter
metabolic acidosis
mitral valve prolapse
myocardial ischemia and infarction
myocarditis
sympathomimetic drugs, such as epinephrine and isoproterenol
tobacco use
caffeine or alcohol ingestion
drug intoxication, particularly with cocaine, amphetamines, digoxin (Lanoxin), phenothiazines, and tricyclic antidepressants.
Clinical significance
PVCs are significant for two reasons. First, they can lead to more serious arrhythmias, such as VT or VF. The risk of developing a more serious arrhythmia increases in patients with ischemic or damaged hearts.
PVCs also decrease cardiac output, especially if ectopic beats are frequent or sustained. The decrease in cardiac output with a PVC stems from reduced ventricular diastolic filling time and the loss of atrial kick for that beat. The clinical impact of PVCs hinges on the body’s ability to maintain adequate perfusion and the duration of the abnormal rhythm.
To help determine the seriousness of PVCs, ask these questions:
How often do they occur? In patients with chronic PVCs, an increase in frequency or a change in the pattern of PVCs from the baseline rhythm may signal a more serious condition.
What’s the pattern of PVCs? If the ECG shows a dangerous pattern—such as paired PVCs, PVCs with more than one focus, a bigeminal rhythm, or R-on-T phenomenon (when a PVC strikes on the down slope of the preceding normal T wave)—the patient may require immediate treatment. (See Patterns of potentially dangerous PVCs.)
Are they really PVCs? Make sure the complex is a PVC, not another, less dangerous arrhythmia. PVCs may be mistaken for ventricular escape beats or normal impulses with aberrant ventricular conduction. Ventricular escape beats serve as a safety mechanism to protect the heart from ventricular standstill. Some supraventricular impulses may follow an abnormal (aberrant) conduction pathway causing an abnormal appearance to the QRS complex. In any event, never delay treatment if the patient is unstable.
ECG characteristics
Rhythm: Atrial and ventricular rhythms are irregular during PVCs; the underlying rhythm may be regular.
Rate: Atrial and ventricular rates reflect the underlying rhythm.
P wave: Usually absent in the ectopic beat, but with retrograde conduction to the atria, the P wave may appear after the QRS complex. It’s usually normal if present in the underlying rhythm.
PR interval: Not measurable except in the underlying rhythm.
QRS complex: Occurrence is earlier than expected. Duration exceeds 0.12 second, with a bizarre and wide configuration. Configuration of the QRS complex is usually normal in the underlying rhythm.
T wave: Occurrence is in opposite direction to the QRS complex. When a PVC strikes on the downslope of the preceding normal T wave—the R-on-T phenomenon—it
can trigger more serious rhythm disturbances such as ventricular fibrillation.
QT interval: Not usually measured, except in the underlying rhythm.
Other: A PVC may be followed by a compensatory pause, which can be full or incomplete. The sum of a full compensatory pause and the preceding R-R interval is equal to the sum of two R-R intervals of the underlying rhythm. If the sinoatrial (SA) node is depolarized by the PVC, the timing of the SA node is reset, and the compensatory pause is called incomplete. In this case, the sum of an incomplete compensatory pause and the preceding R-R interval is less than the sum of two R-R intervals of the underlying rhythm. A PVC occurring between two normally conducted
QRS complexes without greatly disturbing the underlying rhythm is referred to as interpolated. A full compensatory pause, usually accompanying PVCs, is absent with interpolated PVCs.
Patterns of potentially dangerous PVCs
Some premature ventricular contractions (PVCs) are more dangerous than others. Here are examples of patterns of potentially dangerous PVCs.
Paired PVCs
Two PVCs in a row, called paired PVCs or a ventricular couplet (see shaded areas), can produce ventricular tachycardia (VT). That’s because the second contraction usually meets refractory tissue. A burst, or a salvo, of three or more PVCs in a row is considered a run of VT.
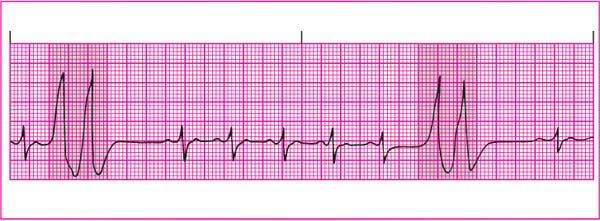 |
Multiform PVCs
Multiform PVCs, which look different from one another, arise from different sites or from the same site with abnormal conduction (see shaded areas). Multiform PVCs may indicate severe heart disease or digoxin toxicity.
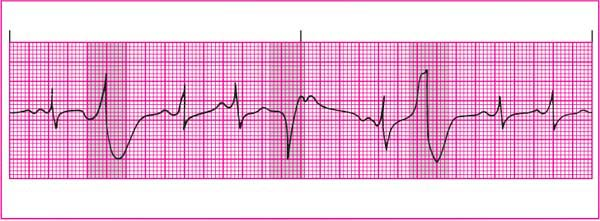 |
Bigeminy and trigeminy
PVCs that occur every other beat (bigeminy) or every third beat (trigeminy) may indicate increased ventricular irritability, which can result in VT or ventricular fibrillation (see shaded areas). The rhythm strip shown at the top of the next page illustrates ventricular bigeminy.
 |
Sometimes it’s difficult to distinguish PVCs from aberrant ventricular conduction. (See Distinguishing PVCs from ventricular aberrancy, pages 160 and 161.)
Signs and symptoms
The patient experiencing PVCs usually has a normal pulse rate with a momentarily irregular pulse rhythm when a PVC occurs.
With PVCs, the patient has a weaker pulse wave after the premature beat and a longer-than-normal pause between pulse waves. If the carotid pulse is visible, however, you may see a weaker arterial wave after the premature beat. When auscultating for heart sounds, you hear an abnormally early heart sound with each PVC.
A patient with PVCs may be asymptomatic; however, patients with frequent PVCs may complain of palpitations. The patient may also exhibit signs and symptoms of decreased cardiac output, including hypotension and syncope.
Interventions
If the PVCs are infrequent and the patient has normal heart function and is asymptomatic, the arrhythmia probably doesn’t require treatment. If symptoms or a dangerous form of PVCs occur, the type of treatment given depends on the cause of the problem.
If PVCs have a purely cardiac origin, drugs to suppress ventricular irritability, such as procainamide (Procan), amiodarone (Cordarone), or lidocaine, may be used. When PVCs have a noncardiac origin, treatment is aimed at correcting the cause. For example, drug therapy may be adjusted or the patient’s acidosis or electrolyte imbalance may be corrected.
Patients who have recently developed PVCs need prompt assessment, especially if they have underlying heart disease or complex medical problems. Patients with chronic PVCs should be closely observed for the development of more frequent PVCs or more dangerous PVC patterns.
Until effective treatment is begun, patients with PVCs accompanied by serious symptoms should have continuous ECG monitoring and ambulate only with assistance. If the patient is discharged on antiarrhythmic medications, family members should know how to contact the
emergency medical system and perform cardiopulmonary resuscitation (CPR).
emergency medical system and perform cardiopulmonary resuscitation (CPR).
Look-Alikes
Distinguishing PVCs from ventricular aberrancy
Perhaps one of the most challenging look-alikes—premature ventricular contractions (PVCs) versus ventricular aberrancy—can sometimes be distinguished with complete confidence only in the electrophysiology laboratory. Ventricular aberrancy, or aberrant ventricular conduction, occurs when an electrical impulse originating in the sinoatrial node, atria, or atrioventricular junction is temporarily conducted abnormally through the bundle branches.
The abnormal conduction results in a bundle-branch block and usually stems from the arrival of electrical impulses at the bundle branches before the branches have been sufficiently repolarized.
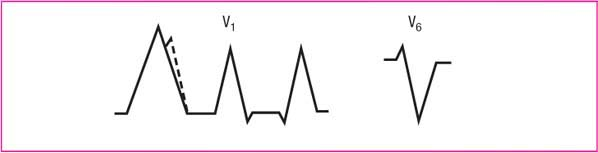
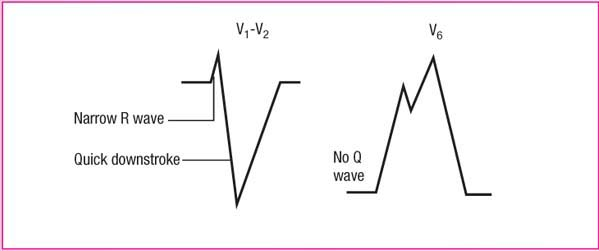
To distinguish between PVCs and ventricular aberrancy, examine the deflection of the QRS complex in lead V1. Determine whether the QRS complex is primarily positive or negative. Based on this information, follow these clues to guide your analysis.
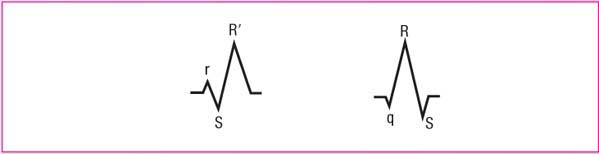
Mostly positive QRS
Right bundle-branch aberrancy has a triphasic rSR′ configuration in V1 and a triphasic qRS configuration in V6.
If there are two positive peaks in V1 and the left peak is taller, the beat is probably a PVC.
PVCs are monophasic or biphasic in V1, and biphasic in V6, with a deep S wave.
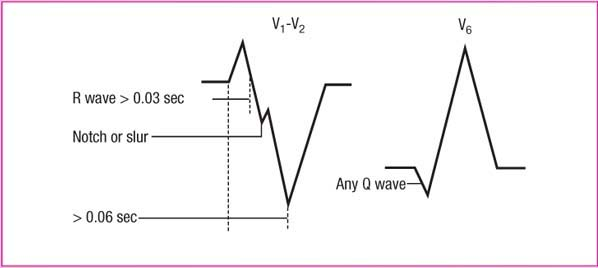
Mostly negative QRS
Left bundle-branch aberrancy has a narrow R wave with a quick downstroke in leads V1 and V2, with no Q wave in V6.
PVCs have a wide R wave (> 0.03 second) and a notched or slurred S-wave downstroke in leads V1 and V2, with a duration of > 0.06 second from the onset of the R wave to the deepest point of the S wave in V1 and V2, with a Q wave in V6.
P waves commonly precede aberrancies, but don’t generally precede PVCs.
Aberrancies usually have a QRS duration of 0.12 second. PVCs are more likely to have a QRS duration of 0.14 second or more.
Life-Threatening
Idioventricular Rhythm
Idioventricular rhythm, also referred to as ventricular escape rhythm, originates in an escape pacemaker site in the ventricles. The inherent firing rate of this ectopic pacemaker is usually 20 to 40 beats/minute. The rhythm acts as a safety mechanism by preventing ventricular standstill, or asystole—the absence of electrical activity in the ventricles. When fewer than three QRS complexes arising from the escape pacemaker occur, they’re called ventricular escape beats or complexes. (See Recognizing idioventricular rhythm.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree