Urinary Tract Infection
Tracy N. Offerdahl Pharm.D.
Elena M. Umland Pharm.D.
Urinary tract infections (UTIs) are common and may range in severity from uncomplicated cystitis to severe pyelonephritis. These infections result in millions of visits to health care providers each year and may also become an unexpected complication of a hospital admission. Both men and women experience UTIs, but the incidence in females far exceeds that of males until the age of 50. UTIs may also become complications of pregnancy, paralysis, diabetes mellitus, renal transplantation, and many renal diseases (Kunin, 1994a; (Young & Koda-Kimble, 1995).
UTIs may be classified according to where the infection occurs or by the frequency of infection. For instance, cystitis or urethritis are both considered lower tract infections because they usually involve the bladder and urethra. In contrast, pyelonephritis is considered an upper tract infection because it involves inflammation of the renal parenchyma. Patients may also experience an acute UTI, or they may experience chronic exacerbations of infection from either relapse or reinfection (Young & Koda-Kimble, 1995; DiPiro et al, 1997; Perdue & Plaisance, 1995).
UTIs can further be classified as uncomplicated or complicated—no structural or neurologic abnormalities versus a predisposing lesion of the urinary tract. Other patient factors that may be associated with a complicated UTI include pregnancy, diabetes mellitus, and immunosuppression (Young & Koda-Kimble, 1995; DiPiro et al, 1997; Perdue & Plaisance, 1995).
Additionally, patients may present with nephrolithiasis (kidney stones) of infectious origin. Patients may have symptoms of a UTI, such as bacteriuria or dysuria, without actually having a UTI (Young & Koda-Kimble, 1995; DiPiro et al, 1997; Perdue & Plaisance, 1995).
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
Bacteria enter and spread throughout the urinary tract in three ways: the ascending route, the hematogeneous route, and the lymphatic route. The ascending route is the most common (Young & Koda-Kimble, 1995; Stamm & Hooton, 1993; Hatton et al, 1994; Mandell et al, 1995).
In comparing the female and male anatomies, the urethra in the female is shorter and in close proximity to the rectal area, making it an easy target for fecal contamination. Once bacteria have colonized the urethral area, they multiply, leading to retrograde infection of the bladder (Young & Koda-Kimble, 1995; Stamm & Hooton, 1993; Hatton et al, 1994; Mandell et al, 1995).
Although both urine elements and bladder mucosal elements have protective properties against infection, certain risk factors may predispose patients to infection. These will be discussed later in the chapter. Bacteria can further move to involve the bladder (upper tract infection), especially in patients with decreased urethral peristalsis, such as in pregnancy, urethral obstruction, urethral massage, self-catheterization, diaphragm use, or virulent gram-negative bacterial infections (Young & Koda-Kimble, 1995; Stamm & Hooton, 1993; Hatton et al, 1994; Mandell et al, 1995).
The hematogenous route of bacterial entry involves bloodborne pathogens that infect the renal parenchyma. The lymphatic route has been examined in animals, where a lymphatic connection was found between the ureters and the kidneys. This, however, seems to be a relatively unimportant route of infection in humans (Young & Koda-Kimble, 1995; Stamm & Hooton, 1993; Hatton et al, 1994; Mandell et al, 1995).
Nephrolithiasis
In addition to UTI development, other disorders of the urinary tract exist. One of these disorders is renal stone disease, or nephrolithiasis. The pathophysiology of nephrolithiasis is multifaceted. Renal stones may contain calcium, uric acid, struvite, cystine, and other substances, but calcium-containing stones account for a large number of recovered renal stones in cases of noninfectious nephrolithiasis (Mandell et al, 1995).
For a renal stone to develop, three requirements have been identified: the formation of a nidus, retainment of the nidus within the urinary tract, and growth of the nidus. Risk factors that contribute to stone formation are many. Hypercalciuria is a common finding in stone formers. Idiopathically it has been found to occur in 40% to 60% of these patients (Mandell et al, 1995). Other contributing factors to the formation of renal stones include dietary factors, level of patient activity, primary hyperparathyroidism, renal tubular acidosis, and hyperoxaluria (Mandell et al, 1995).
Pathology
Patients with structural abnormalities (eg, vesicoureteral reflux, neurogenic bladder, neoplasm, stricture) may experience complicated UTIs from less virulent strains of bacteria. Patients who are wheelchair-bound because of paralysis often experience these problems. These patients are categorized as having complicated UTIs, regardless of the location of the infection (Mandell et al, 1995; Lipsky, 1989; Kunin, 1994b).
EPIDEMIOLOGY
UTIs: Acute, Chronic, Pyelonephritis
UTIs are among the most frequently observed infections in clinical medicine. Primary complaints of painful urination, frequency, and urgency or actual UTI account for an estimated 6.2 million annual health care visits in the United States (Mandell et al, 1995). In more than 95% of these infections, a single bacterial species was responsible (Kunin, 1994b).
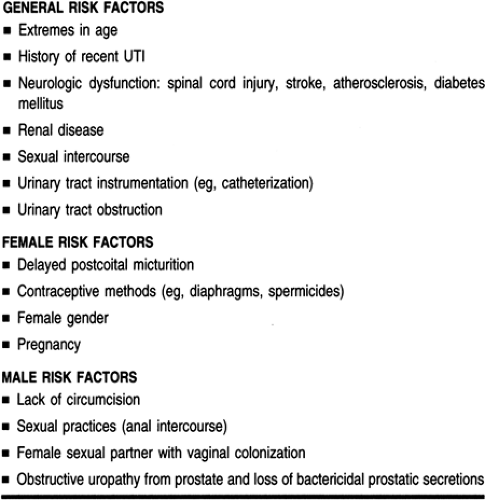
UTIs occur in both men and women at any age, independent of race. However, the risk of acquiring a UTI (Table 35-1) and the subsequent actual incidence varies according to age and gender. Between the ages of 1 and 50 years, UTIs predominantly affect females. Women in young adulthood are 30 times more likely to develop a UTI compared to males in this age group (Stamm & Hooton, 1993; Kunin, 1994b). It is estimated that 10% to 20% of the female population will experience a symptomatic UTI in their lifetime (Kunin, 1994a; Kunin, 1994b; Lemcke et al, 1995). Additionally, about half of school-aged girls found to have significant bacteriuria will develop symptomatic infection about the time they become sexually active (Perdue & Plaisance, 1995).
Gender Factors
FEMALE GENDER
Women, particularly those of childbearing age, experience UTIs at a much higher rate than do their male counterparts. About 20% of young women with an initial episode will have recurrent infections. Greater than 90% of these will be reinfections, occurring months apart. Recurrence has been associated with diaphragm use and the use of spermicides, because spermicides induce Escherichia coli colonization of the vagina (DiPiro et al, 1997). Generally, frequency of sexual intercourse, diaphragm use, and lack of urination after intercourse are risk factors for UTIs in women (Kunin, 1994b).
Pregnancy is an independent risk factor for UTI. Bacteriuria occurs in 4% to 10% of pregnant women, double the incidence in nonpregnant women of similar age. Hormones and anatomic changes have been suggested as causes (Kunin, 1994a).
Twenty-five to 30% of postpartum women have bacteriuria (Stamm & Hooton, 1993; Hatton et al, 1994). After age 65 years, approximately 20% of women have bacteriuria. Women older than 80 years of age have a 20% to 50% incidence of bacteriuria (Stamm & Hooton, 1993; Hatton et al, 1994; Warren, 1992). This incidence is highest in nursing-home residents, women with incomplete bladder emptying, those with fecal incontinence, and those requiring intermittent bladder catheterization. Postmenopausal estrogen deficiency has been implicated in contributing to increased vaginal pH, thus altering the vaginal flora and possibly contributing to bacteriuria and increased UTI occurrence in this population (Stamm & Hooton, 1993; Warren, 1992).
MALE GENDER
In general, uncomplicated UTI is rare in school-aged boys and men 20 to 50 years of age. However, by age 65 the incidence of UTI in men is comparable to that observed in women. Potential causes for this increased incidence in older men include obstructive uropathy from the prostate, fecal incontinence, and increased instrumentation and bladder catheter usage (Kunin, 1994b).
In older men, the presence of benign prostatic hypertrophy can greatly increase the incidence of UTIs. This may occur because of urethral obstruction from the size of the prostate, as well as a decrease in the bactericidal activity of the prostatic secretions. The major concern here is that bacteria may infect the prostate gland, causing bacterial prostatitis (Hatton et al, 1994; Mandell et al, 1995; Lipsky, 1989).
UTI is rare in men younger than 50 years of age, and if present it may be considered indicative of an underlying abnormality of the urologic system. In other cases, risk factors play some role. These factors include anal intercourse without a condom, in which exposure to E. coli has been noted; lack of circumcision, associated with enhanced E. coli colonization of the glans and prepuce; and sex with a partner who is vaginally colonized with uropathogens (DiPiro et al, 1997; Lipsky, 1989).
Nephrolithiasis
Nephrolithiasis affects approximately 12% of the population. It has an annual incidence in the United States of 1.6 per 1000 population (Mandell et al, 1995).
DIAGNOSTIC CRITERIA
Diagnosis of a UTI is based on patient signs and symptoms as well as laboratory testing. Another important point to consider is whether this is a first UTI or a recurrent UTI, because females with recurrent UTIs may need to be evaluated for interstitial cystitis. Symptomatic female patients with lower tract infection may complain of the following (Young & Koda-Kimble, 1995; Stamm & Hooton, 1993):
Abrupt or gradual onset of dysuria
Increased frequency of urination
Urgency of urination
Difficulty in urinating
Suprapubic or lower back pain.
Signs and symptoms of an upper tract infection may include any of the above and also the following (Young & Koda-Kimble, 1995; Stamm & Hooton, 1993):
Fever
Chills
Nausea or vomiting
Headache
Malaise
Hematuria
Flank pain.
Differentiating between a lower tract infection and an upper tract infection may be difficult, however, based on symptoms alone. Some patients with upper tract infections fail to present with the typical upper tract symptoms. Therefore, a urinalysis is important to identify any other components of infection (Young & Koda-Kimble, 1995; Stamm & Hooton, 1993).
Men with acute or chronic prostatitis may experience a variety of signs and symptoms, but many men with chronic prostatitis are totally asymptomatic. Symptoms may be similar to the typical ones experienced by patients with acute cystitis (eg, frequency of urination, difficulty on urination, and painful urination). Other signs and symptoms may include the following (Stamm & Hooton, 1993; Hatton et al, 1994; Mandell et al, 1995; Lipsky, 1989):
Fever
Chills
Perineal pain
Tender or swollen prostate gland that is warm to the touch on exam.
Nephrolithiasis
Although renal stones may form in patients of any age, the highest incidence is in patients between the ages of 20 and 40. Idiopathic hypercalciuria is the primary cause in most cases. In the elderly, primary hyperparathyroidism and drug-induced etiologies should be considered (Mandell et al, 1995).
Microbiology
In the large majority of uncomplicated cases, a single bacterial species is responsible for causing a UTI. E. coli is by far the most common pathogen isolated in acute cases of uncomplicated cystitis. Urine samples that contain multiple organisms are seen in patients with complicated UTIs or in contaminated specimens. Organisms that may indicate a contaminated specimen include Staphylococcus epidermidis, diphtheroids, lactobacilli, and anaerobes. These are normally found on the skin and urethra. Additional organisms frequently found to cause UTIs include other enteric (found in the gastrointestinal tract) gram-negative organisms such as Klebsiella spp., Proteus spp., Enterobacter spp., Staphylococcus spp., and Enterococcus spp. These organisms, along with Pseudomonas spp. and Acinetobacter spp., are more likely to be a problem in patients with recurrent or complicated UTIs, as well as in hospitalized patients. Hospitalized patients experience infection more frequently with resistant strains of these organisms (Young & Koda-Kimble, 1995; Stamm & Hooton, 1993; Hatton et al, 1994; Mandell et al, 1995).
Men with acute or chronic prostatitis may be infected with a variety of organisms, including E. coli, Pseudomonas spp., Enterococcus spp., Klebsiella spp., Enterobacter spp., and Proteus spp. (Hatton et al, 1994; Mandell et al, 1995; Lipsky, 1989).
Patients with indwelling genitourinary catheters or those receiving antimicrobial therapy may also experience UTIs caused by fungi such as Candida spp. Organisms such as Chlamydia trachomatis, Neisseria gonorrhoeae, and herpes simplex virus have been isolated in cases of sexually transmitted urethritis. These infections should be ruled out, especially in sexually active patients (Young & Koda-Kimble, 1995; Stamm & Hooton, 1993; Hatton et al, 1994; Mandell et al, 1995).
Patients with infection-induced stones, or nephrolithiasis, usually have struvite stones, which form in the presence of urease-producing bacteria that cause alkaline urine (pH ≥ 7). Many bacteria are capable of producing urease enzyme; examples include Proteus spp. and Ureaplasma urealyticum (Young & Koda-Kimble, 1995; DiPiro et al, 1997; Mandell et al, 1995) (see Table 35-1).
HISTORY AND PHYSICAL EXAM
Specific signs and symptoms are mentioned above.
DIAGNOSTIC STUDIES
Urinalysis is performed in virtually all patients suspected of having a UTI or prostatitis. It can give a quick laboratory diagnosis of infection. The midstream clean-catch method of urine collection is one of three acceptable methods of urine collection for analysis. It is the most common method for routine exam. Once the urethral area has been cleaned appropriately, patients are instructed to void and discard a small amount of urine. The rest of the midstream urine is then collected for analysis (Young & Koda-Kimble, 1995; DiPiro et al, 1997; Stamm & Hooton, 1993; Hatton et al, 1994). The two other methods of urine collection are catheterization and suprapubic aspiration, and these will be discussed later in the chapter. Regardless of the method of collection, problems with sterility and contamination of urine specimens may affect the results of the urinalysis. These problems are mainly caused by poor or inconsistent collection methods or failure to take the specimen to the laboratory immediately (or failure to refrigerate the specimen). Therefore, bacteriuria alone is not diagnostic of a UTI (Young & Koda-Kimble, 1995; DiPiro et al, 1997; Stamm & Hooton, 1993; Hatton et al, 1994).
The urinalysis includes both macroscopic and microscopic evaluation of the urine specimen. The macroscopic analysis is done by the dipstick method and consists of measuring or analyzing the urine color, specific gravity, pH, glucose, protein, ketone, blood, and bilirubin. Often the macroscopic evaluation and the dipstick portion of the urinalysis are the only parts evaluated in the laboratory. Another quick but indirect method to detect the presence of bacteria in the urine is the nitrite test: bacteria in the urine break down urinary nitrate into nitrite, resulting in a positive test (Young & Koda-Kimble, 1995; DiPiro et al, 1997; Stamm & Hooton, 1993; Hatton et al, 1994; Kunin, 1994b).
Microscopic examination is performed on the urine sample once it has been centrifuged; the sediment is then examined under a microscope. The presence and the quantity of white blood cells, or leukocytes (pyuria), erythrocytes, and bacteria is determined. Also examined in the microscopic analysis of urine is the presence of epithelial cells, crystals, and casts. The presence of white blood cell casts on the microscopic exam may be an indication of upper tract involvement; however, the absence of such casts does not rule out upper tract involvement. Table 35-2 lists normal and abnormal levels for these components of the urinalysis (Young & Koda-Kimble, 1995; DiPiro et al, 1997; Stamm & Hooton, 1993; Hatton et al, 1994; Kunin, 1994b; Traub, 1992).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree