FIGURE 26-1. Early application of Doppler ultrasound by LaGrange to perform supraclavicular brachial block.
In 1989, P. Ting and V. Sivagnanaratnam reported the use of B-mode ultrasonography to demonstrate the anatomy of the axilla and to observe the spread of local anesthetics during axillary brachial plexus block. In 1994, Stephan Kapral and colleagues systematically explored brachial plexus with B-mode ultrasound. Since that time, multiple teams worldwide have worked tirelessly on defining and improving the application of ultrasound imaging in regional anesthesia. Ultrasound-guided nerve blockade is currently used routinely in the practice of regional anesthesia in many centers worldwide.
Here is a summary of ultrasound quick facts:
• 1880: Pierre and Jacques Curie discovered the piezoelectric effect in crystals.
• 1915: Ultrasound was used by the navy for detecting submarines.
• 1920s: Paul Langevin discovers that high-power ultrasound can generate heat in osseous tissues and disrupt animal tissues.
• 1942: Karl and Dussik described ultrasound use as a diagnostic tool.
• 1950s: Ultrasound was used to treat patients with Ménière disease, Parkinson disease, and rheumatic arthritis.
• 1978: P. La Grange published the first case-series of ultrasound application for placement of needles for nerve blocks.
• 1989: P. Ting and V. Sivagnanaratnam used ultrasonography to demonstrate the anatomy of the axilla and to observe the spread of local anesthetics during axillary block.
• 1994: Steven Kapral and colleagues explored brachial plexus blockade using B-mode ultrasound.
Definition of Ultrasound
Sound travels as a mechanical longitudinal wave in which back-and-forth particle motion is parallel to the direction of wave travel. Ultrasound is high-frequency sound and refers to mechanical vibrations above 20 kHz. Human ears can hear sounds with frequencies between 20 Hz and 20 kHz. Elephants can generate and detect the sound with frequencies <20 Hz for long-distance communication; bats and dolphins produce sounds in the range of 20 to 100 kHz for precise navigation (Figure 26-2A and B). Ultrasound frequencies commonly used for medical diagnosis are between 2 MHz and 15 MHz. However, sounds with frequencies above 100 kHz do not occur naturally; only human-developed devices can both generate and detect these frequencies, or ultrasounds.
FIGURE 26-2. (A) Elephants can generate and detect the sound of frequencies <20 Hz for long-distance communication. (B) Bats and dolphins produce sounds in the range of 20–100 kHz for navigation and spatial orientation.
Piezoelectric Effect
The piezoelectric effect is a phenomenon exhibited by the generation of an electric charge in response to a mechanical force (squeeze or stretch) applied on certain materials. Conversely, mechanical deformation can be produced when an electric field is applied to such material, also known the piezoelectric effect (Figure 26-3). Both natural and human-made materials, including quartz crystals and ceramic materials, can demonstrate piezoelectric properties. Recently, lead zirconate titanate has been used as piezoelectric material for medical imaging. Lead-free piezoelectric materials are also under development. Individual piezoelectric materials produce a small amount of energy. However, by stacking piezoelectric elements into layers in a transducer, the transducer can convert electric energy into mechanical oscillations more efficiently. These mechanical oscillations are then converted into electric energy.
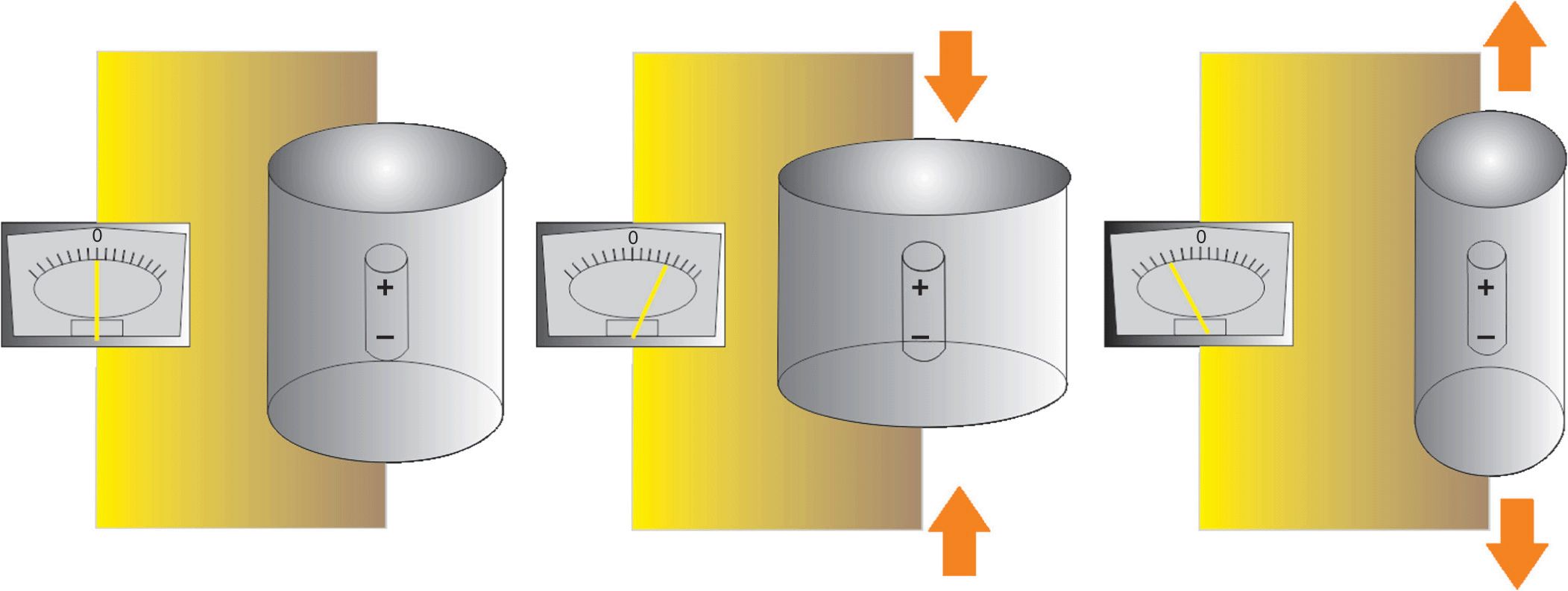
FIGURE 26-3. The piezoelectric effect. Mechanical deformation and consequent oscillation caused by an electrical field applied to certain material can produce a sound of high frequency.
Ultrasound Terminology
Period is the time it takes for one cycle to occur; the period unit of measure is the microsecond (μs).
Wavelength is the length of space over which one cycle occurs; it is equal to the travel distance from the beginning to the end of one cycle.
Acoustic velocity is the speed at which a sound wave travels through a medium. It is equal to the frequency times the wavelength. Speed is determined by the density (ρ) and stiffness (κ) of the medium (c = (κ/ρ)1/2). Density is the concentration of medium. Stiffness is the resistance of a material to compression. Propagation speed increases if the stiffness is increased or the density is decreased. The average propagation speed in soft tissues is 1540 m/s (ranges from 1400 m/s to 1640 m/s). However, ultrasound cannot penetrate lung or bone tissues.
Acoustic impedance(z) is the degree of difficulty demonstrated by a sound wave being transmitted through a medium; it is equal to density ρ multiplied by acoustic velocity c (z = ρc). It increases if the propagation speed or the density of the medium is increased.
Attenuation coefficient is the parameter used to estimate the decrement of ultrasound amplitude in a certain medium as a function of ultrasound frequency. The attenuation coefficient increases with increasing frequency; therefore, a practical consequence of attenuation is that the penetration decreases as frequency increases (Figure 26-4).
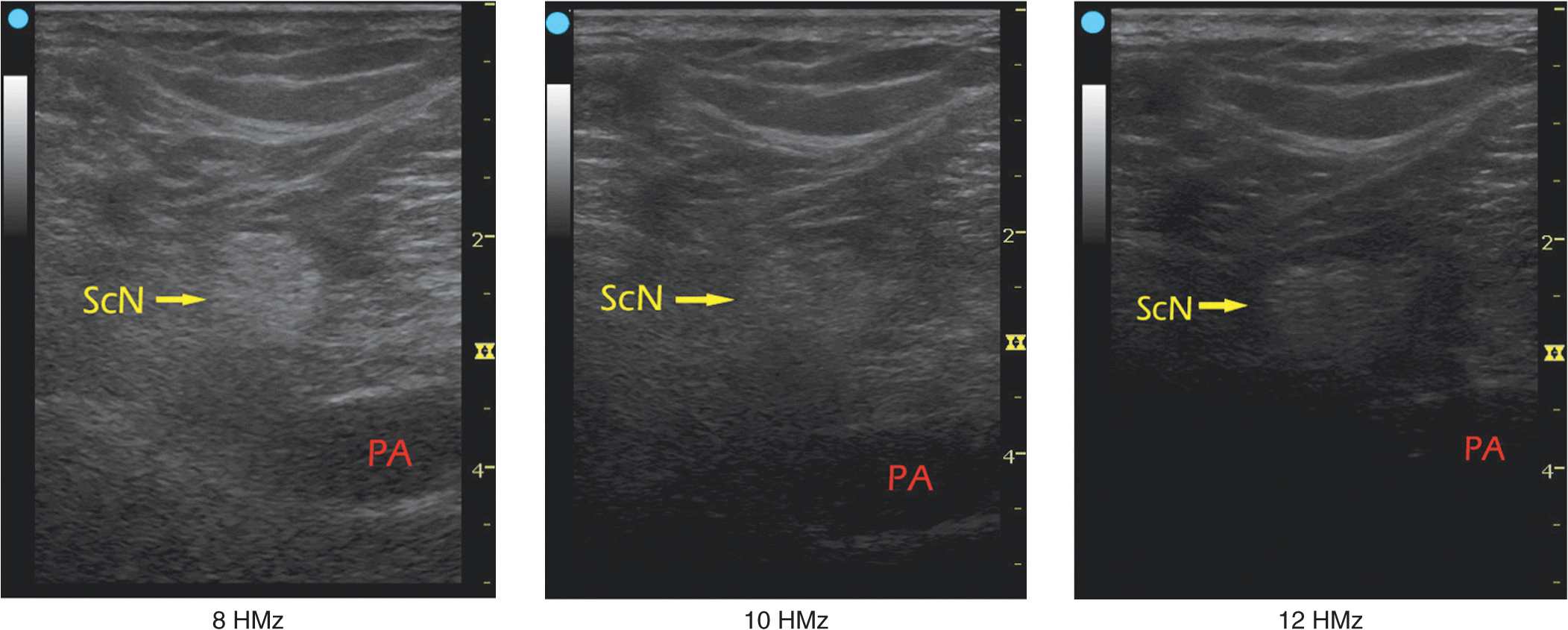
FIGURE 26-4. The ultrasound amplitude decreases in certain media as a function of ultrasound frequency, a phenomenon known as attenuation coefficient. ScN-Sciatic nerve, PA – Popliteal artery.
Ultrasound waves have a self-focusing effect, which refers to the natural narrowing of the ultrasound beam at a certain travel distance in the ultrasonic field. It is a transition level between near field and far field. The beam width at the transition level is equal to half the diameter of the transducer. At the distance of two times the near-field length, the beam width reaches the transducer diameter. The self-focusing effect amplifies ultrasound signals by increasing acoustic pressure.
In ultrasound imaging, there are two aspects of spatial resolution: axial and lateral. Axial resolution is the minimum separation of above-below planes along the beam axis. It is determined by spatial pulse length, which is equal to the product of wavelength and the number of cycles within a pulse. It can be presented in the following formula:
Axial resolution = wavelength (λ) × number of cycle per pulse = wavelength number of cycle per pulse ![]()
The number of cycles within a pulse is determined by the damping characteristics of the transducer. The number of cycles within a pulse is usually set between 2 and 4 by the manufacturer of the ultrasound machines. As an example, if a 2-MHz ultrasound transducer is theoretically used to do the scanning, the axial resolution would be between 0.8 and 1.6 mm, making it impossible to visualize a 21-G needle. For a constant acoustic velocity, higher frequency ultrasound can detect smaller objects and provide a better resolution image. Figure 26-5 shows the images at different resolutions when a 0.5-mm-diameter object is visualized with three different frequency settings. Lateral resolution is another parameter of sharpness to describe the minimum side-by-side distance between two objects. It is determined by both ultrasound frequency and beam width. Lateral resolution can be improved by focusing to reduce the beam width.
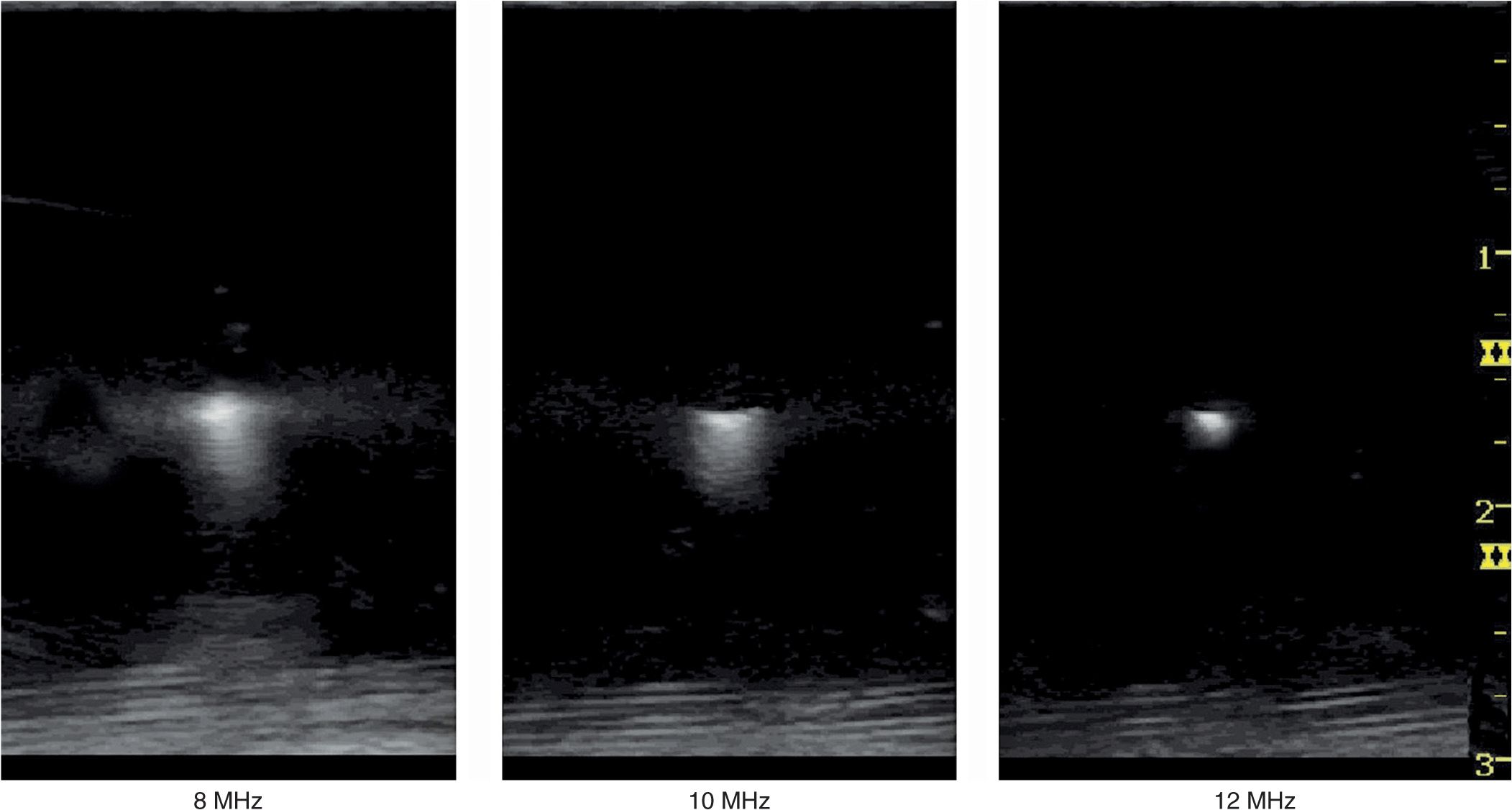
FIGURE 26-5. Ultrasound frequency affects the resolution of the imaged object. Resolution can be improved by increasing frequency and reducing the beam width by focusing.
Temporal resolution is also important to observe moving objects, such as blood vessels and the heart. Similar to a movie or cartoon video, the human eye requires that the image be updated at a rate of approximately 25 times a second or higher for an ultrasound image to appear continuous. However, imaging resolution is compromised by increasing the frame rate. Optimizing the ratio of resolution to frame rate is essential to provide the best possible image.
Interactions of Ultrasound Waves with Tissue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








