Intercostal Block

FIGURE 24-1. Intercostal nerve block: Patient position and needle insertion.
General Considerations
Intercostal block produces discrete bandlike segmental anesthesia in the chosen levels. Intercostal block is an excellent analgesic option for a variety of acute and chronic pain conditions. The beneficial effect of intercostal blockade on respiratory function following thoracic or upper abdominal surgery, or following chest wall trauma, is well documented. Although similar in many ways to the paravertebral block, intercostal blocks are generally simpler to perform because the osseous landmarks are more readily palpable. However, the risks of pneumothorax and local anesthetic systemic toxicity are present, and care must be taken to prevent these potentially serious complications. Intercostal blocks can be more challenging to perform above the level of T7 because the scapula prevents access to the ribs. Although an intercostal block is an excellent choice for analgesic purposes, it is often inadequate as a complete surgical anesthesia. For this application, supplementation with another anesthesia technique usually is required.
Regional Anesthesia Anatomy
After emerging from their respective intervertebral foramina, the thoracic nerve roots divide into dorsal and ventral rami (Figure 24-2). The dorsal ramus provides innervation to the skin and muscle of the paravertebral region; the ventral ramus continues laterally as the intercostal nerve. This nerve then pierces the posterior intercostal membrane approximately 3 cm lateral to the intervertebral foramen and enters the subcostal groove of the rib, where it travels inferiorly to the intercostal artery and vein. Initially, the nerve lies between the parietal pleura and the inner most intercostal muscle. Immediately proximal to the angle of the rib, it passes into the space between the innermost and internal intercostal muscles, where it remains for much of the remainder of its course. At the midaxillary line, the intercostal nerve gives rise to the lateral cutaneous branch, which pierces the internal and external intercostal muscles and supplies the muscles and skin of the lateral trunk. The continuation of the intercostal nerve terminates as the anterior cutaneous branch, which supplies the skin and muscles of the anterior trunk, including the skin overlying the sternum and rectus abdominis.
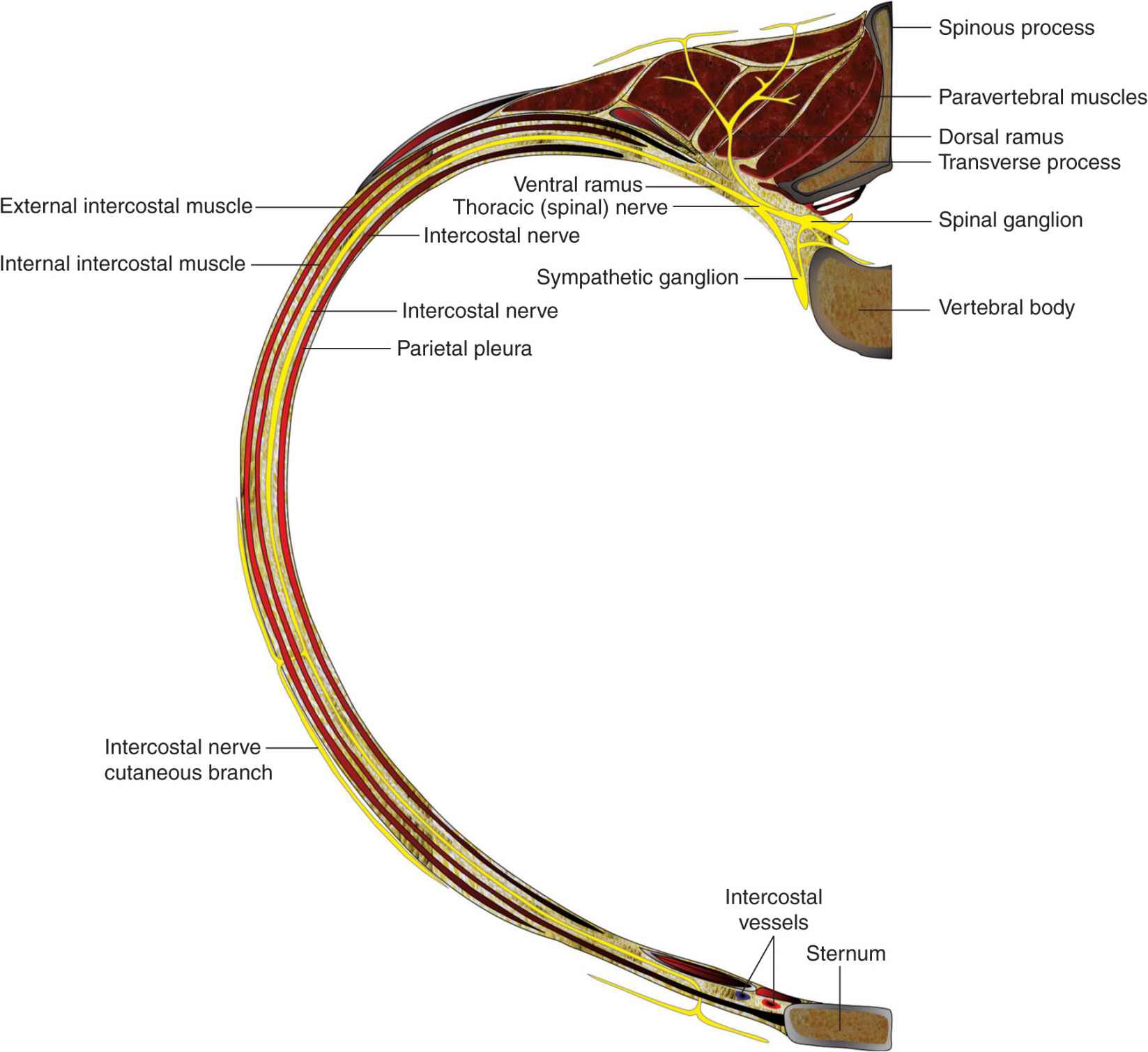
FIGURE 24-2. Anatomy of the thoracic spinal and intercostal nerves.
Distribution of Anesthesia
Intercostal blockade results in the spread of local anesthetic along the intercostals sulcus underneath the parietal pleura, leading to ipsilateral anesthesia of the blocked intercostals levels (Figure 24-3). A larger volume of local anesthetic or more medial injection may result in backtracking of local anesthetic into the paravertebral space. The extent of the resulting dermatomal distribution of anesthesia or analgesia is simply a function of the level of blockade. In contrast to paravertebral blockade, longitudinal (cephalad-caudad) spread between adjacent levels is much less common, although possible with large volumes of injectate and/or injection sites close to the midline of the back. In such instances, the local anesthetic can spread between the levels via the overflow into the paravertebral space.

FIGURE 24-3. Injection of the local anesthetic (red dye) in intercostal space results in a medial-lateral spread of the local anesthetic in the intercostal space where the intercostal nerves (arrow) are contained.
Equipment
A standard regional anesthesia tray is prepared with the following equipment:
• Sterile towels and gauze packs
• 20-mL syringes containing local anesthetic
• Sterile gloves and marking pen
• A 10-mL syringe plus 25-gauge needle with local anesthetic for skin infiltration
• A 1.5-in, 22-gauge needle attached to extension tubing
Patient Positioning
An intercostal block can be performed with the patient in the sitting, lateral decubitus, or prone positions. With the patient in sitting or lateral position, it is helpful to have the patient’s spine arched with the arms extended forward. Patients who are prone are best positioned for the block by placing a pillow under the abdomen and with the arms hanging down from the sides of the bed (Figure 24-4). This rotates the scapulae laterally and permits access to the angles of the rib above the level of T7 (Figure 24-5).

FIGURE 24-4. The patient position for intercostal block. A pillow is used as an abdominal/pelvic support. The arms are hanging off the table.
FIGURE 24-5. Technique of palpating the intercostal space. The fingers of the palpating hand are firmly pressed in the intercostal space 5–7 cm lateral to the midline.
Landmarks and Maneuvers to Accentuate Them
The following anatomic landmarks are used to estimate the position of the relevant ribs.
1. Twelfth rib (last rib palpable inferiorly) (Figure 24-6)

FIGURE 24-6. Landmarks for intercostal space are identified first by determining the midline and the spinous processes (skin marks). Intercostal space is then determined by palpation at each level to be blocked, and the insertion point for needle is marked 5–7 cm lateral to the midline.
2. The 7th rib (lowest rib covered by the angle of the scapula) (Figure 24-7)
FIGURE 24-7. Estimating T7 level at the tip of the scapula.
Once identified by palpation, the inferior border of the corresponding ribs can be marked on the skin (Figure 24-8). An “x” at the angle of the rib identifies the site of needle insertion, usually about 6–8 cm from the midline. For thoracotomy or upper abdominal incisions, an estimate of the levels required for effective analgesia can be made after discussion with the surgeon as to the planned approach and length of incision. Analgesic blocks for rib fractures are planned based on the area of the injury. Typically, in addition to the estimated dermatomal levels, one additional level above and one below the estimated levels are also blocked.

FIGURE 24-8. The needle insertion site for intercostal space is labeled 5–7 cm lateral to the midline.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








