Ultrasound-Guided Supraclavicular Brachial Plexus Block
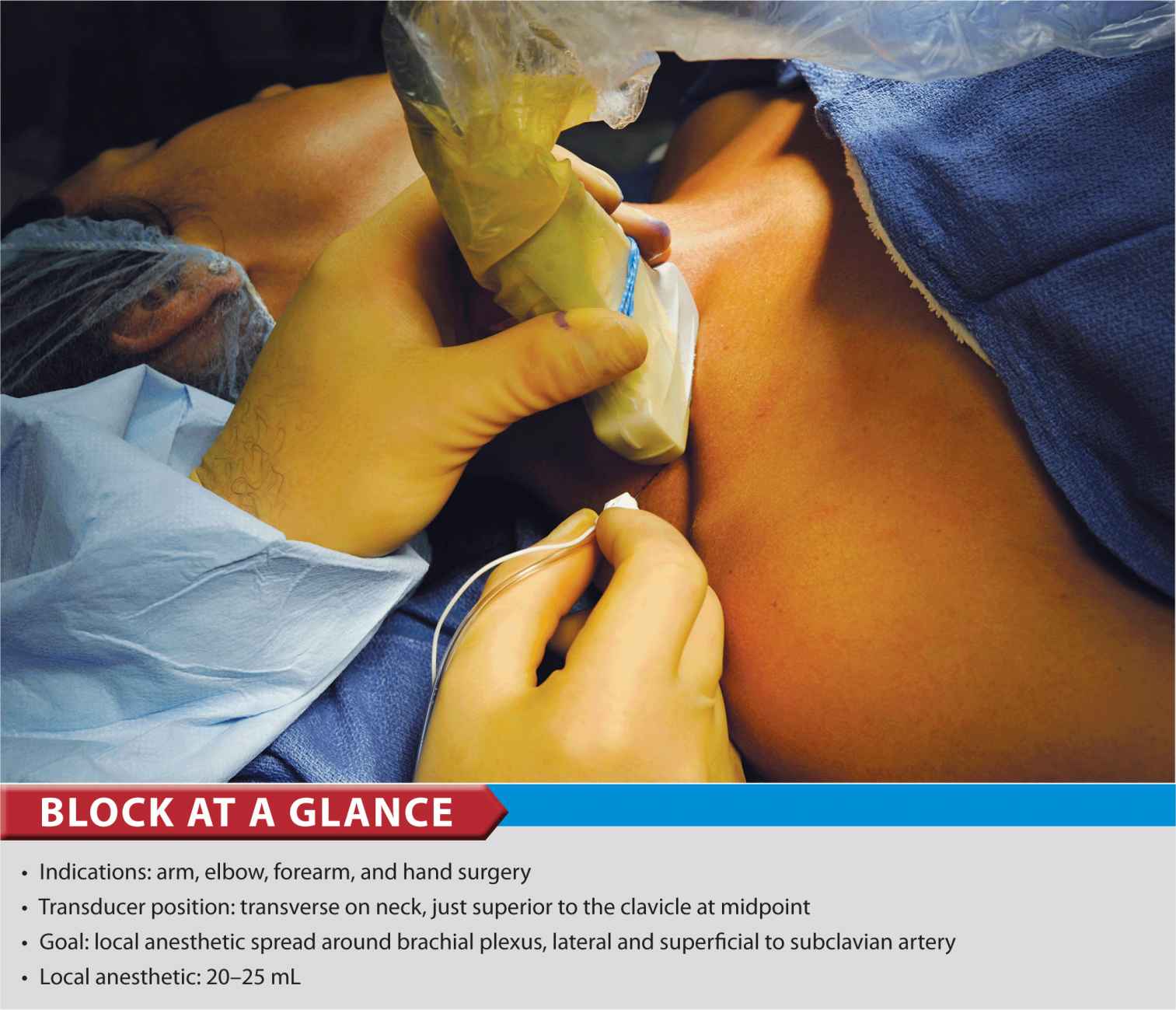
FIGURE 30-1. Supraclavicular brachial plexus; transducer position and needle insertion.
General Considerations
The proximity of the brachial plexus at this location to the chest cavity and pleura, has been of concern to many practitioners (Figure 30-2). However, ultrasound guidance has resulted in a resurgence of interest in the supraclavicular approach to the brachial plexus. The ability to image the plexus, rib, pleura, and subclavian artery with ultrasound guidance has increased safety due to better monitoring of anatomy and needle placement. Because the trunks and divisions of the brachial plexus are relatively close as they travel over the first rib, the onset and quality of anesthesia is fast and complete. For these reasons, the supraclavicular block has become a popular technique for surgery below the shoulder.
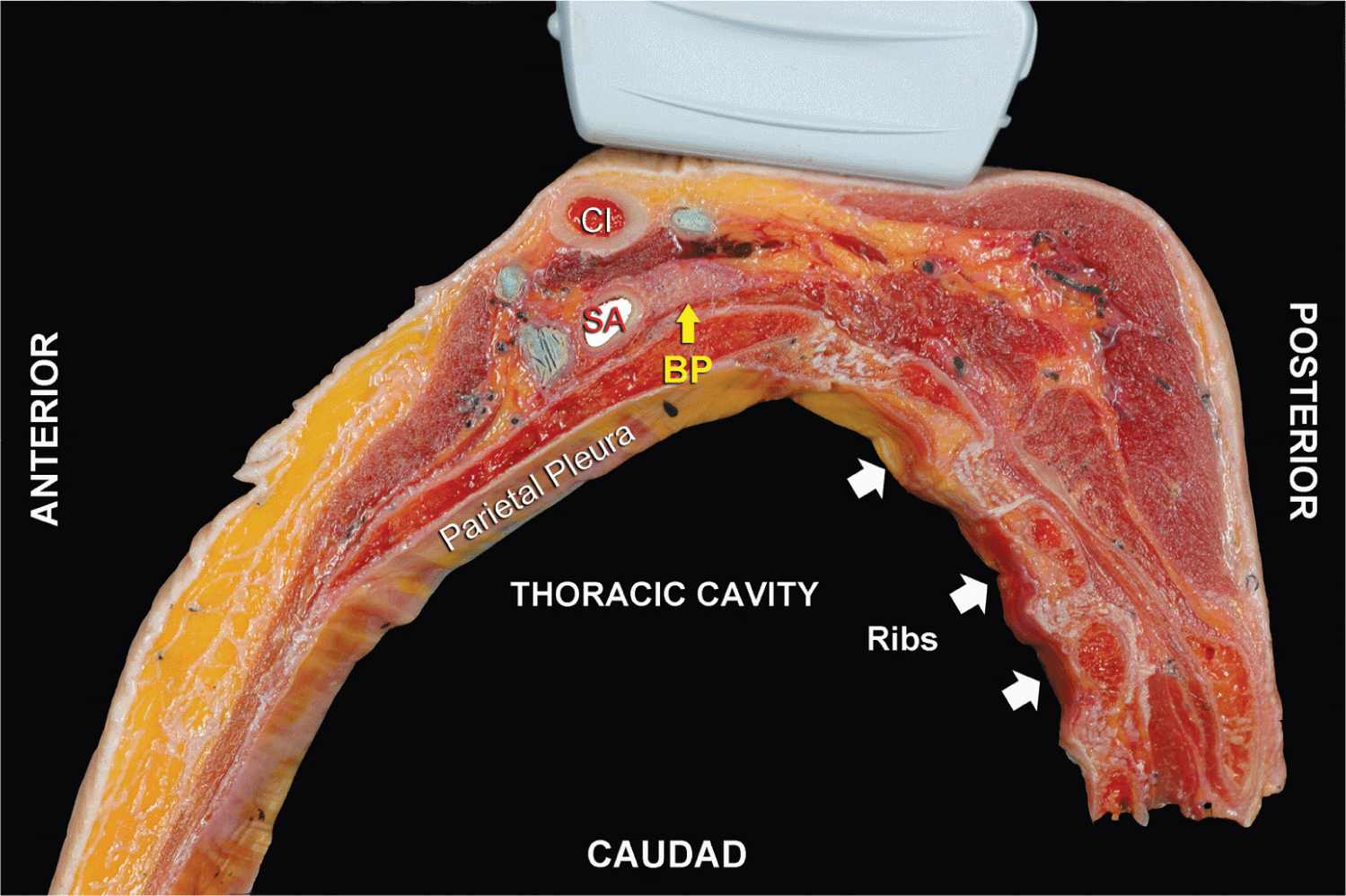
FIGURE 30-2. Anatomy of the supraclavicular brachial plexus with proper transducer placement slightly obliquely above the clavicle (Cl). SA, subclavian artery; arrow, brachial plexus (BP).
Ultrasound Anatomy
The subclavian artery crosses over the first rib between the insertions of the anterior and middle scalene muscles, at approximately the midpoint of the clavicle. The pulsating subclavian artery is readily apparent, whereas the parietal pleura and the first rib can be seen as a linear hyperechoic structure immediately lateral and deep to it, respectively (Figure 30-3). The rib, as an osseous structure, casts an acoustic shadow, so that the image field deep to the rib appears anechoic, or dark. A reverberation artifact (refer to Chapter 26) often occurs, mimicking a second subclavian artery beneath the rib. The brachial plexus can be seen as a bundle of hypoechoic round nodules (e.g., “grapes”) just lateral and superficial to the artery (Figures 30-3, 30-4, 30-5A and B). It is often possible to see the fascial sheath enveloping the brachial plexus. Depending at the level at which the plexus is scanned and the transducer orientation, brachial plexus can have an oval or flattened appearance (Figure 30-5A and B). Two different sonographic appearances of the brachial plexus (one oval and one flattened) are easily seen by changing the angle of the transducer orientation during imaging. Lateral and medial to the first rib is the hyperechoic pleura, with lung tissue deep to it. This structure can be confirmed by observation of a “sliding” motion of the viscera pleura with the patient’s respiration. The brachial plexus is typically visualized at a 1- to 2-cm depth at this location, an important anatomical characteristic of the plexus that must be kept in mind throughout the procedure.
FIGURE 30-3. Unlabeled ultrasound image of the supraclavicular brachial plexus.
FIGURE 30-4. Supraclavicular brachial plexus (BP) is seen slightly superficial and lateral to the subclavian artery (SA). Brachial plexus is enveloped by a tissue sheath (white arrows). Note the intimate location of the pleura and lung to the brachial plexus and subclavian artery. Middle scalene muscle (MSM). White arrows: Prevertebral fascia.
FIGURE 30-5. (A) Ultrasound image of the brachial plexus (BP) assuming an oval shape and circled by the tissue sheath (yellow arrows). (B) Ultrasound image of the BP at the supraclavicular fossa with the downward orientation of the transducer. The brachial plexus assumes a flatter configuration as it descends underneath the clavicle into the infraclavicular fossa. SA, subclavian artery. ASM, anterior scalene muscle.
Distribution of Blockade
The supraclavicular approach to the brachial plexus blockade results in anesthesia of the upper limb below the shoulder because all trunks and divisions can be anesthetized. The medial skin of the upper arm (intercostobrachial nerve, T2), however, is never anesthetized by any technique of the brachial plexus block and when needed can be blocked by an additional subcutaneous injection just distal to the axilla. For a more comprehensive review of the brachial plexus anatomy and distribution, see Chapter 1, Essential Regional Anesthesia Anatomy.
Equipment
Equipment needed includes the following:
• Ultrasound machine with linear transducer (8–14 MHz), sterile sleeve, and gel (or other coupling medium; e.g. saline)
• Standard nerve block tray (described in Chapter 3)
• 20 to 25 mL local anesthetic
• 5-cm, 22-gauge short-bevel insulated stimulating needle
• Peripheral nerve stimulator
• Sterile gloves
Landmarks and Patient Positioning
Any position that allows comfortable placement of the ultrasound transducer and needle advancement is appropriate. This block can be performed with the patient in the supine, semi-sitting (our favorite), or slight oblique position, with the patient’s head turned away from the side to be blocked. When possible, asking the patient to reach for the ipsilateral knee will depress the clavicle slightly and allow better access to the structures of the anterolateral neck. Also, a slight elevation of the head of the bed is often more comfortable for the patient and allows for better drainage and less prominence of the neck veins (Figure 30-1).
Adherence to strict anatomic landmarks is of lesser importance for the ultrasound-guided supraclavicular block than for the surface anatomy techniques. However, knowledge of the underlying anatomy and the position of the brachial plexus in relation to the subclavian artery, first rib, and pleura are important for the success and safety of the technique. Scanning is usually started just above the clavicle at approximately its midpoint.
Technique
With the patient in the proper position (we prefer semi-sitting position), the skin is disinfected and the transducer is positioned in the transverse plane immediately superior to the clavicle at approximately its midpoint. The transducer is tilted caudally to obtain a cross-sectional view of the subclavian artery (Figures 30-6). The brachial plexus is seen as a collection of hypoechoic oval structures lateral and superficial to the artery.

FIGURE 30-6. Supraclavicular brachial plexus; transducer position and needle insertion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








