Ultrasound-Guided Cervical Plexus Block

FIGURE 28-1. Needle and transducer position to block the superficial cervical plexus using a transverse view.
General Considerations
The goal of the ultrasound-guided technique of superficial cervical plexus block is to deposit local anesthetic in the vicinity of the sensory branches of the nerve roots C2, C3, and C4. Advantages over the landmark-based technique include the ability to ensure the spread of local anesthetic in the correct plane and therefore increase the success rate and avoid too deep needle insertion and/or inadvertent puncture of neighboring structures. Both in-plane and out-of-plane approaches can be used. The experience with ultrasound-guided deep cervical plexus is still in its infancy and not described here.
Ultrasound Anatomy
The sternocleidomastoid muscle (SCM) forms a “roof” over the nerves of the superficial cervical plexus (C2-4). The roots combine to form the four terminal branches (lesser occipital, greater auricular, transverse cervical, and supraclavicular nerves) and emerge from behind the posterior border of the SCM (Figure 28-2). The plexus can be visualized as a small collection of hypoechoic nodules (honeycomb appearance or hypo-echoic [dark] oval structures) immediately deep or lateral to the posterior border of the SCM (Figure 28-3), but this is not always apparent. Occasionally, the greater auricular nerve is visualized (Figure 28-4) on the superficial surface of the SCM muscle as a small, round hypoechoic structure. The SCM is separated from the brachial plexus and the scalene muscles by the prevertebral fascia, which can be seen as a hyperechoic linear structure. The superficial cervical plexus lies posterior to the SCM muscle, and immediately underneath the prevertebral fascia overlying the interscalene groove. (Figure 28-3).
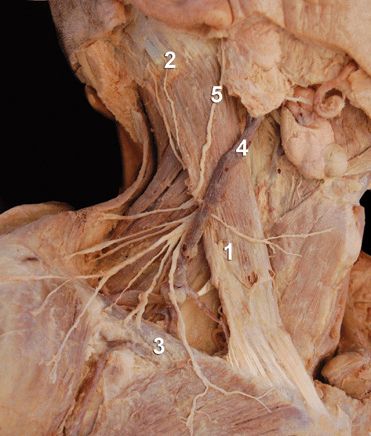
FIGURE 28-2. Anatomy of the superficial cervical plexus. ![]() sternocleidomastoid muscle.
sternocleidomastoid muscle. ![]() mastoid process.
mastoid process. ![]() clavicle.
clavicle. ![]() external jugular vein. Superficial cervical plexus is seen emerging behind the posterior border of the sternocleidomastoid muscle at the intersection of the muscle with the external jugular vein.
external jugular vein. Superficial cervical plexus is seen emerging behind the posterior border of the sternocleidomastoid muscle at the intersection of the muscle with the external jugular vein. ![]() Greater auricular nerve.
Greater auricular nerve.
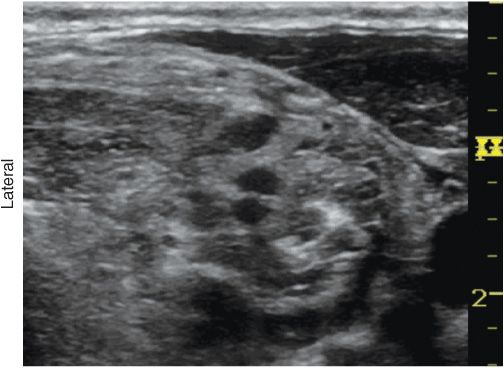
FIGURE 28-3. Superficial cervical plexus-transverse view.
FIGURE 28-4. Branches of the superficial cervical plexus (CP) emerging behind the prevertebral fascia that covers the middle (MSM) and anterior (ASM) scalene muscles, and posterior to the sternocleidomastoid muscle (SCM). White arrows, Prevertebral Fascia; CA, carotid artery; PhN, phrenic nerve.
Distribution of Blockade
The superficial cervical plexus block results in anesthesia of the skin of the anterolateral neck and the anteauricular and retroauricular areas, as well as the skin overlying and immediately inferior to the clavicle on the chest wall (Figure 28-5).
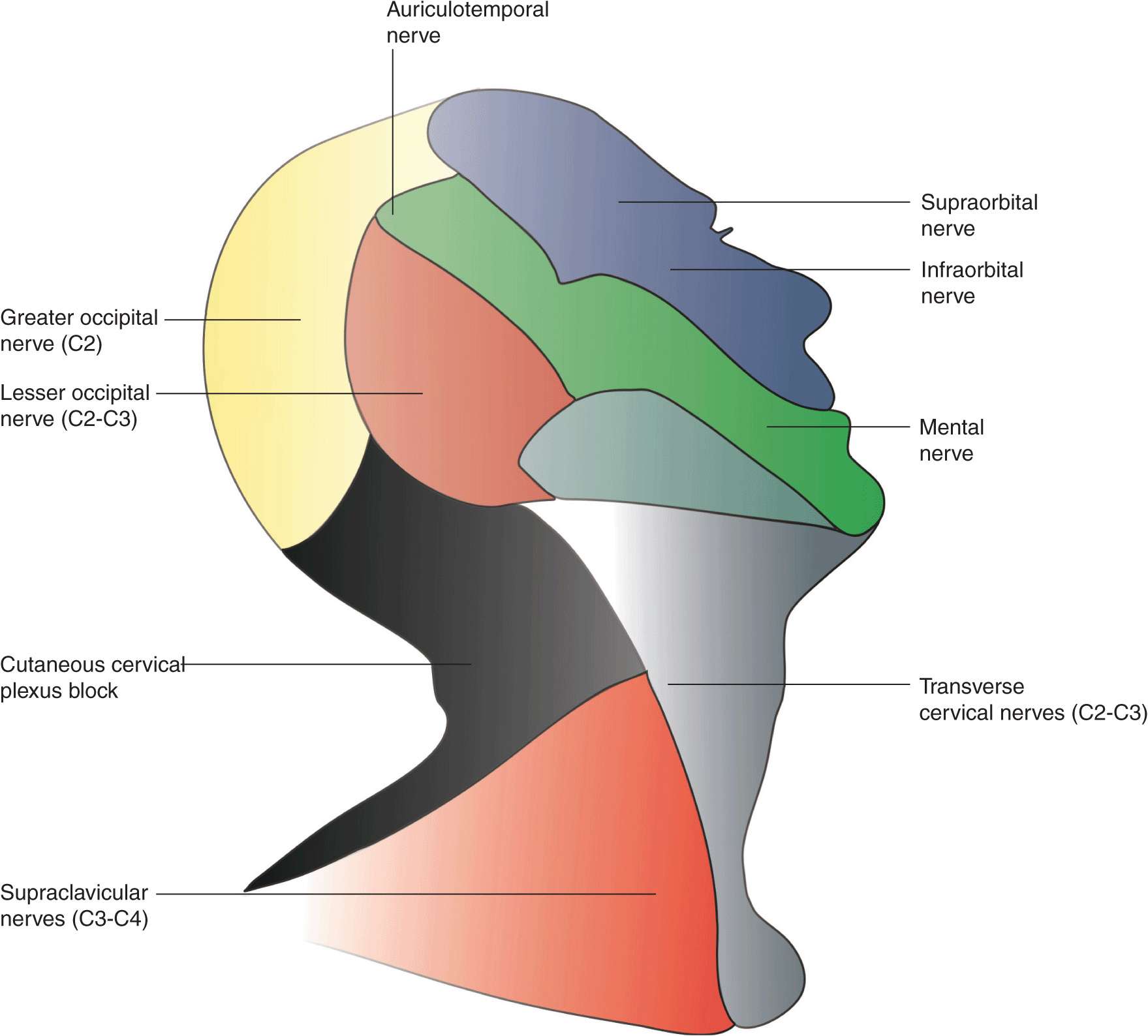
FIGURE 28-5. Sensory distribution of the cervical plexus and innervation of the lateral aspect of the face.
Equipment
Equipment needed includes the following:
• Ultrasound machine with linear transducer (8–18 MHz), sterile sleeve, and gel
• Standard nerve block tray (described in the equipment section)
• Two 10-mL syringes containing local anesthetic
• A 2.5-in, 23- to 25-gauge needle attached to low-volume extension tubing
• Sterile gloves
Landmarks and Patient Positioning
Any patient position that allows for comfortable placement of the ultrasound transducer and needle advancement is appropriate. This block is typically performed in the supine or semi-sitting position, with the head turned slightly away from the side to be blocked to facilitate operator access (Figure 28-6A and B). The patient’s neck and upper chest should be exposed so that the relative length and position of the SCM can be assessed.

FIGURE 28-6. Superficial cervical plexus block. A) Transverse approach with an in-plane needle advancement. B) Longitudinal approach.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








