CHAPTER 17
Trigeminal Ganglion and Nerve Block
INTRODUCTION
Blockade of the trigeminal ganglion and/or its peripheral branches is a useful technique that can benefit patients who have refractory facial pain and certain types of headaches that have not responded to conservative measures. The trigeminal ganglion was first described by the anatomist Johann Gasser and blockade of the ganglion was first described by Hartel in 1912.
INDICATIONS
Indications for blockade of the ganglion and/or its peripheral branches include:
• Tic douloureux (trigeminal neuralgia)
• Atypical trigeminal neuralgia
• Chronic, intractable cluster headaches1–5
• Persistent idiopathic facial pain
• Herpes zoster
• Palliation of cancer-related pain
RELEVANT ANATOMY
The trigeminal ganglion resides in the middle cranial fossa.6–8 The ganglion is formed by the fusion of a series of cell bodies that originate at the mid-pontine level of the brainstem. It is situated in a fold of dura mater that forms an invagination around the posterior two-thirds of the ganglion. This region is referred to as the Meckel cavity and contains cerebrospinal fluid.
• The ganglion is bound medially by the cavernous sinus and optic and trochlear nerves; superiorly by the inferior surface of the temporal lobe of the brain; and posteriorly by the brain stem. Access to the ganglion requires passage of the block needle through foramen ovale.
• The ganglion is situated in the posterior part of the sphenoid bone, posterolateral to foramen rotundum.
• Within foramen ovale lies the mandibular nerve, accessory meningeal artery and the lesser petrosal nerve.
• The ganglion has three major divisions: ophthalmic (V1), maxillary (V2), and mandibular (V3). The ophthalmic division is located dorsally, the maxillary branch intermediate, and the mandibular branch ventrally. This arrangement is important when a thermal rhizotomy is being considered.
• The ophthalmic division leaves the ganglion and passes into the orbit through the superior orbital fissure. It further divides into the supraorbital, supratrochlear, and nasociliary nerves which innervate the forehead and the nose.8
• The maxillary division exits the middle cranial fossa via foramen rotundum, crosses the pterygopalatine fossa, and enters the orbit through the inferior orbital fissure. Branches include the infraorbital, superior alveolar, palatine, and zygomatic nerves which carry sensory information from the maxilla and overlying skin, the nasal cavity, palate, nasopharynx and meninges of the anterior and middle cranial fossa.8
• The mandibular division exits through foramen ovale and divides into the buccal, lingual, inferior alveolar, and auriculotemporal nerves. These nerves carry sensory input from the buccal region, the side of the head and scalp, and the lower jaw including teeth, gums, anterior two-thirds of the tongue, chin, and lower lip.8
• The motor component of V3 innervates the masseter, temporalis, and medial and lateral pterygoids.
• The ganglion interferes with the autonomic nervous system via the ciliary, sphenopalatine, otic, and submaxillary ganglia. It also communicates with the oculomotor, facial, and glossopharyngeal nerves.
The key to successively block the trigeminal ganglion is to identify the following structures radiographically:
• Ramus of the mandible
• Foramen ovale
• Sella turcica
• Clivus
• Mastoid air cells
External landmarks that are important include:
• Ipsilateral pupil
• Ipsilateral tragus
PREOPERATIVE CONSIDERATIONS
Given that blockade of the trigeminal ganglion can be a painful procedure, conscious sedation may be required. With this in mind, the patient’s overall health status must be maximized prior to the procedure.
• All prescribed medications should be continued unless there is a contraindication.
• The vascular nature of the region necessitates a review of the concomitant use of anticoagulants.
• While guidelines exist for the use of anticoagulants and regional anesthesia,10 there are no guidelines per se when it comes to pain management procedures.
• While up for debate, our institution holds nonsteroidal anti-inflammatory drugs for 4 days, aspirin (baby and full dose) for 5 days, Coumadin for 5 days (with a preprocedure INR), clopidogrel (Plavix) for 7 to 10 days, and ticlopidine (Ticlid) for 10 to 14 days prior to the procedure.
• There is very little information regarding newer anticoagulant drugs such as dabigatran etexilate (Pradaxa) and rivaroxaban (Xarelto) in relation to pain management procedures.
The benefits and risks of discontinuing an anticoagulant must be entertained and discussed with the patient prior to the procedure. Permission from the prescribing physician to discontinue the medication should also be sought and documented. One also needs to question the patient about homeopathic remedies, especially anything that begins with the letter “G,” eg, ginko, garlic, ginseng, and fish oil, as these can also affect bleeding status.
CONTRAINDICATIONS
Contraindications are broken down into absolute and relative. While absolute contraindications are straight forward, relative contraindications require a benefit-risk discussion with the patient. Absolute contraindications for a trigeminal ganglion block are:
• Increased intracranial pressure
• Patient refusal
• Infection in the region where the block is to be performed
• Inability to stop anticoagulant medication
• Untreated psychopathologies
Relative contraindications include anticoagulant use.
FLUOROSCOPIC VIEWS
• The initial anterior-posterior fluoroscopic image should be with the head in the neutral position with the nasal septum squared (Figure 17-1). The nasal septum unless deviated should appear as a solid black line.
• Submental view. The image intensifier should be angled approximately 25 to 30 degrees in the caudal direction (Figure 17-2). This allows the physician to look up into the base of the skull.
• Oblique view. The image intensifier should be rotated approximately 20 to 30 degrees toward the intended side to bring the foramen ovale into view (Figure 17-3). The foramen should be close to the medial side of the mandible at the level of the second molar.
• Lateral view. Sella turcica should be identified just cephalad and posterior to the shadow of the pterygomaxillary fissure (Figure 17-4).
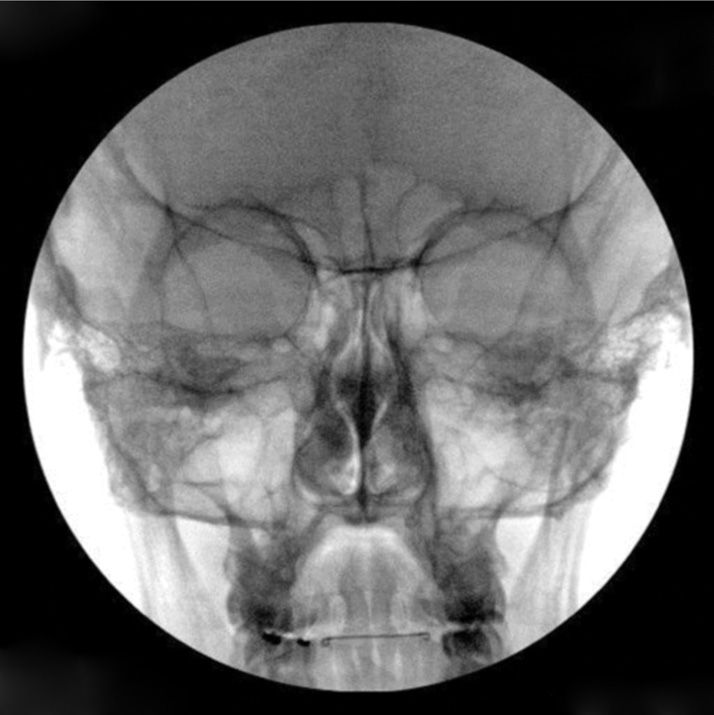
Figure 17-1. AP of the face. The septum of the nose is squared.
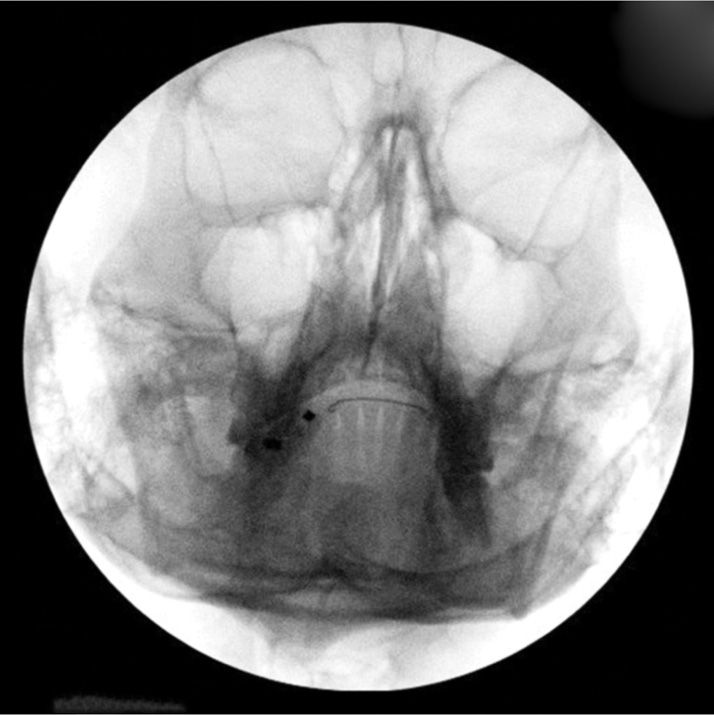
Figure 17-2. A 30-degree submental view.
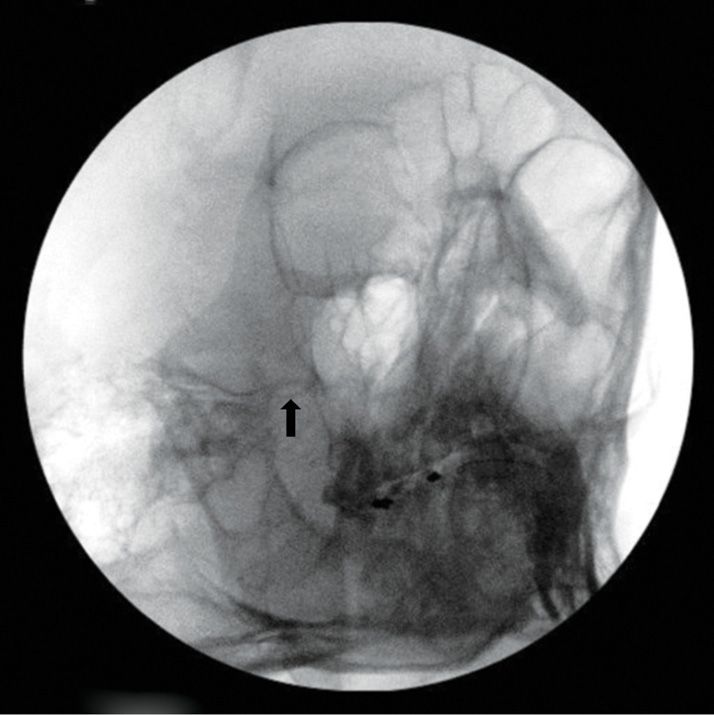
Figure 17-3. A 20-degree oblique view. The arrow indicates foramen ovale.

Figure 17-4. Lateral view. The white arrow denotes the angle formed by the clivus and the petrous portion of the temporal bone.
Equipment
• 25-gauge, 1.5-in needle for skin infiltration
• 22-gauge, 3.5-in spinal needle or 22-gauge, 10-cm blunt tipped block needle
• 22-gauge radiofrequency needle with a 2 to 3-mm active tip (for thermal rhizotomy)
• 18-gauge angiocatheter (if using a blunt needle)
• 5-cc syringe for local anesthetic
• 3-cc syringe for contrast
• 3-cc syringe for local anesthetic/steroid mixture
• Extension connector tubing
Medications
• 1% lidocaine (skin infiltration)
• 0.25% bupivacaine or 0.2% ropivacaine (block local anesthetic)
• Omnipaque 240 (nonionic, water-soluble contrast)
• Corticosteroid (for radiofrequency lesioning)
TECHNIQUE
As previously stated, blockade of the trigeminal ganglion can be a painful procedure and conscious sedation may be necessary. Therefore, monitoring to include heart rate, ECG, blood pressure, and pulse oximetry is required. Supplemental oxygen should also be provided through a nasal cannula positioned out of the way of the sterile field.
• Place the patient on the bed supine with the head in a neutral position. A radiolucent head cradle can also be used to keep the head in a stable position.
• Prep and drape the block side sterilely, keeping the ipsilateral eye exposed.
• Obtain a PA view and adjust the C-arm to square the nasal septum.
• Tilt the image intensifier approximately 25 to 30 degrees in the caudal direction.
• Oblique the image intensifier 20 to 30 degrees ipsilaterally.
• Make subtle adjustments to identify foramen ovale which should be just medial to the ramus of the mandible (Figure 17-5).
• Mark the skin entry site which is approximately 2 cm lateral to the corner of the mouth.
• Anesthetize the skin and insert the block needle. Advance in a coaxial fashion using intermittent fluoroscopic images (Figure 17-6). If utilizing external landmarks, aim toward the midline, ipsilateral pupil and just anterior to the tragus of the ear. If using the blunt needle, the angiocatheter should be inserted first.
• Once the needle is engaged in the soft tissue of the cheek, obtain a lateral image to check the depth and direction of the needle. Aim toward the angle produced by the clivus and the petrous portion of the temporal bone (Figure 17-4).
• Check an oblique image to ensure the needle is advancing toward foramen ovale.
• Return to the lateral view and advance the needle through foramen ovale (Figure 17-7). With a blunt needle, slight force may be required to advance the tip through foramen ovale. Be careful not to advance the needle tip past the clivus as the tip could enter brain matter. If using a sharp needle, cerebrospinal fluid (CSF) may be encountered if the tip of the needle passes through the dura covering the ganglion. In the first author’s experience, this has not occurred with the use of a blunt-tipped needle.
• Remove the stylet and aspirate. If blood is aspirated, reposition the needle tip and repeat the aspiration. If blood is encountered again, reposition the needle tip. If blood is once again encountered, abort the procedure. Aspiration of CSF also requires repositioning of the needle tip. CSF will not interfere with a thermal rhizotomy, but it could lead to side effects and complications if a chemical rhizotomy is planned. If cerebrospinal fluid is obtained, the needle tip can be withdrawn until fluid is no longer appreciated. If an abundant cerebrospinal fluid leak is present, the remainder of the procedure should be halted. With a significant leak, a high spinal block can be caused with even low volumes of local anesthetic. A small leak of cerebrospinal fluid may or may not cause a high spinal and if present, the pain practitioner should proceed with caution.
• After negative aspiration for blood and CSF, slowly inject a small amount (no more than 0.5-1.0 cc) of nonionic, water-soluble contrast to confirm position and filling of the Meckel cavity. Any vascular runoff requires repositioning of the needle.
• Slowly inject local anesthetic in volumes of 0.25-0.5 cc at a time, up to 1-2 cc, and observe for effect. Remove the needle.

Figure 17-5. Submental oblique. Foramen ovale is just cephalad to the black arrow.

Figure 17-6. A 22-gauge curved, blunt block needle slightly posterior to foramen ovale.
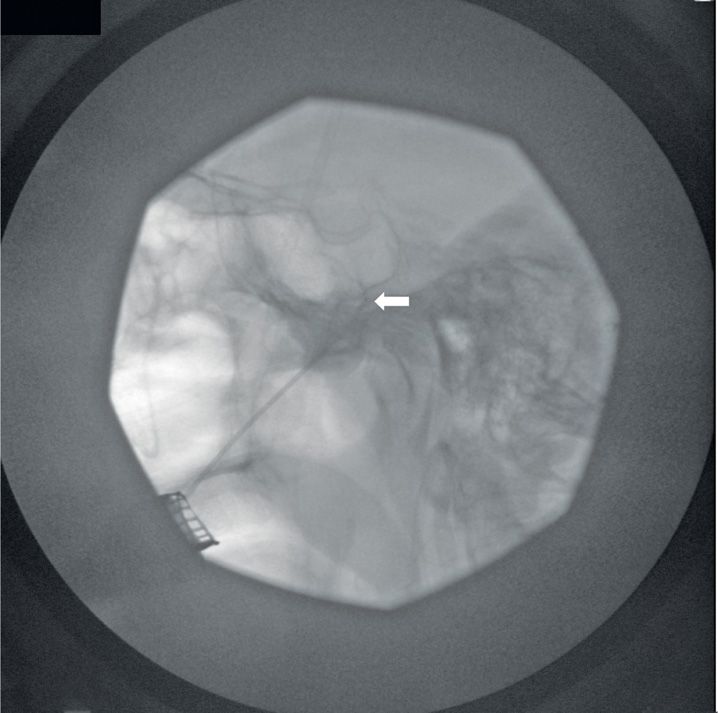
Figure 17-7. Final position of the needle on the lateral view. The white arrow indicates the tip of the needle.
THERMAL RHIZOTOMY
Needle placement is the same as with a local anesthetic block with a few differences. In place of the block needle, a radiofrequency needle of the same caliber with a 2- to 3-mm active tip is used. Sensory and motor stimulations are required to properly position the needle tip. This requires the patient to be able to respond to questions, so the level of sedation needs to be monitored closely.
• After the needle has entered foramen ovale, perform motor stimulation at 2 Hz, up to 2 V. Mandible contraction should be observed secondary to stimulation of the mandibular division. Next, perform sensory stimulation at 50 Hz, up to 1 V. The goal is to position the needle tip on the portion of the ganglion that will elicit a paresthesia in the desired division.
• Once the needle tip is positioned, and after negative aspiration of blood and CSF, inject local anesthetic and wait approximately 1 minute. The first author also mixes a small amount of corticosteroid (2 mg dexamethasone) with the local anesthetic.
• Commence lesioning at 70°C for 1 minute. Repeat stimulation and observe if the paresthesia in the intended division has diminished. Based on the repeat stimulation, a second lesion may be necessary.
• If lesioning of more than one division is required, the needle tip will have to be repositioned to create a larger lesion. Begin with lesioning of the portion of the ganglion of the more distal division, and withdraw the needle tip to the more proximal portion, eg, lesion the portion of the ganglion corresponding to the maxillary division before the mandibular division.
• Lesioning of the ophthalmic division requires special consideration as this division innervates the cornea. Perform lesioning at 60°C. Check the corneal reflex intermittently during lesioning. If the reflex diminishes, stop the lesioning.
CHEMICAL RHIZOTOMY
Glycerol and phenol in glycerin can also be used to achieve long-term analgesia.
• Once through the foramen ovale, advance the needle until cerebrospinal fluid is observed returning through the needle.
• Place the patient in a semisitting position with the neck flexed. Inject water-soluble, nonionic contrast solution in 0.1 mL aliquots (up to 0.5 mL) into the trigeminal cistern.11 Failure of visualization or diffusion of the contrast requires repositioning the needle.
• Once the cistern is visualized, draw back the contrast material by free flow. The flow of contrast is slower than cerebrospinal fluid.
• Inject the same amount of glycerol into the cistern.
• Flush the needle with 0.5 mL of saline prior to removal.
• Keep the patient in a semisitting position for 2 hours. During the procedure, patients often report pain, burning, or paresthesia in the affected division(s).16
PULSED RADIOFREQUENCY
The use of nonthermal radiofrequency, ie, pulsed radiofrequency, can also be performed.
• After proper positioning of the needle tip, perform 2 to 3 pulsed radiofrequency cycles for 120 seconds each at 45 V. The temperature of the needle tip rarely exceeds 42°C, thus local anesthetic is not required.
• If significant masseter contraction is noted during pulsing, inject 1 to 2 mL of local anesthetic to diminish this, or hold the patient’s mouth closed with your hand while the cycles are completed.
POSTPROCEDURE
Monitor the patient for at least 1 hour. In the case of a chemical rhizotomy, observe for 2 hours. Vitals signs including blood pressure, heart rate, and oxygen saturation should be recorded. An ice pack over the injection site can be helpful to decrease swelling and pain. Once awake, assess the patient’s pain level and degree of hypoesthesia in the trigeminal division blocked or lesioned.
COMPLICATIONS
The location of the trigeminal ganglion and adjacent structures is important in understanding the potential complications of this procedure. Also, prior to rhizotomy the difference between a side effect and a complication must be thoroughly explained to the patient. Sensory loss in the division lesioned is expected and is not considered a complication. It can be as high as 98% with thermal rhizotomy compared to 60% seen with chemical rhizotomy.12 Thermal rhizotomy (TR) had a higher rate of complications at 29.2% compared to chemical rhizotomy (CR) at 24.8%.13 Potential complications include, but are not limited to:
• Bleeding
• Retrobulbar hematoma
• Local infection
• Meningitis
• High spinal
• Adjacent cranial nerve palsies (usually transient)
• Corneal anesthesia (TR > CR),14 keratitis, ulceration, and hypesthesia
• Masseter weakness (TR >>> CR)14 when lesioning the mandibular division
• Anesthesia dolorosa up to 4% (TR > CR)14
TRIGEMINAL NERVE DIVISION BLOCKS
Ophthalmic Nerve Blocks
The ophthalmic division can only be blocked at 2 of its peripheral branches which are the supraorbital and supratrochlear nerves. The usual indications are trigeminal neuralgia and post-herpetic neuralgia although it has been used for intractable frontal headaches. Preoperative considerations and contraindications are essentially the same as for the trigeminal ganglion block. Sedation is not typically required. Complications include bleeding, hematoma, infection, and nerve injury.
For the supraorbital nerve:
• Palpate the supraorbital notch/foramen which is located on the mid superior orbital ridge.
• After sterile prep, insert a short 25- or 22-gauge needle perpendicular to the skin and advance until bone is touched. Avoid advancing the needle into the foramen.
• Withdraw the needle slightly and after negative aspiration for blood, inject 1 to 2 cc of local anesthetic.
For the supratrochlear nerve:
• Palpate the supratrochlear notch/foramen which is located on the medial aspect of the superior orbital ridge in line with the medial canthus.
• After sterile prep, insert a short 25- or 22-gauge needle perpendicular to the skin and advance until bone is touched. Avoid advancing the needle into the foramen.
• Withdraw the needle slightly and after negative aspiration for blood, inject 1 to 2 cc of local anesthetic.
Maxillary Nerve Block
Blockade of the maxillary nerve can be accomplished by blocking it in the pterygopalatine fossa or by blocking one of its peripheral branches, the infraorbital nerve. Preoperative considerations and contraindications are essentially the same as for the trigeminal ganglion block. Indications are trigeminal neuralgia of the maxillary division, and idiopathic or secondary maxillary neuralgia. Complications are the same as for the trigeminal ganglion block except for the ophthalmic complications and high spinal. An infraorbital nerve block does not usually require sedation, but for the maxillary nerve block in the pterygopalatine fossa, follow the trigeminal ganglion block protocol.
Infraorbital nerve block:
• Palpate the infraorbital notch/foramen which is located on the mid inferior orbital ridge.
• After sterile prep, insert a short 25- or 22-gauge needle perpendicular to the skin and advance until bone is touched. Avoid advancing the needle into the foramen.
• Withdraw the needle slightly and after negative aspiration for blood, inject 1 to 2 cc of local anesthetic.
Maxillary nerve block:
• Place the patient in the supine position with the head in a neutral position.
• Obtain a lateral fluoroscopic image to identify the coronoid notch. It can also be identified by asking the patient to open and close their mouths, and with palpation anterior and inferior to the external auditory meatus.
• Once the landmarks are identified, anesthetize the skin and advance a 22-gauge, 3.5-in spinal needle or blunt tipped block needle (will first require insertion of an 18-gauge angiocatheter) perpendicular to the skin of the side of the face, just below the zygomatic arch directly in the center of the coronoid arch.
• Once the lateral pterygoid plate is contacted (at about 4-5 cm from the skin), redirect the needle cephalad, anterior and medial toward the cephalad portion of the pterygopalatine fossa. Intermittent, lateral fluoroscopic images will facilitate proper placement of the needle.
• Obtain an AP fluoroscopic image to check the depth of the needle. The tip should be cephalad to the middle turbinate and adjacent to the palatine bone. Sometimes a paresthesia is elicited and should be felt in the upper teeth.
• After negative aspiration for blood, inject 3 cc of local anesthetic. For a neurolytic block, 1 to 1.5 cc of 6% phenol in iohexol can be injected.
• A thermal rhizotomy is not recommended, but pulsed radiofrequency can be performed. Once a 10-cm radiofrequency needle with a 5-mm active tip is in position, perform sensory stimulation at 50 Hz, up to 1 V. Stimulation at less than 0.5 V is desirable. The patient should experience a paresthesia in the upper teeth. Inject 1 cc of local anesthetic and perform 2 to 3 pulsed radiofrequency cycles for 120 seconds each at 45 V.
Mandibular Nerve Block
Blockade of the mandibular nerve can be accomplished by following the coronoid approach to the maxillary nerve protocol, but redirecting the needle posteriorly when the lateral pterygoid plate is touched. Preoperative considerations and contraindications are essentially the same as for the trigeminal ganglion block. Indications are trigeminal neuralgia of the mandibular division, and idiopathic or secondary mandibular neuralgia. Complications are the same as for the trigeminal ganglion block except for the ophthalmic complications and high spinal. Weakness of the muscle of mastication can occur after a neurolytic procedure and this should be thoroughly discussed. Follow the trigeminal ganglion block protocol with regards to sedation.
• Place the patient in the supine position with the head in a neutral position.
• Obtain a lateral fluoroscopic image to identify the coronoid notch.
• Once the landmarks are identified, anesthetize the skin and advance a 22-gauge, 3.5-in spinal needle or blunt-tipped block needle (will first require insertion of an 18-gauge angiocatheter) perpendicular to the skin of the side of the face, just below the zygomatic arch directly in the center of the coronoid arch.
• Once the lateral pterygoid plate is contacted (at about 4-5 cm from the skin), obtain an AP fluoroscopic image to confirm location.
• Redirect the needle posteriorly and inferiorly no more than 1 cm. A paresthesia is usually elicited in the lower jaw and lip, ear, and ipsilateral tongue.
• After negative aspiration for blood, inject 3 cc of local anesthetic. For a neurolytic block, 1 to 1.5 cc of 6% phenol in iohexol can be injected.
• A thermal rhizotomy is not recommended, but pulsed radiofrequency can be performed. Once a 10-cm radiofrequency needle with a 5-mm active tip is in position, perform sensory stimulation at 50 Hz, up to 1 V. Stimulation at less than 0.5 V is desirable and should be felt in the lower jaw and lip, ear, and ipsilateral tongue. Inject 1 cc of local anesthetic and perform 2 to 3 pulsed radiofrequency cycles for 120 seconds each at 45 V.
CLINICAL PEARLS
• Detailed knowledge of the anatomy of the head and neck is imperative. This will increase the success of the block while theoretically decreasing the potential for complications.
• Always perform a diagnostic block first before proceeding to a rhizotomy. On occasion, a diagnostic block can have therapeutic benefit.
• Thoroughly explain the difference between an expected side effect and a complication before performing a rhizotomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






