Fig. 12.1
Sagittal T2 MRI with cervical spinal levels identified; note the limited CSF signal (bright white on T2) in the cervical spine as compared with the thoracic spine
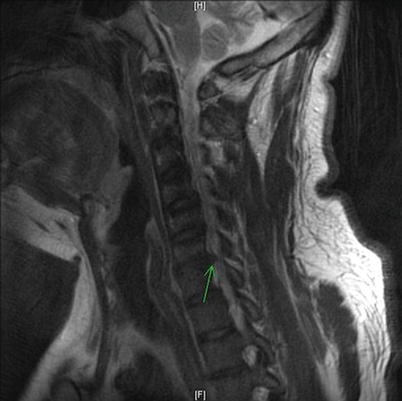
Fig. 12.2
Sagittal T2 MRI with C6–C7 disk herniation identified by arrow
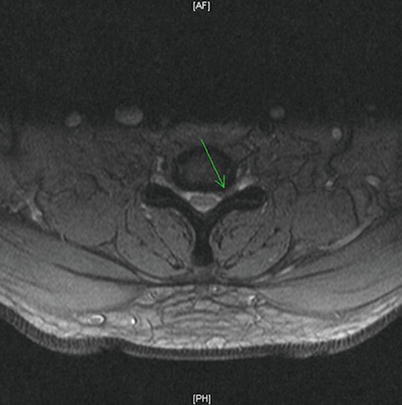
Fig. 12.3
Axial T2 MRI with leftward C6–C7 disk herniation identified by arrow

Fig. 12.4
Lateral fluoroscopic view post-contrast injection; note contrast spread in the posterior epidural space to C6 level

Fig. 12.5
AP fluoroscopic view post-contrast injection; note needle placement at C7-T1 interspace
12.2 Case Discussion
12.2.1 Anatomy of the Cervical Epidural Space
The boundaries of the epidural space are as follows: superiorly by the foramen magnum, inferiorly by the sacral hiatus, anteriorly by the posterior longitudinal ligament, and posteriorly by the ligamentum flavum . The diameter of the posterior epidural space is approximately 3–5 mm at the C7–T1 interspace. The ligamentum flavum is also relatively thin (and possibly discontinuous in the cervical spine) as compared to the lumbar region, making LOR more subtle in the cervical spine. Cadaver evidence has shown that the ligamentum flavum frequently fails to fuse in the midline over the cervical interspaces and that midline gaps were observed in more than 50% of specimens [1, 2]. Therefore, injection at the C7–T1 level is favored, taking into account that injected substances will likely spread over multiple interspaces in the cervical spine, so most levels can be reached from a C7–T1 epidural entry. Some practitioners favor a paramedian approach due to the possibility of incomplete fusion of the ligamentum flavum in the midline, whereas other practitioners favor a midline approach to avoid neural and vascular structures that may be located more laterally.
12.2.2 Technique for Interlaminar Cervical Epidural Steroid Injection
Typically the patient is positioned prone on the fluoroscopy table. Some practitioners perform the procedure in the sitting position; however, it may be more difficult for the patient to hold his/her head in a fixed position while sitting. After sterile prep and drape is performed, fluoroscopy is used to identify the C7–T1 interspace and optimize the angle of entry. Local infiltration is performed, and the epidural needle is introduced through the skin and subcutaneous tissue. The first structure to be encountered deep to the subcutaneous tissue is the supraspinous ligament. After passing through the supraspinous ligament, the needle will next traverse the ligamentum nuchae, a large structure that bridges the dorsal edges of the cervical spinous processes. Next, the interspinous ligament is encountered, which runs between the spinous processes. The density of this ligament is such that the needle will remain seated even when released, as compared with more superficial structures. The interspinous ligament then adjoins the ligamentum flavum , and occasionally the practitioner may sense a change in resistance at the junction between these two ligaments. Resistance will often increase once again as the needle progresses into the ligamentum flavum. (See Fig. 12.6 for an illustration of the above structures and their anatomical relationships.) A noticeable and complete LOR should occur as the needle passes through the ligamentum flavum into the epidural space. Whether using LOR to saline or air, there should be almost no resistance to injection into the epidural space. If the patient complains of a significant increase in pain or the practitioner notes a change in resistance to injection, the procedure should be halted and needle placement reassessed. The use of the hanging drop technique, whereby a non-styletted epidural needle topped with saline is advanced until the saline is pulled into the needle, has fallen out of favor due to an increased risk of dural puncture when compared with other methods. This phenomenon is best explained by the fact the epidural space may not always be in a negative pressure state, particularly in patients with spinal pathology (who are often presenting for ESI). If the epidural space is in a positive pressure state, no LOR will be obtained on entry into the epidural space, and the needle may be inadvertently advanced into the subarachnoid space or, worse, the spinal cord. Fluoroscopy is advocated as a safety measure among many practitioners; however, it is not a guarantee against complications. Following a negative aspiration for blood or CSF, injection of contrast should be done under live fluoroscopy. Another image may be obtained shortly after injection to verify that the location of the contrast has not changed or disappeared. Digital subtraction imaging (whereby images are produced using contrast medium by subtracting a pre-contrast image from post-contrast images) may also be useful to clarify contrast spread.
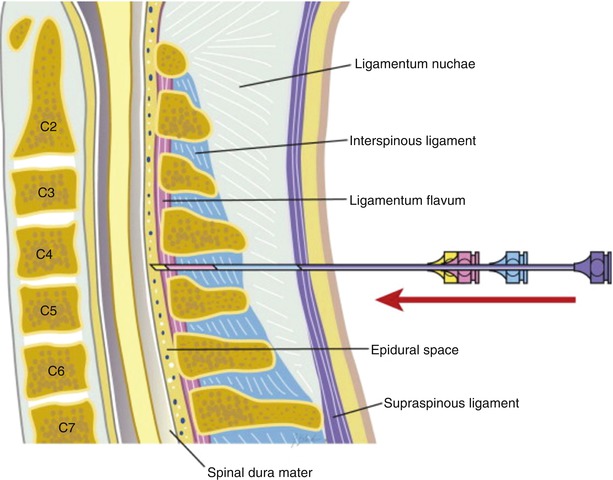
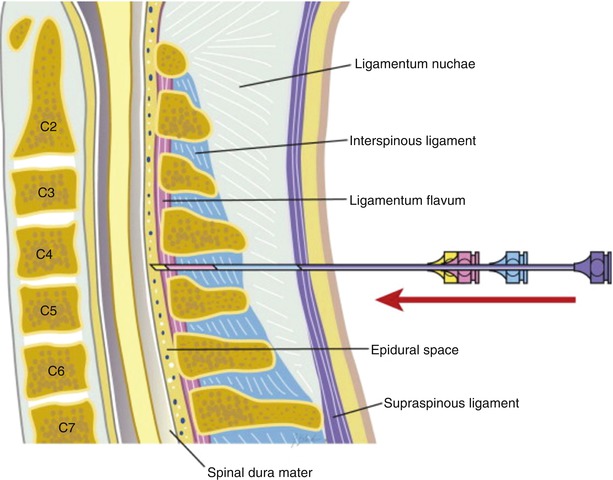
Fig. 12.6
Ligamentous anatomy of the cervical spine . Reprinted from Atlas of Interventional Pain Management, 4th Ed., Waldman SD, Cervical Epidural Block, pp. 178–187, Copyright (2015), with permission from Elsevier
12.2.3 Potential Complications of Interlaminar Cervical Epidural Steroid Injection
- 1.
Get Clinical Tree app for offline access
Dural puncture +/− intrathecal injection—estimated incidence less than 1%. Failure to recognize improper needle placement may result in immediate total spinal anesthesia (if local anesthetic is injected) with associated loss of consciousness, hypotension, and apnea (see Table 12.1 for signs and symptoms of total spinal anesthesia ).
- (a)
Management of high spinal anesthesia—the clinician must address and manage signs or symptoms, including applying the ABCs (airway, breathing, circulation):
Airway support including oxygen supplementation and positive pressure ventilation via mask or endotracheal tube if indicated
Administration of intravenous fluids and vasopressors and initiation of advanced cardiovascular life support (ACLS) protocol in the event of a cardiac arrest
- (b)
Management of dural puncture —there is currently no data to support the immediate treatment of dural puncture with epidural blood patch (EBP) , saline injection, or mobility restrictions. The patient should be counseled about the possibility and characteristics of a post dural puncture headache (PDPH) . If a PDPH presents, many practitioners advocate aggressive fluid intake, consumption of caffeinated beverages, and/or over-the-counter or prescription analgesics. If the patient does not respond to conservative measures, an EBP could be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



- (a)



