Fig. 35.1
Picture of the snail
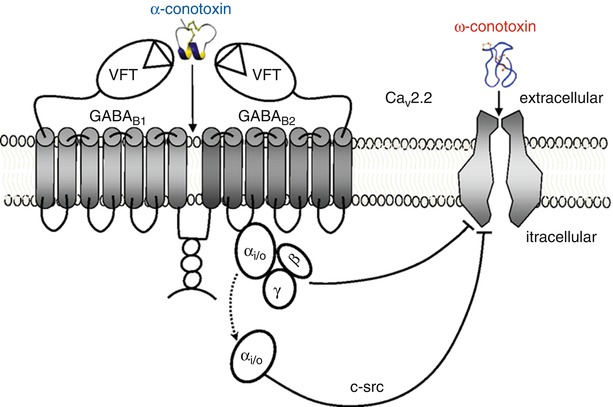
Fig. 35.2
Mechanism of action of conotoxin
35.2.2 N-Type Voltage-Gated Calcium Channel
In the nervous system, calcium is highly metabolically active and plays an important role in hormone secretion, synaptic transmission, gene expression, regulation of enzyme activity, and the modulation of synaptic plasticity [19–21]. In nociceptive pain pathways, calcium influx in response to the depolarization of nociceptors facilitates the release of proinflammatory neurotransmitters [19–21]. These neurotransmitters include substance P, glutamate, and calcitonin gene-related peptide (CGRP) [20–22], which are involved in neurogenic inflammation, nociceptor sensitization to painful stimuli, and the development of chronic pain [21]. As a result, the voltage-gated or N-type calcium channel has significant implications for the treatment and management of chronic pain and is a target for therapeutic intervention [11, 20, 21].
In rats, ziconotide has been shown to act on the N-type calcium channel, which tightly governs the transport of calcium across the cellular membrane at the afferent nerve terminal [18, 19, 21, 23]. These channels open in response to membrane depolarization from painful stimuli and are inactivated in nondepolarized states by voltage-dependent and calcium-dependent mechanisms [19–21]. In the open state, N-type calcium channels allow calcium to diffuse down its concentration gradient into the cell where it facilitates the fusion of synaptic vesicles and subsequent release of substance P, glutamate, and CGRP into the synapse of nociceptive afferent nerve terminals in the Rexed laminae I and II of the spinal dorsal horn [19–21, 23, 24]. Here, the neurotransmitters communicate with interneurons carrying afferent signals to the thalamus for interpretation [19, 21]. The N-type calcium channels are important drivers of evoked synaptic transmission and play an important role in nociceptive and neuropathic pain signaling [20, 21]. N-type calcium channels are located in the central and peripheral nervous system including the brain, spinal cord, and primary sensory neurons [19–21, 23]. The channels function at presynaptic, C fiber and A delta afferents in the spinal dorsal horn, and within the cell bodies of the dorsal root ganglia [11, 18, 19, 23]. The role of N-type calcium channel inhibition in pain pathways has been demonstrated genetically in groups of knockout mice that showed reduced pain sensitivity in models of inflammatory and neuropathic pain [11, 19], and this role has been validated clinically by multiple randomized controlled trials demonstrating the efficacy of ziconotide [6–10, 12, 25].
35.2.2.1 Pharmacodynamics and Pharmacokinetics
Ziconotide is polar, hydrophilic, and hypobaric at clinically useful concentrations [25]. It is formulated in 1 or 5 mL vials of 100mcg/mL or 20 mL of 25 mcg/mL aqueous solution diluted in preservative-free normal saline and intended for use with Medtronic SynchroMed II and CADD-Micro ambulatory infusion pumps [11, 25]. Figure 35.3 is a picture from the ziconotide packaging that holds the vials of medication that are used for the pump.


Fig. 35.3
Picture of vials by manufacturer
Ziconotide is marketed by the manufacturer for continuous intrathecal infusion [11]. The initial starting dose for ziconotide infusion is less than or equal to 2.4mcg/day or 0.1mcg/h and may be titrated by less than or equal to 2.4mcg/day or 0.1mcg/h every 2–3 days for a maximum dose of 19.2mcg/day or 0.8mcg/h on day 21 [11]. The slow titration technique described is recommended to limit the development of delayed adverse effects, and faster titrations should be restricted for situations in which urgent analgesia outweighs the risk to patient safety [11].
Ziconotide can have a delayed time of onset of ~8–24 h after initiation of infusion [6–9, 11]. The delayed onset reflects the slow distribution of ziconotide through the cerebral spinal fluid (CSF) and its slow penetration into the CNS parenchyma. Onset time may be hastened by increasing the volume and rate of infusion, which would subsequently increase the intrathecal spread of the medication [6–9, 11, 22]. The volume of distribution approximates the volume of CSF in the body at any given time (~155–260 mL), and ziconotide relies on bulk CSF flow generated by cardiac oscillations for its distribution [11, 22, 25].
The use of an intrathecal drug delivery system greatly limits the uptake of ziconotide from the CSF into the blood stream [11, 17, 22]. Its CSF half-life is 2.9–6.5 h and estimates the daily turnover of CSF [11, 12, 17, 22]. In addition, the size, polarity, and hydrophilicity of ziconotide further limit its efflux through the meninges and into the systemic circulation [22]. Potentially small amounts of medication can efflux out of the CSF through the dural puncture site, but this contribution is considered negligible [22]. Its clearance is described by linear kinetics whether given by bolus or infusion, and its elimination relies on bulk redistribution of CSF to the arachnoid appendages and drainage into the venous circulation [11, 22]. Once in the systemic circulation, ziconotide is cleaved into small peptides and free amino acids by endopeptidases and exopeptidases located in many tissues [11, 12, 22]. Spinal tissue uptake has a minimal contribution to the clearance of ziconotide, and protein binding is negligible in the CSF [22]. Less than 1% is excreted in the urine [12]. Figure 35.4 is a schematic of ziconotide clearance from the CSF following a 1mcg bolus. Estimated CSF concentration of 20 ng/mL and 4.5 h half-life.
Fig. 35.4
Schematic of ziconotide clearance from the CSF following 1mcg bolus. Estimated CSF concentration of 20 ng/mL and 4.5 h half-life [17]
35.2.2.2 Clinical Considerations
Ziconotide monotherapy is indicated for the management of moderate to severe chronic pain in patients for whom IT therapy is warranted, and who are intolerant of or refractory to systemic analgesics and adjunctive therapies, or IT morphine [8, 10–12]. Preclinical and clinical studies, including three randomized controlled trials, have established the efficacy of ziconotide intrathecal infusion for chronic malignant and nonmalignant pain of nociceptive and neuropathic origins [5–9]. Using Visual Analog Scale of Pain Intensity (VASPI) scores as efficacy measures, these RCTs demonstrated significant pain relief over placebo for ~30% of patients treated with ziconotide monotherapy, and a small portion of patients even reported complete pain relief [6–9, 12]. Of note, the early RCTs used higher doses and faster titrations than what is currently used, which led to increased pain relief but a greater incidence of adverse effects and discontinuations from treatment [6–9, 12]. Significant adverse events usually occur within 2–3 days following the initiation of therapy and are thought to reflect the slow pharmacokinetics of the medication [6–8, 11, 12]. The manufacturer recommends a slow titration over a 3-week period, and later studies utilizing the slow titration technique demonstrated a decreased, yet still significant, rate of development of adverse effects and treatment discontinuations when compared to placebo [11, 26]. Interestingly, the abrupt discontinuation of ziconotide intrathecal infusion did not result in drug withdrawal in any of the treatment subjects [6–8, 11, 12].
Despite having many advantages, such as the lack of tolerance or withdrawal, intrathecal ziconotide infusion has a narrow therapeutic window, and adverse effects are common [4, 6–14, 25–27]. Clinical studies have evaluated the use of ziconotide monotherapy in 1254 patients over 7.5 years and demonstrated that adverse effects occur in the CNS in a dose- and rate-related manner and generally resolve within 1–2 weeks after discontinuation of treatment [11, 12]. The most common adverse effects are cerebellar, cognitive, and neuropsychiatric in nature and include dizziness (46%), nausea (40%), asthenia (18%), diarrhea (18%), somnolence (17%), vomiting (16%), and confusion (15%) [11, 12]. These effects are thought to be the result of toxic inhibition of N-type calcium channels throughout the central nervous system, particularly supraspinal structures [12, 22, 23]. In addition to the spinal cord, N-type calcium channels are found in the cerebellum and basal ganglia, and inhibition at these locations is implicated for side effects like dizziness, difficulty walking, nystagmus, and confusion [12, 23]. Ziconotide also has sympatholytic activity and may inhibit central autonomic pathways, explaining the nausea, vomiting, urinary retention, and hypotension also seen in clinical use [12, 24].
35.2.3 Cognitive and Neuropsychiatric Adverse Effects
In clinical trials, confusion was the most common neuropsychiatric effect and occurred most frequently in adults >65 years (47% vs. 29%) [11]. Memory impairment was the second most frequent adverse cognitive effect reported by the manufacturer and was not related to age [11]. Other more adverse neuropsychiatric effects included hallucinations, paranoid reactions, hostility, delirium, psychosis, and mania [11]. Cognitive, psychiatric, and other CNS effects may be delayed and take 1–2 weeks to develop and usually resolve within 2 weeks of discontinuing therapy [10–12, 25]. Ziconotide can be safely discontinued without withdrawal effects [8, 10–12, 25].
The manufacturer warns of the development of severe psychiatric symptoms and neurological impairment during use and advocates patients be monitored frequently for evidence of cognitive impairment, hallucinations, and changes in mood or consciousness. Furthermore, the package insert states Prialt may cause or worsen depression, with the ultimate risk of suicide in susceptible patients [11]. Ziconotide intrathecal infusion is contraindicated in patients with a previous history of psychosis or suicidal ideations or attempts [11]. If serious psychiatric adverse effects occur during drug administration, drug dosages should be adjusted or discontinued and patients instituted on proper psychiatric therapy and/or admitted to an inpatient facility for management [11].
In addition to monitoring for neuropsychiatric adverse effects, patients, caregivers, and healthcare workers must also be diligent about monitoring for potential signs of meningitis, including headache, fever, stiff neck, altered mental status, nausea, vomiting, and seizures [11]. Meningitis was a complication in 3% (40 cases) of treatment subjects in clinical trials and predominantly occurred in patients using external delivery devices (37 cases) [11]. Strict aseptic technique should be used when preparing, placing, or refilling microinfusion delivery devices [11]. If meningitis is suspected, CSF cultures should be obtained, and the patient should be started on appropriate antimicrobial therapy [11]. Typically the drug delivery device is removed along with the intrathecal catheter and all foreign bodies in the intrathecal space [11].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






