Thoracic Paravertebral Block
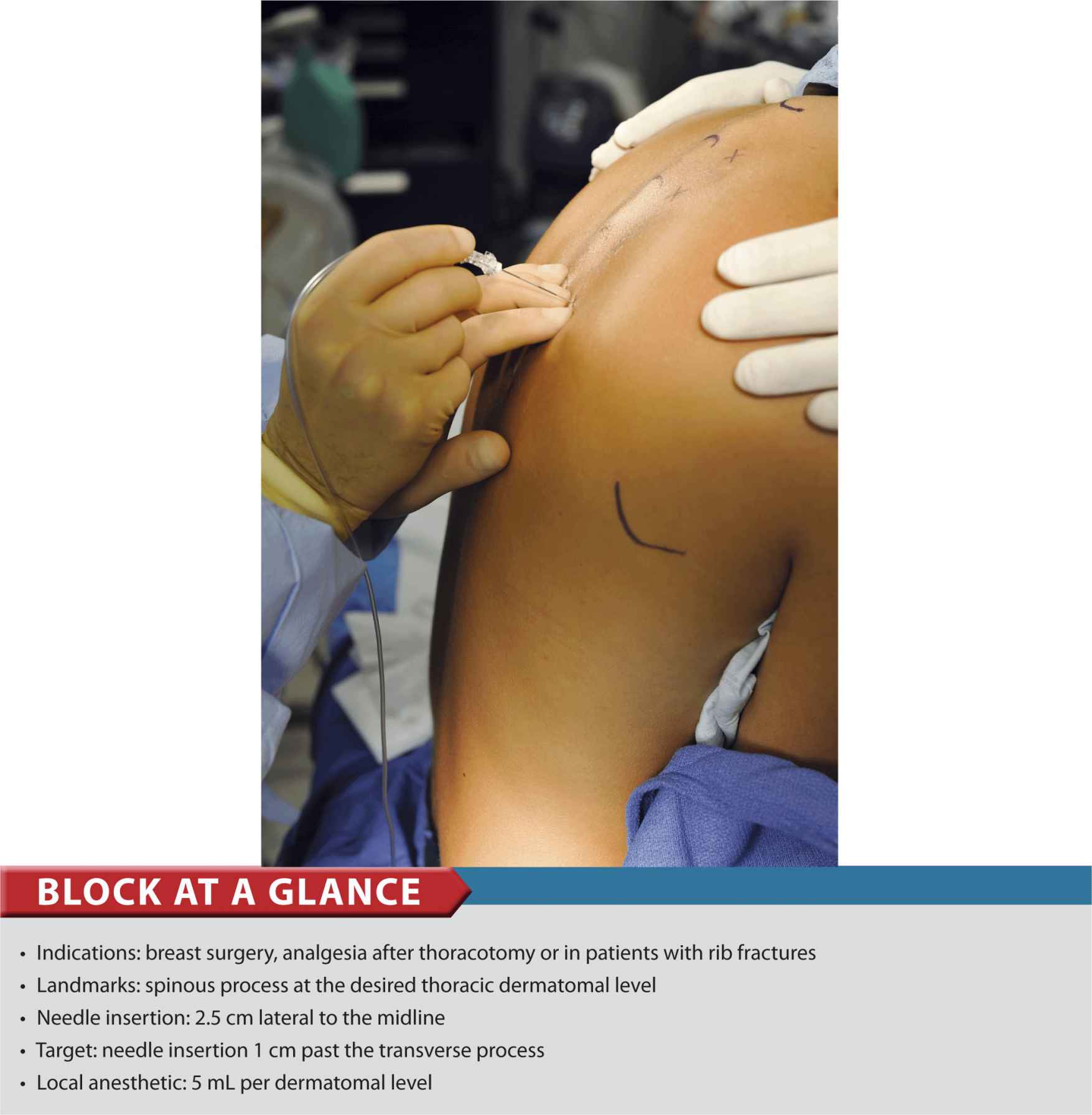
FIGURE 23-1. Thoracic paravertebral block.
General Considerations
A thoracic paravertebral block is a technique where a bolus of local anesthetic is injected in the paravertebral space, in the vicinity of the thoracic spinal nerves following their emergence from the intervertebral foramen. The resulting ipsilateral somatic and sympathetic nerve blockade produces anesthesia or analgesia that is conceptually similar to a “unilateral” epidural anesthetic block. Higher or lower levels can be chosen to accomplish a unilateral, bandlike, segmental blockade at the desired levels without significant hemodynamic changes. For a trained regional anesthesia practitioner, this technique is simple to perform and time efficient; however, it is more challenging to teach because it requires stereotactic thinking and needle maneuvering. A certain “mechanical” mind or sense of geometry is necessary to master it. This block is used most commonly to provide anesthesia and analgesia in patients having mastectomy and cosmetic breast surgery, and to provide analgesia after thoracic surgery or in patients with rib fractures. A catheter can also be inserted for continuous infusion of local anesthetic.
Regional Anesthesia Anatomy
The thoracic paravertebral space is a wedge-shaped area that lies on either side of the vertebral column (Figure 23-2). Its walls are formed by the parietal pleura anterolaterally; the vertebral body, intervertebral disk, and intervertebral foramen medially; and the superior costotransverse ligament posteriorly. After emerging from their respective intervertebral foramina, the thoracic nerve roots divide into dorsal and ventral rami. The dorsal ramus provides innervation to the skin and muscle of the paravertebral region; the ventral ramus continues laterally as the intercostal nerve. The ventral ramus also gives rise to the rami communicantes, which connect the intercostal nerve to the sympathetic chain. The thoracic paravertebral space is continuous with the intercostal space laterally, epidural space medially, and contralateral paravertebral space via the prevertebral fascia. In addition, local anesthetic can also spread longitudinally either cranially or caudally. The mechanism of action of a paravertebral blockade includes direct action of the local anesthetic on the spinal nerve, lateral extension along with the intercostal nerves and medial extension into the epidural space through the intervertebral foramina.
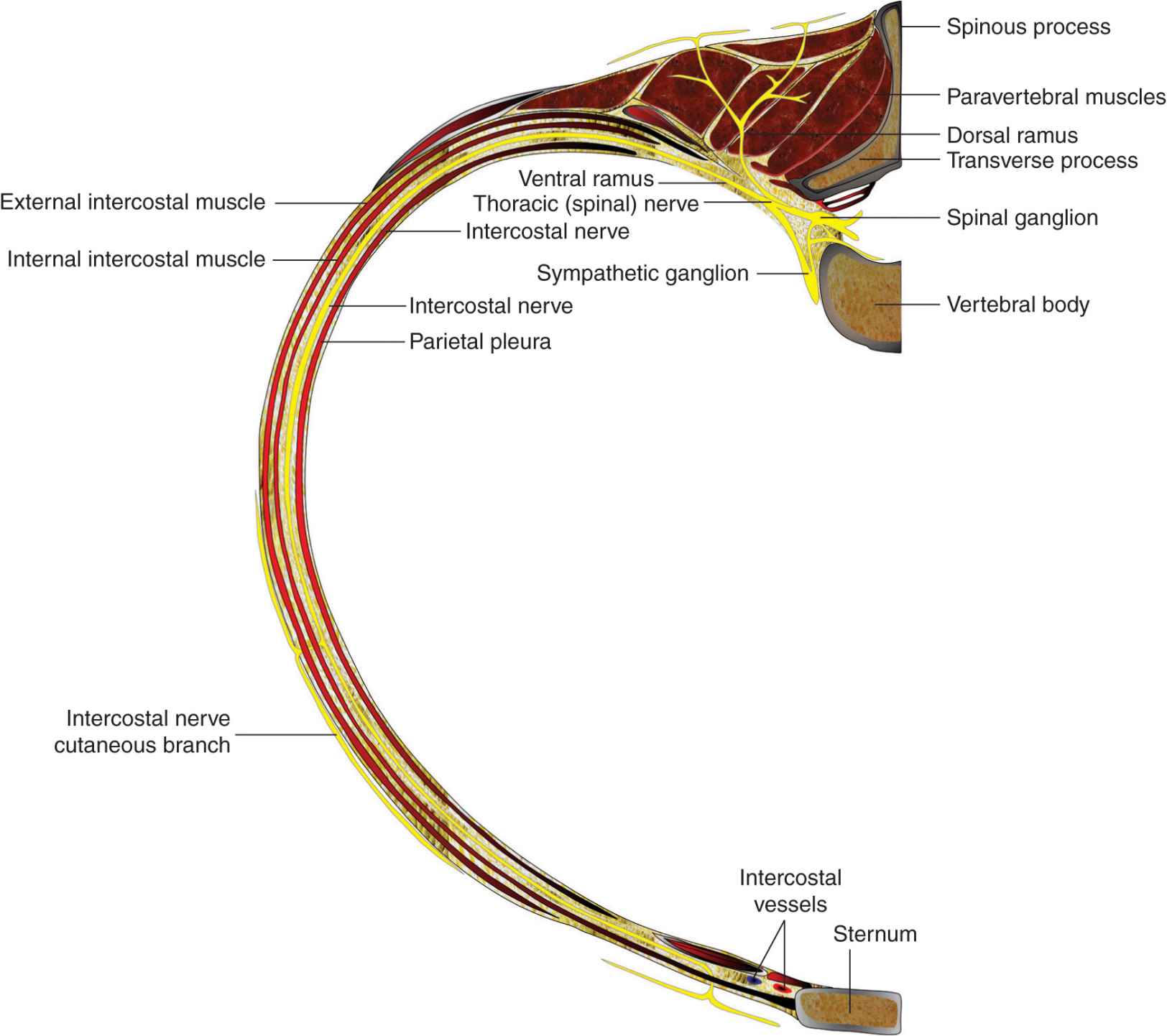
FIGURE 23-2. Anatomy of the thoracic spinal nerve (root) and innervation of the chest wall.
Distribution of Anesthesia
Thoracic paravertebral blockade results in ipsilateral anesthesia. The location of the resulting dermatomal distribution of anesthesia or analgesia is a function of the level blocked and the volume of local anesthetic injected (Figure 23-3).
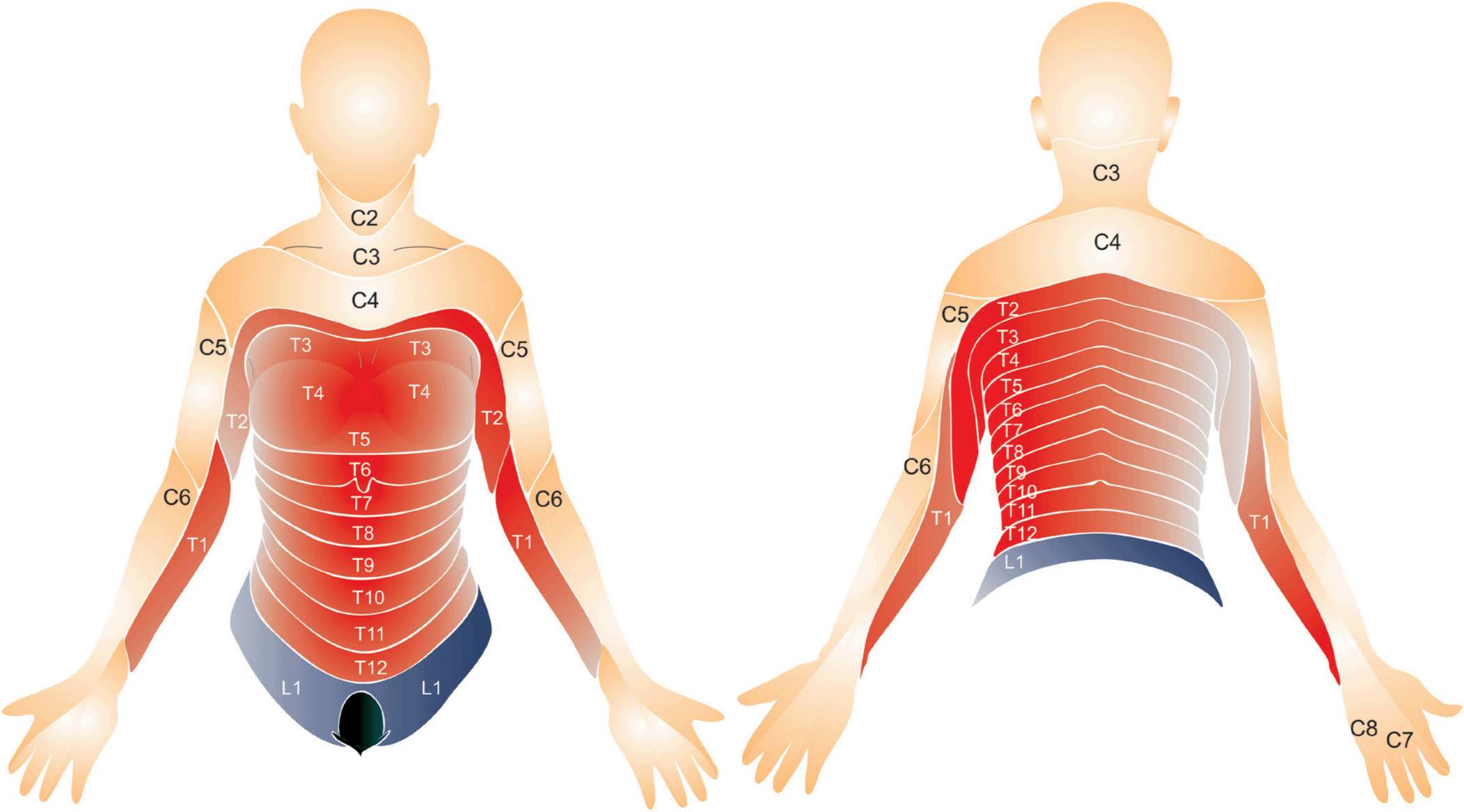
FIGURE 23-3. Thoracic dermatomal levels.
Single-Injection Thoracic Paravertebral Block
Equipment
A standard regional anesthesia tray is prepared with the following equipment:
• Sterile towels and gauze packs
• A 20-mL syringe containing local anesthetic
• Sterile gloves and marking pen
• A 10-mL syringe plus 25-gauge needle with local anesthetic for skin infiltration
• An 8-10 cm, 18-gauge Tuohy tip epidural needle for continuous paravertebral block or an 8-10 cm Quincke tip needle for single injection paravertebral block.
• Low-volume extension tubing
Patient Positioning
The patient is positioned in the sitting or lateral decubitus (with the side to be blocked uppermost) position and supported by an attendant (Figure 23-4). The back should assume knee-chest position, similar to the position required for neuraxial anesthesia. The patient’s feet rest on a stool to allow greater patient comfort and a greater degree of kyphosis. The positioning increases the distance between the adjacent transverse processes and facilitates advancement of the needle between them.

FIGURE 23-4. Patient positioning for thoracic paravertebral block. The patient is positioned in a sitting position with feet resting on a stool and assumes a knee-chest position.
Landmarks and Maneuvers to Accentuate Them
The following anatomic landmarks are used to identify spinal levels and estimate the position of the relevant transverse processes (Figure 23-5):
FIGURE 23-5. Spinal processes are the main landmarks for the thoracic paravertebral block. Processes are outlined from C7 (the most prominent vertebrate) to T7 (tip of scapulae).
1. Spinous processes (midline)
2. Spinous process of C7 (the most prominent spinous process in the cervical region when the neck is flexed)
3. Lower tips of scapulae (corresponds to T7)
The tips of the spinous processes should be marked on the skin. Then a parasagittal line can be measured and drawn 2.5 cm lateral to the midline (Figure 23-6). For breast surgery, the levels to be blocked are T2 through T6. For thoracotomy, estimates can be made after discussion with the surgeon about the planned approach and length of incision.

FIGURE 23-6. The needle insertion points for paravertebral block are labeled 2.5 cm lateral to the spinous processes.
Technique
After cleaning the skin with an antiseptic solution, 6 to 10 mL of dilute local anesthetic is infiltrated subcutaneously along the line where the injections will be made. The injection should be carried out slowly to avoid pain on injection.
The subcutaneous tissues and paravertebral muscles are infiltrated with local anesthetic to decrease the discomfort at the site of needle insertion. The fingers of the palpating hand should straddle the paramedian line and fix the skin to avoid medial-lateral skin movement. The needle is attached to a syringe containing local anesthetic via extension tubing and advanced perpendicularly to the skin at the level of the superior aspect of the corresponding spinous process (Figure 23-7). Constant attention to the depth of needle insertion and the slight medial to lateral needle orientation is critical to avoid pneumothorax and direction of the needle toward the neuraxial space, respectively. The utmost care should be taken to avoid directing the needle medially (risk of epidural or spinal injection). The transverse process is typically contacted at a depth of 3 to 6 cm. If it is not, it is possible the needle tip has missed the transverse processes and passed either too laterally or in between the processes. Osseous contact at shallow depth (e.g., 2 cm) is almost always due to a too lateral needle insertion (ribs). In this case, further advancement could result in too deep insertion and possible pleural puncture. Instead, the needle should be withdrawn and redirected superiorly or inferiorly until contact with the bone is made.

FIGURE 23-7. The technique of thoracic paravertebral block begins with insertion of the needle 2.5 cm lateral to the spinous process with an intention to contact the transverse process.
After the transverse process is contacted, the needle is withdrawn to the skin level and redirected superiorly or inferiorly to “walk off” the transverse process (Figure 23-8A and B). The ultimate goal is to insert the needle to a depth of 1 cm past the transverse process. A certain loss of resistance to needle advancement often can be felt as the needle passes through the superior costotransverse ligament; however, this is a nonspecific sign and should not be relied on for correct placement.
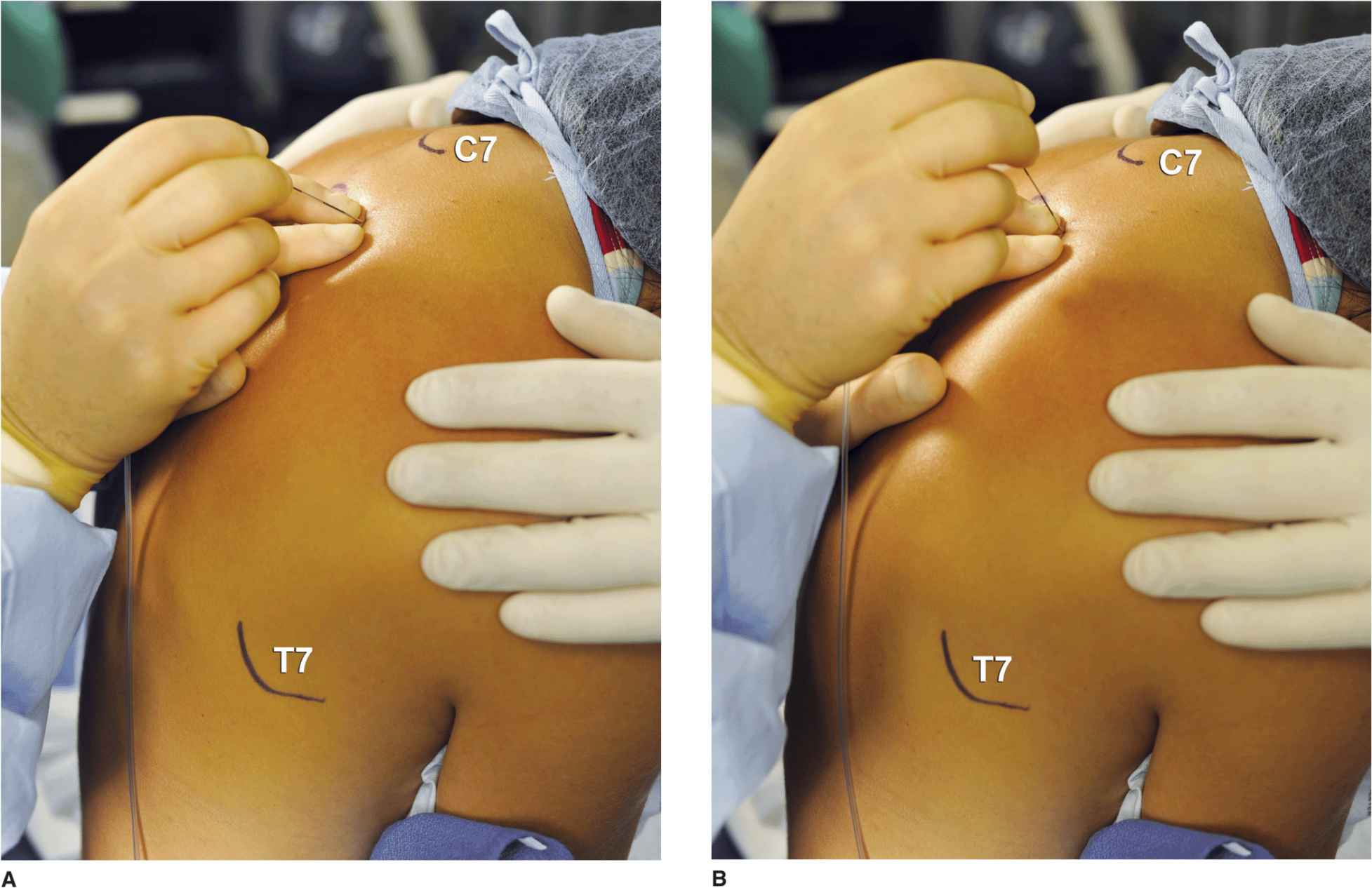
FIGURE 23-8. (A) Once the transverse process is contacted, the needle is walked-off superiorly or inferiorly and advanced 1–1.5 cm past the transverse process. (B) When walking-off the transverse process superiorly proves difficult, the needle is redirected to walk off inferiorly.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








