The Emergency Airway Algorithms
Ron M. Walls
APPROACH TO THE AIRWAY
This chapter presents and discusses the emergency airway algorithms, which we have used, taught, and refined for >15 years. These algorithms are intended to reduce error and improve the pace and quality of decision making for an event that is uncommonly encountered by most practitioners, and often disrupts attempts at sound and orderly clinical management.
When we first set out to try to codify the cognitive aspects of emergency airway management, we were both liberated and impaired by the complete lack of any such algorithms to guide us. In developing The Difficult Airway Course: EmergencyTM, The Difficult Airway Course: AnesthesiaTM, and The Difficult Airway Course: EMSTM, and in applying successively each iteration of the emergency airway algorithms to tens of thousands of real and simulated cases involving thousands of providers, we felt guided by both our continuous learning about optimal airway management and the empirical application of these principles on a large scale. They are based on the best evidence available and the opinions of the most reputable experts in the field of emergency airway management. These algorithms, or adaptations of them, now appear in many of the major emergency medicine textbooks and online references. They are used in airway courses, for residency training, and in didactic teaching sessions, both for in-hospital and out-of-hospital providers. They have stood the test of time and have benefited from constant update.
The revolution in video laryngoscopy has caused us to rethink concepts related to the definition and management of the “difficult airway” (see Chapter 2). This current iteration reflects the broader application of flexible endoscopic methods, which formerly were all flexible fiberoptic scopes, now improved by adoption of complementary metal-oxide semiconductor video, which largely will supplant fiberoptic devices. There are new options with extraglottic devices (EGDs), both with and without intubating capability. Surgical airway management, while still an essential skill, moves from uncommon to rare as the sophistication of rescue devices and techniques increases.
Together, as before, these algorithms comprise a fundamental, reproducible approach to the emergency airway. The purpose is not to provide a “cookbook,” which one could universally and mindlessly apply, but rather to describe a reproducible set of decisions and actions to enhance performance and maximize the opportunities for success, even in difficult or challenging cases.
The specialized algorithms all build from concepts found in the universal emergency airway algorithm, which describes the priority of the key decisions; the determination whether the patient represents a crash airway, a difficult airway, or a failed airway. The algorithms do not attempt to deal with the decision to intubate. This is discussed in Chapter 1. Therefore, the entry point for the emergency airway algorithm is immediately after the decision to intubate has been made.
This iteration of the algorithms introduces a new concept, the “forced to act” situation. There are clinical circumstances in which it is essential to use neuromuscular blocking agents (NMBA) even in the face of an identified difficult airway, simply because there is not sufficient time to attempt any other approach. The operator, forced to act, uses an induction agent and an NMBA to create the best possible circumstances for intubation. In other words, to take the one best chance to secure the airway, and for successful rescue should the primary method fail. An example of this might be the morbidly obese difficult airway patient who prematurely self-extubates in the ICU and is agitated, hypoxic, and deteriorating. Although the patient’s habitus and airway characteristics normally would argue against the use of rapid sequence intubation (RSI), the need to secure the airway within just a few minutes and the patient’s critical deterioration mandate immediate action. By giving an NMBA and induction agent, the operator can optimize conditions for video or direct laryngoscopy, with a plan to either insert a laryngeal mask airway (LMA) or perform a surgical airway if unsuccessful. In some cases, the primary method may be a surgical airway.
The algorithms are intended as guidelines for management of the emergency airway, regardless of the locus of care (emergency department [ED], inpatient unit, operating room, ICU, and out-of-hospital). The goal is to simplify some of the complexities of emergency airway management by defining distinct classes of airway problems. For example, we single out those patients who are essentially dead or near death (i.e., unresponsive, agonal) and manage them using a distinct pathway, the crash airway algorithm. Similarly, a patient with a difficult airway must be
identified and managed according to sound principles. Serious problems can ensue if a NMBA is given to a patient with a difficult airway, unless the difficulty was identified and planned for and the NMBA is part of that planned approach.
identified and managed according to sound principles. Serious problems can ensue if a NMBA is given to a patient with a difficult airway, unless the difficulty was identified and planned for and the NMBA is part of that planned approach.
In human factors analysis, failure to recognize a pattern is often a precursor to medical error. The algorithms aid in pattern recognition by guiding the provider to ask specific questions, such as “Is this a crash airway?” and “Is this a difficult airway?” The answers to these questions group patients with certain characteristics together and each group has a defined series of actions. For example, in the case of a difficult airway, the difficult airway algorithm facilitates formulation of a distinct, but reproducible plan, which is individualized for that particular patient, yet lies within the overall approach that is predefined for all patients in this class, that is, those with difficult airways.
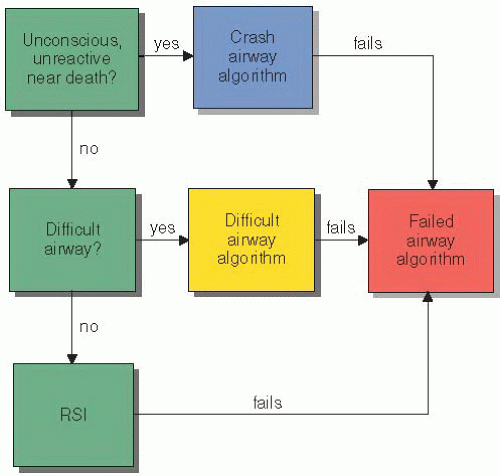
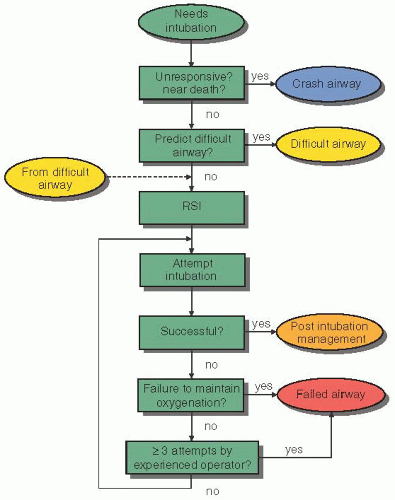
Algorithms are best thought of as a series of key questions and critical actions, with the answer to each question guiding the next critical action. The answers are always binary: “yes” or “no” to simplify and speed cognitive factor analysis. Figures 3-1 and 3-2 provide an overview of the algorithms, and how they work together.
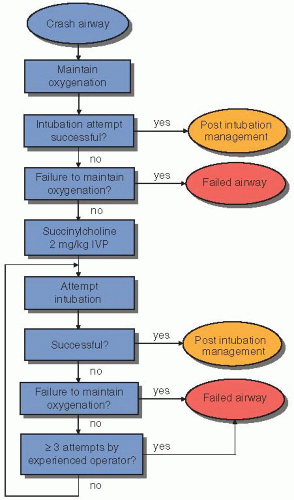
When a patient requires intubation, the first question is “Is this a crash airway?” (i.e., is the patient unconscious, near death, with agonal or no respirations, expected to be unresponsive to the stimulation of laryngoscopy?). If the answer is “yes,” the patient is managed as a crash airway using the crash airway algorithm (Fig. 3-3). If the answer is “no,” the next question is “Is this a difficult airway?” (see Chapter 2). If the answer is “yes,” the patient is managed as a difficult airway (Fig. 3-4). If the answer is “no,” then neither a crash airway nor a difficult airway is present, and RSI is recommended, as described on the main algorithm (Fig. 3-2). Regardless of the algorithm used initially (main, crash, or difficult), if airway failure occurs, the failed airway algorithm (Fig. 3-5) is immediately invoked. The working definition of the failed airway is crucial and is explained in much more detail in the following sections. It has been our experience that airway management errors occur both because the provider does not recognize the situation (e.g., failed airway), and because, although recognizing the situation, he or she does not know what actions to take.
THE MAIN AIRWAY ALGORITHM
The main emergency airway algorithm is shown in Figure 3-2. It begins after the decision to intubate and ends when the airway is secured, whether intubation is achieved directly or through one of the other algorithms. The algorithm is navigated by following defined steps with decisions driven by the answers to a series of key questions:
Key question 1: Is this a crash airway? If the patient presents in an essentially unresponsive state and is deemed to be unlikely to respond to laryngoscopy, then the patient is defined as a crash airway. Here, we are either identifying patients who are in full cardiac or respiratory arrest or those with agonal cardiorespiratory activity (e.g., agonal, ineffective respirations, pulseless idioventricular rhythm). These patients are managed in a manner appropriate for their extremis condition. If a crash airway is identified, exit this main algorithm and begin the crash airway algorithm (Fig. 3-3). Otherwise, continue on the main algorithm.
Key question 2: Is this a difficult airway? If the airway is not identified as a crash airway, the next task is to determine whether it is a difficult airway, which encompasses difficult laryngoscopy and intubation, difficult bag-mask ventilation (BMV), difficult cricothyrotomy, and difficult EGD use. Chapter 2 outlines the assessment of the patient for a potentially difficult airway using the various mnemonics (LEMON, MOANS, RODS, and SMART)
corresponding to these dimensions of difficulty. Difficult video laryngoscopy is sufficiently new and rare that useful predictive parameters have yet to be defined. This is discussed further in Chapter 2. It is understood that virtually all emergency intubations are difficult to some extent. However, the evaluation of the patient for attributes that predict difficult airway management is extremely important. If the patient represents a particularly difficult airway situation, then he or she is managed as a difficult airway, using the difficult airway algorithm (Fig. 3-4), and one would exit the main algorithm. Although it is the LEMON assessment for difficult laryngoscopy and intubation that may be the main driver, evaluation for the other difficulties (BMV, cricothyrotomy, and EGD) also is critical at this point. If the airway is not identified as particularly difficult, continue on the main algorithm to the next step, which is to perform RSI.
Critical action: Perform RSI. In the absence of an identified crash or difficult airway, RSI is the method of choice for managing the emergency airway. RSI is described in detail in Chapter 19 and affords the best opportunity for success with the least likelihood of adverse outcome of any possible airway management method, when applied to appropriately selected
patients. This step assumes that the appropriate sequence of RSI (the seven Ps) will be followed. If the patient is in extreme respiratory distress, or if haste is indicated for any reason, an accelerated or immediate RSI protocol can be used (see Chapter 19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree