Applied Functional Anatomy of the Airway
Michael F. Murphy
There are many salient features of the anatomy and physiology of the airway to consider with respect to airway management maneuvers. This chapter discusses the anatomical features most involved in the act of intubation, the important vascular structures, and the innervation of the upper airway. Chapter 23 builds on these anatomical and functional relationships to describe anesthesia techniques for the airway. Chapter 24 addresses developmental and pediatric anatomical features of the airway.
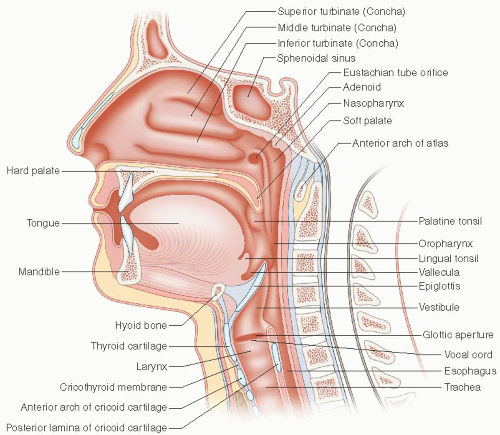
We consider each anatomical structure in the order in which it appears as we enter the airway: the nose, the mouth, the pharynx, the larynx, and the trachea (Fig. 4-1).
THE NOSE
The external nose consists of a bony vault, a cartilaginous vault, and a lobule. The bony vault comprises the nasal bones, the frontal processes of the maxillae, and the nasal spine of the frontal bone. The nasal bones are buttressed in the midline by the perpendicular plate of the ethmoid bone that
forms part of the bony septum. The cartilaginous vault is formed by the upper lateral cartilages that meet the cartilaginous portion of the septum in the midline. The nasal lobule consists of the tip of the nose, the lower lateral cartilages, the fibrofatty alae that form the lateral margins of the nostril, and the columella. The cavities of each nostril are continuous with the nasopharynx posteriorly.
forms part of the bony septum. The cartilaginous vault is formed by the upper lateral cartilages that meet the cartilaginous portion of the septum in the midline. The nasal lobule consists of the tip of the nose, the lower lateral cartilages, the fibrofatty alae that form the lateral margins of the nostril, and the columella. The cavities of each nostril are continuous with the nasopharynx posteriorly.
nose from front to back, the location of the adenoid, the location of the vallecula between the base of the tongue and the epiglottis, and the location of the hyoid bone in relation to the posterior limit of the tongue.
Important Anatomical Considerations
Kiesselbach’s plexus (Little’s area) is a very vascular area located on the anterior aspect of the septum in each nostril. Epistaxis most often originates from this area. During the act of inserting a nasal trumpet or a nasotracheal tube (NTT), it is generally recommended that the device be inserted in the nostril such that the leading edge of the bevel (the pointed tip) is away from the septum. The goal is to minimize the chances of trauma and bleeding from this very vascular area. This means that the device is inserted “upside down” in the left nostril and rotated 180° after the tip has proceeded beyond the cartilaginous septum. Although some authors have recommended the opposite (i.e., that the bevel tip approximate the nasal septum to minimize the risk of damage and bleeding from the turbinates), the bevel away from the septum approach makes more sense and is the recommended method.
The major nasal airway is between the laterally placed inferior turbinate, the septum, and the floor of the nose. The floor of the nose is tilted slightly downward front to back, approximately 10° to 15°. Thus, when a nasal tube, trumpet, or fiberscope is inserted through the nose, it should not be directed upward or even straight back. Instead, it should be directed slightly inferiorly to follow this major channel. Before nasal intubation of an unconscious adult patient, some authorities recommend gently but fully inserting one’s gloved and lubricated little finger to ensure patency and to maximally dilate this channel before the insertion of the nasal tube. In addition, placing the endotracheal tube (ETT; preferably an Endotrol tube) in a warm bottle of saline or water softens the tube and attenuates its damaging properties.
The nasal mucosa is exquisitely sensitive to topically applied vasoconstricting medications such as phenylephrine, epinephrine, oxymetazoline, or cocaine. Cocaine has the added advantage of providing profound topical anesthesia and is the only local anesthetic agent that produces vasoconstriction; the others cause vasodilatation. Shrinking the nasal mucosa with a vasoconstricting agent can increase the caliber of the nasal airway by as much as 50% to 75% and may reduce epistaxis incited by nasotracheal intubation, although there is little evidence to support this claim. Cocaine has been implicated in coronary vasoconstriction when applied to the nasal mucosa, so it should be used with caution in patients with coronary artery disease (see “Evidence” section at the end of this chapter).
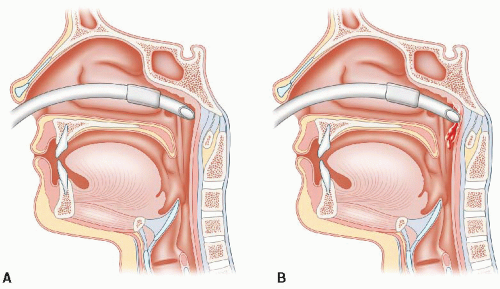
The nasal cavities are bounded posteriorly by the nasopharynx. The adenoids are located posteriorly in the nasopharynx just above the nasal surface of the soft palate and partially surround a depression in the mucosal membrane where the eustachian tube enters the nasopharynx. During insertion, the NTT often enters this depression and resistance is encountered. Continued aggressive insertion can cause the NTT to penetrate the mucosa and pass submucosally deep to the naso- and oropharyngeal mucous membrane (Fig. 4-2). Although alarming when one recognizes that this has occurred, no specific treatment is indicated, except that withdrawing the tube and trying the opposite nostril is advised. Despite the theoretical risk of infection, there is no literature to suggest that this occurs. Documentation of the complication and communication to the accepting team on admission is important.
The soft palate rests on the base of the tongue during quiet nasal respiration, sealing the oral cavity anteriorly.
The contiguity of the paranasal sinuses with the nasal cavity is believed to be responsible for the infections of the paranasal sinuses that may be associated with prolonged nasotracheal intubation. Although this fact has led some physicians to condemn nasotracheal intubation, fear of infection should not deter the emergency physician from considering nasotracheal intubation when indicated. Securing the airway in an emergency takes precedence over possible later infective complications, and in any case, the intubation can always be changed to an oral tube or tracheostomy, if necessary.
A nasotracheal intubation is relatively contraindicated in patients with basal skull fractures (i.e., when the maxilla is fractured away from its attachment to the base of the skull) be cause of the risk of penetration into the cranial vault (usually through the cribriform plate) with the ETT. Careful technique avoids this complication: the cribriform plate is located cephalad of the nares, and tube insertion should be directed slightly caudad (see previous discussion). Maxillary fractures (e.g., LeFort fractures) may disrupt the continuity of the nasal cavities and are a relative contraindication to blind nasal intubation. Again, cautious insertion, especially if guided by a fiberscope, can mitigate the risk.