Testicular and Penile Cancer
John Bisson MD
Carol Green-Hernandez PhD, RN, CS, ANP/FNP
James Tazelaar MS, FNP, RN, CS
Male genital cancers are not uncommon, and because of their location they may be detected at an early stage. It is important that the primary care provider educate men about the importance of regular self-examination of the testicles and penis. Although cancers of the testes and penis are in close physical proximity, their pathogenesis and management differ so greatly that they will be discussed separately.
TESTICULAR CANCER
Primary cancer of the testis accounts for less than 1% of all malignancies (Gilliland & Key, 1995). With the appropriate use of modern diagnostic and treatment techniques, the long-term disease-free survival rate is 90% or better (van Basten et al, 1997).
Anatomy, Physiology, and Pathology
Germ cells are responsible for sperm production and are the site for 95% of the malignant neoplasms of the testes. Germ cells are arranged in a series of tubules, contained within a dense fascial covering called the tunica albuginea. The testis embryologically originates in the genital ridge and descends from the retroperitoneum during fetal development through the abdomen and inguinal canal into the scrotum (Bosl & Motzer, 1997). Extensions of the peritoneum and abdominal wall cover the testes within the scrotum. These layers include the tunica vaginalis, the internal spermatic fascia, the internal and external cremasteric fascia, and finally the dartos muscle and scrotal wall skin. Testicular neoplasms are contained by the tunica albuginea, resulting in fusiform enlargement of the testis, and metastatic spread via the blood and lymphatic supply is into the retroperitoneal nodes. Tumor spread via the scrotal skin and lymphatics into the groin is not seen unless surgery or other interventions have compromised the tumor itself.
Classification of testicular cancer is based on histologic type; this in turn reflects the major treatment options. Because 95% of testicular neoplasms arise from the germ cells, only their pathology and treatment will be discussed; for others, the provider should consult an oncologist. The two main divisions of germ cell tumors are seminoma and nonseminoma, which are additionally divided into embryonal, teratoma, choriocarcinoma, yolk sac, and mixed-cell tumors.
Right-sided tumors are slightly more common than left-sided ones, corresponding to the increased incidence of right cryptorchidism. The incidence of bilateral primary tumors is 1% to 2%. Asynchronous tumor involvement is more common than synchronous. However, on biopsy, approximately 5% of men with testicular cancer have carcinoma in situ in the contralateral testis. Approximately half of these eventually present with cancer. This corresponds to the approximately 2% to 5% cumulative risk of developing cancer in the opposite testicle over the initial 25 years after initial diagnosis (Collis et al, 1996).
The most common germ cell tumors are seminomas, which account for about 50%. These malignancies usually present in men between 30 and 40 years of age. There are three types of seminomas: classic, anaplastic, and spermatocytic. Of these, anaplastic is notable for its high mitotic rate. Spermatocytic seminoma presents late in life and has little metastatic potential.
Between 50% and 60% of germ cell tumors are of the nonseminomatous type. This kind of tumor is most common in men up to age 30. Embryonal carcinoma is the most anaplastic of nonseminomatous tumors and may differentiate into any of the other nonseminomatous types. Choriocarcinoma is the rarest type of nonseminomatous tumor and usually shows up in mixed germ cell tumors.
Mixed germ cell tumors can comprise multiple seminomas and nonseminomas. This type of tumor accounts for close to half of tumors identified. In a mixed tumor, it is important to identify the specific type of tumor cell lines and histologic patterns involved, because treatment effectiveness depends on this information. The most difficult cell line identified dictates the treatment to be used.
Epidemiology
Germ cell cancer of the testis is the most common malignancy in males aged 15 to 35 (Devesa et al, 1995; Buetow, 1995). The incidence varies with race and socioeconomic groups. It is highest in northern Europe and New Zealand, intermediate in the United States, and lowest in Africa and Asia (Adami et al, 1994). The worldwide incidence has increased by more than 100% in the past 40 years (Bosl & Motzer, 1997). It is primarily seen in men of European heritage; in developed countries, the incidence in males of European descent is three times that in males of African descent (Feuer, 1995). Testicular cancer is found more often in developed countries than in developing countries, regardless of race. The peak incidence occurs in men age 20 to 40 years, with secondary rate increases in men older than 60 and boys younger than 10. The latter two elevations in occurrence are specific to individual rare histologic types. Primary testis cancer is the most common solid tumor in men aged 20 to 34, and the second most common in men from that point until age 40.
Higher socioeconomic status is connected with an increased frequency of testicular cancer. The relation between prosperity and testicular cancer remains unclear. Henderson et al (1997) postulated that testicular cancer and cryptorchidism are related to in utero estrogen exposure from hyperemesis gravidarum.
The strongest risk factors for hyperemesis gravidarum are early age at pregnancy, nulliparity, and high body weight of the mother.
The strongest risk factors for hyperemesis gravidarum are early age at pregnancy, nulliparity, and high body weight of the mother.
The primary risk factor for testicular cancer is cryptorchidism. This risk does not appear to be reduced by orchiopexy, although correction of the undescended testicles allows complete palpation. Other factors that appear to increase the risk for testicular cancer are white European heritage, high socioeconomic status, family history, gonadal dysgenesis, fetal exposure to diethylstilbestrol (DES) or oral contraceptives, and a history of orchitis. Lack of descent of the testicles and damage to the testicles appear to be common to all the risk factors listed, but how these link to cancer formation is not clear. Several factors, including orchitis and trauma, may lead to earlier identification of testicular tumors rather than being true risks in and of themselves. No correlations between testicular cancer and nutritional intake or occupational hazards have been established.
Diagnostic Criteria
Testicular cancer is established by pathologic analysis of the testis after inguinal orchiectomy. Diagnosis, staging, and management of malignancies of the testes can be greatly enhanced by the use of tumor markers, discussed below.
DIFFERENTIAL DIAGNOSIS
Torsion, epididymitis, epididymo-orchitis, hydrocele, hernia, hematoma, and spermatocele can in one way or another be confused with testicular cancer. Epididymitis is the most common misdiagnosis. Any solid mass within the testicle should be considered cancer until proven otherwise. If the diagnosis is unclear or examination is hindered by a hydrocele, then ultrasonography should be obtained (Li et al, 1997).
History and Physical Exam
Many, if not most, testicular cancers present with pain or tenderness. The history needs to include assessment of risk factors, including in utero information.
The provider must examine the normal testis first as a baseline. Use the thumb and first two fingers to evaluate the size, consistency, and location of any mass. The scrotal skin should remain normal. In general, any mass within the testis is cancer, and any outside the testis is benign. A hydrocele may be present, making appreciation of a testicular mass more difficult. The abdomen is examined for evidence of retroperitoneal nodal disease; supraclavicular adenopathy suggests advanced disease.
CLINICAL WARNING
Although many, if not most, testicular cancers present with pain, tender gynecomastia may be the only presenting complaint.
Diagnostic Studies
Ultrasound is the single best technique for evaluating testicular pathology and should be performed in all cases of suspected testicular neoplasm. The spread of metastases is predictable, according to the testicle involved. A right testicular tumor tends to metastasize to lymph nodes between the aorta and inferior vena cava. Metastasis from a left testicular tumor tends to spread to nodes lateral to the aorta (Bosl & Motzer, 1997). Computed tomography (CT) of the pelvis and abdomen will show nodal involvement in these areas much of the time. However, microscopic nodal involvement may still be present with negative CT results. Chest x-ray and CT are used when mediastinal or lung metastasis is suspected. The mediastinum is the source of the primary tumor in rare cases. Brain CT is usually reserved for men who show neurologic impairment.
TUMOR MARKERS
Along with imaging, one of the mainstays of testicular tumor testing is serum tumor markers. Many germ cell cancers of the testis produce useful marker materials in three basic types: oncofetal chemicals (alpha-fetoprotein [AFP]), hormonal substances (the beta subunit of human choriogonadotropin [hCG]), and cellular enzymes (lactase dehydrogenase [LDH]). AFP is produced by the least differentiated nonseminomatous tumors (embryonal carcinoma and yolk sac). The beta-hCG level is elevated in several testicular tumors, including choriocarcinoma, seminoma, and nonseminoma. LDH is not specific to any individual or group of tumor types, but an elevation in the LDH level indicates tissue destruction in advanced disease (Bosl & Motzer, 1997). AFP levels are more often increased in embryonal carcinoma.
CLINICAL WARNINGS
Tumor marker elevation is less useful in tumors of mixed germ cell origin, which can include in their mix seminomas, choriocarcinomas, teratomas, embryonal cell carcinomas, and so on.
Serum marker concentrations should be obtained before initiating therapy, after completion of therapy, and regularly during long-term surveillance. The half-life of AFP and beta-hCG is important in assessing the rate of marker decrease after therapy. Therefore, these markers should begin to fall within a week or two with successful treatment; failure to decline suggests persistent disease or metastases. Tumor marker elevation that persists after radical inguinal orchiectomy is highly correlated with pulmonary metastases or metastatic retroperitoneal involvement.
STAGING
Staging is used to define the extent of testicular cancer before initiating treatment. Staging also helps to guide treatment. Staging of the primary cancer is based on the TMN (tumor, metastasis, node) system, using three stages that correspond to the extent of treatment needed and the prognosis.
Treatment Options, Expected Outcomes, and Comprehensive Management
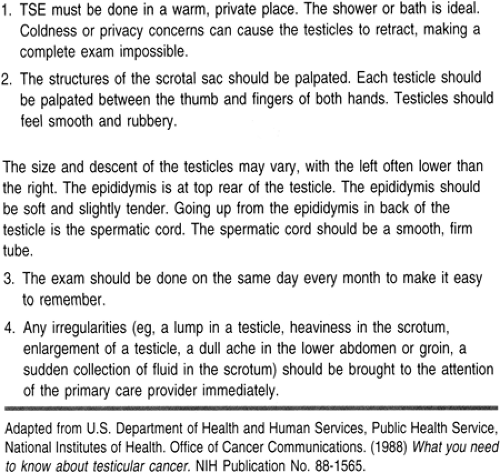
Testicular self-exam (TSE) is the best known form of early detection. Men at risk need to be educated to do TSE on a regular basis, in addition to having the provider perform the exam.
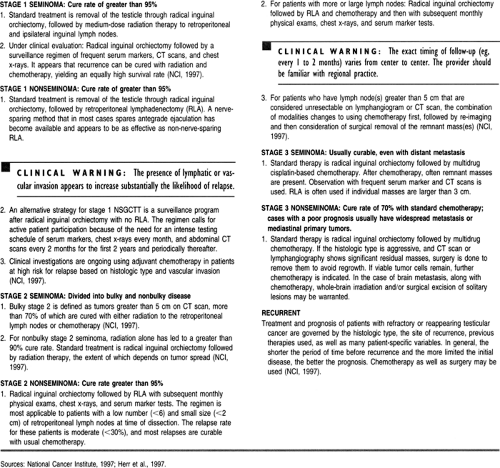
The following testicular cancer treatment options were taken from the National Cancer Institute’s clinician treatment data base (1997). This data base is updated frequently and provides a strong source of current practice standards.
Seminomas are more susceptible to irradiation than nonseminomas. Thus, the treatment of these tumors varies even if they are at the same stage. For this reason, the treatment measures are separated into seminomatous and nonseminomatous sections. In general, mixed tumors are treated as nonseminomatous tumors because these are the more difficult to manage. Patients diagnosed with testicular cancer are referred to a urologist or a uro-oncologist who specializes in the management of this disease. An overview of management is shown in Table 70-1.
Teaching and Self-Care
Rosella (1994) reviewed 11 studies that examined men’s knowledge of risk for testicular cancer, knowledge of TSE, and practice of TSE. The results revealed that most men did not know their risk of testicular cancer or how to perform TSE. Clearly, it is important that the primary care provider teach TSE to all young men at puberty (Table 70-2). Providers should especially target men who are at identified risk for developing testicular cancer.
Monthly TSE has received much attention as a screening method to improve early detection. However, there are no studies showing that TSE leads to earlier identification of testicular carcinomas (Meadus, 1995). Increased surveillance has led to earlier detection of tumors in other at-risk groups (eg, breast cancer, skin cancer). Because most testicular tumors are found by the patient, the more thoroughly prepared a patient is to detect a mass, the more likely he is to succeed. The greatest impediment to tumor identification is the lack of provider teaching of TSE (Rosella, 1994). Because men of this age group often do not seek health care, it is important that the primary care provider take advantage of every opportunity to teach men how to perform TSE.
CLINICAL WARNING
TSE is especially important in patients who have undergone an abdominal orchiectomy for testicular cancer. Potential spread to the other testicle needs to be monitored.
For the patient who has been diagnosed with testicular cancer, the education provided depends on the histologic type of tumor, spread of the tumor, and treatment modalities. These patients are typically young men, and treatment options can cause fertility problems. According to cross-cultural studies, the primary care provider should suggest that the patient consider cryobanking his sperm before beginning treatment (Arai et al, 1997; Botchan et al, 1997). The patient should also be evaluated for fertility and emotional concerns. This need may continue even after successful treatment of testicular cancer; psychological referral may be warranted.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree