Tachycardia with Pulses: Narrow and Wide
Peter J. Kudenchuk
Guesses as to whether a wide-complex tachycardia is ventricular or supraventricular in origin are wrong as often they are right. Differentiating a wide-complex tachycardia that is supraventricular from one of ventricular origin is important because of the differing treatment and prognostic implications for the patient. The most common presumption is that a hemodynamically stable wide-complex tachycardia must be supraventricular (with aberrancy) in origin, whereas the hemodynamic characteristics of an arrhythmia have little to do with its site or origin. Accordingly, the clinician then proceeds to inappropriately treat a true VT with agents meant for SVT, which are not only ineffective but also expose the patient to adverse effects.
Definition and approach to the patient with a tachycardia
Differential diagnosis of narrow-complex tachycardias
Emergency differential diagnosis of wide-complex tachycardias
Initial treatment, including “expert consultation advised”
Overview
Although, convention tachycardia is defined as a heart rate ≥100 bpm, abnormal tachycardias are somewhat arbitrarily defined by a resting rate of >120 bpm. It should be recognized, however, that a normal rhythm (sinus tachycardia) may reach or exceed this resting rate under some conditions.
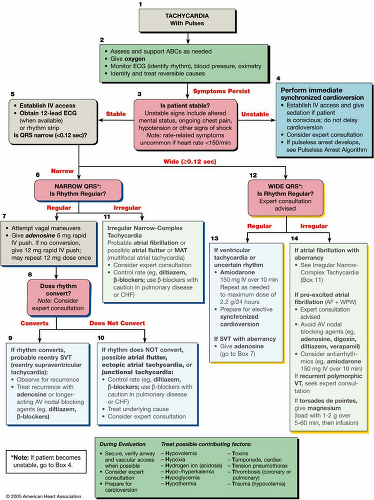
Therefore, in light of the appearance and clinical circumstances surrounding the rhythm and rate, the provider must initially ascertain whether an abnormal tachycardia is actually present. Is it a real tachyarrhythmia? (Fig. 22-1, Box 1.) If the rate and appearance of the tachycardia suggest that it truly represents an arrhythmia (rather than a normal rhythm at a faster rate, or an artifactual arrhythmia), the initial approach to its characterization is to assess the patient and determine if serious symptoms are present and due to the tachycardia (Fig. 22-1, Box 2). If serious or significant symptoms are present, then is the patient hemodynamically stable (Fig. 22-1, Box 3)? Unstable signs include altered mental status, ongoing chest pain, hypotension, or other signs of tissue hypoperfusion. A hemodynamically unstable tachycardia prompts the need for rapid intervention with electrical cardioversion, whereas a hemodynamically stable tachycardia can be approached more deliberately with attention to the most probable rhythm diagnosis and treatment, targeted at its likely origin and mechanism. Or such a patient can potentially be transported to a facility more capable of diagnosing the rhythm.
Initial Steps in Assessing the 12-Lead Electrocardiogram
Is the QRS complex narrow or wide (≥0.12 seconds)?
Is the ventricular rate regular or irregularly irregular?
Are the QRS complexes preceded by P waves in a 1:1 fashion?
Are PR intervals (when seen) constant or variable?
The next steps in the evaluation of the patient with arrhythmia are to characterize the tachycardia as being wide (QRS ≥0.12 seconds) or narrow in appearance (Fig. 22-1, Boxes 6 and 12); whether it is regular or irregularly irregular in rate (Fig. 22-1 stratification of rhythms shown below Boxes 6 and 12); and whether there is a 1:1 correspondence between each P wave and QRS complex. Finally, determining whether the PR intervals (when seen) are constant or variable can be helpful in determining whether P waves are being conducted to QRS complexes or are more randomly associated with them.
Obtaining a 12-lead ECG of the tachycardia is crucial. A rhythm obtained from a single lead (in which a portion of the QRS complex may be isoelectric and
appear flat on the baseline) can mislead providers into thinking a tachycardia is narrow and presumably of supraventricular origin, when seeing the same rhythm in other leads indicates QRS complexes are actually wide.
appear flat on the baseline) can mislead providers into thinking a tachycardia is narrow and presumably of supraventricular origin, when seeing the same rhythm in other leads indicates QRS complexes are actually wide.
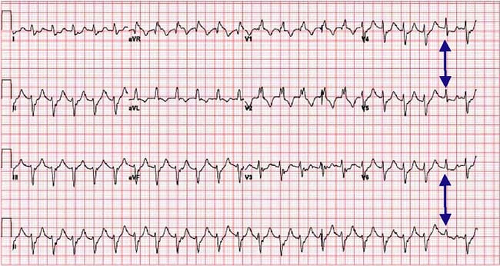
If the patient is stable, obtaining a 12-lead ECG of the tachycardia is crucial. A rhythm obtained from a single lead (in which a portion of the QRS complex may be isoelectric and appear flat on the baseline) can mislead providers into thinking a tachycardia is narrow and presumably of supraventricular origin, when seeing the same rhythm in other leads indicates QRS complexes are actually wide.
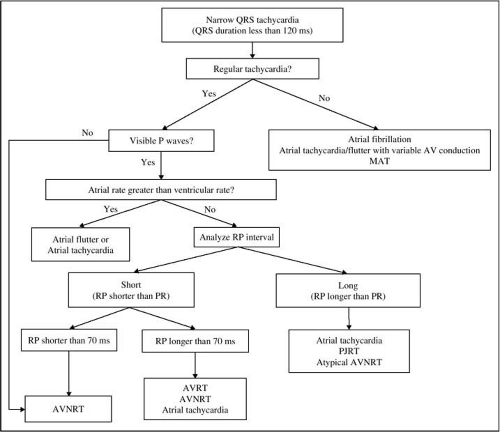
Narrow-Complex Tachycardias
A narrow-complex tachycardia (<120 milliseconds and especially if <110 milliseconds in duration) can almost always be considered to be of supraventricular origin. The rare exception is a form of ventricular tachycardia (called fascicular tachycardia), which involves one of the fascicles of the His-Purkinje system of the ventricle, and appears relatively narrow (110–120 milliseconds) because it utilizes a portion of the His-Purkinje system for conduction, even though it actually originates in the ventricle. Narrow-complex (supraventricular) tachycardias can be subdivided by whether they are regular or irregular and by their mechanism (whether due to increased automaticity or reentry) (Fig. 22-2); see below. The differential diagnosis of the supraventricular tachycardia (SVT) includes sinus tachycardia; sinus node reentry tachycardia; paroxysmal supraventricular tachycardia (PSVT) due to atrioventricular nodal reentry (AVNRT) or atrioventricular reentry utilizing an accessory pathway as the retrograde limb of the reentry circuit (AVRT); ectopic (focal) atrial tachycardia; multifocal atrial tachycardia; intra-atrial reentry tachycardia, atrial fibrillation, and atrial flutter. The features and treatment approaches to these arrhythmias are discussed for each specific entity in the section below. In general, treatment of these arrhythmias, if the patient is hemodynamically stable, is approached by use of drugs that block the AV node and result in slower ventricular rates or result in termination of the arrhythmia by creating AV nodal block. The exception to this generality is when one is dealing with an arrhythmia such
as atrial tachycardia, atrial flutter, or atrial fibrillation that conducts to the ventricles via an accessory pathway (the clue to whose presence is the appearance of a wide QRS complex when conduction to the ventricle occurs over the accessory pathway). In this instance, slowing the ventricular rate requires treatment that is directed at the accessory pathway itself.
as atrial tachycardia, atrial flutter, or atrial fibrillation that conducts to the ventricles via an accessory pathway (the clue to whose presence is the appearance of a wide QRS complex when conduction to the ventricle occurs over the accessory pathway). In this instance, slowing the ventricular rate requires treatment that is directed at the accessory pathway itself.
Differential Diagnosis of Narrow-Complex (Supraventricular) Tachycardias (SVT)
| Rhythm | Mechanism |
|---|---|
| Sinus tachycardia Sinus node reentry tachycardia Paroxysmal supraventricular tachycardia (PSVT) – Atrioventricular nodal reentry tachycardia (AVNRT) – Atrioventricular reentry tachycardia (AVRT) Ectopic (focal) atrial tachycardia (EAT) Multifocal atrial tachycardia (MAT) Junctional tachycardia Intra-atrial reentry tachycardia Atrial fibrillation (AF) Atrial flutter | Increased sinus node automaticity Reentry within the sinus node Reentry within or surrounding the AV node Reentry involving an accessory pathway Increased automaticity of an atrial focus Increased automaticity of many atrial foci Increased automaticity of the AV node Reentry within the atria Multiple reentry circuits within the atria Reentry circuit typically within the right atrium |
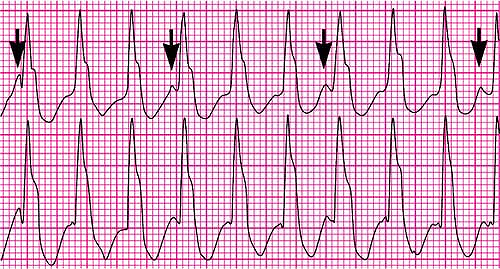
Irregular Narrow-Complex Tachycardias
Narrow-complex tachycardias that are irregularly irregular most commonly represent atrial fibrillation. Atrial fibrillation is defined as an irregularly irregular rhythm without definite P waves. Instead there is a continuous undulation of the baseline between QRS complexes of variable amplitude and contour representing atrial fibrillation waves (Fig. 22-3). The exception to this rule is multifocal atrial tachycardia. Multifocal atrial tachycardia (MAT) is defined as an irregularly irregular tachycardia with distinct P waves of at least three differing morphologies preceding each QRS. The atrial rate may range from 100 to 250 beats/minute. Conduction to the ventricle may be 1:1 as in Fig. 22-4, or variable, in which case each blocked P wave is separated by an isoelectric interval from the next (distinguishing it from atrial fibrillation or flutter where there is no isoelectric interval between successive fibrillation or flutter waves).
In multifocal atrial tachycardia, each blocked P wave is separated by an isoelectric interval from the next. This differential point distinguishes MAT from atrial fibrillation or flutter where there is no isoelectric interval between successive fibrillation or flutter waves.
Regular Narrow-Complex Tachycardias
Regular narrow-complex tachycardias include automatic rhythms, such as sinus tachycardia, junctional tachycardia, and ectopic atrial tachycardia, and reentry rhythms, such as reentrant PSVTs, sinus node reentry tachycardia, intra-atrial reentry tachycardia, and atrial flutter (when conducted with a fixed degree of block). Reentry arrhythmias are distinguished from automatic rhythms by their abrupt onset and termination and their relatively fixed rate, whereas automatic rhythms are characterized by a more gradual “warm up” in rate at their onset.
Reentry Arrhythmias
Reentry arrhythmias (see Chapter 20 for description of mechanisms) typically have an abrupt onset, because once a reentry circuit is activated by a premature complex, the rate of the tachycardia is determined by the conduction properties of the
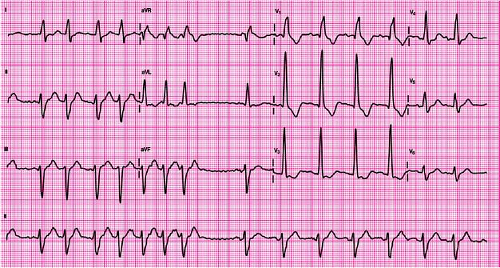
circuit itself, which are relatively constant. Hence the heart rate rapidly increases, becoming steady within a few beats of onset. The term “paroxysmal supraventricular tachycardia” (PSVT), as commonly used, implies a rapid onset of a supraventricular arrhythmia at a regular rate, suggesting a reentry mechanism, usually without easily discernible P waves (although they may be identifiable when not completely hidden within QRS complexes upon closer inspection). The various PSVTs include atrioventricular nodal reentry (AVNRT) and atrioventricular reentry using an accessory pathway (AVRT). These arrhythmias are typically triggered by a premature atrial complex, followed by a rapid, regular tachycardia often without discernible P waves (Fig. 22-5).
circuit itself, which are relatively constant. Hence the heart rate rapidly increases, becoming steady within a few beats of onset. The term “paroxysmal supraventricular tachycardia” (PSVT), as commonly used, implies a rapid onset of a supraventricular arrhythmia at a regular rate, suggesting a reentry mechanism, usually without easily discernible P waves (although they may be identifiable when not completely hidden within QRS complexes upon closer inspection). The various PSVTs include atrioventricular nodal reentry (AVNRT) and atrioventricular reentry using an accessory pathway (AVRT). These arrhythmias are typically triggered by a premature atrial complex, followed by a rapid, regular tachycardia often without discernible P waves (Fig. 22-5).
Other regular narrow-complex tachycardias caused by reentry include atrial flutter (due to a reentry circuit in the right atrium), intra-atrial reentry tachycardia (analogous to atrial flutter, but using a different reentry circuit within the atria and often presenting at a different rate than typical atrial flutter), and sinus node reentry tachycardia (where the reentry circuit occurs within the sinus node). Atrial flutter is defined as an atrial arrhythmia with a “sawtooth” appearance (without an isoelectric period between successive flutter waves) (Fig. 22-6). Typically, the atrial rate in flutter is 300 per minute, with a 2:1 AV block, resulting in a regular ventricular rate of 150 per minute. However, both the atrial rate and degree of AV block can vary and atrial flutter can present with varying ventricular rates (an irregular tachycardia).
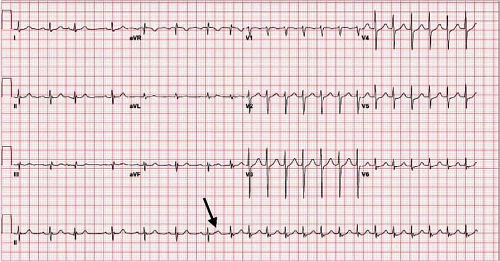 Figure 22-5 • PSVT. Sinus rhythm is followed by a premature atrial impulse (arrow) that is hidden in the T wave, followed by a longer than usual PR interval, representing conduction down a more slowly conducting pathway to the ventricle (see Chapter 20). This is immediately followed by a regular narrow-complex tachycardia at a fixed rate without discernible P waves. |
Automatic Rhythms
In contrast, automatic rhythms (that is, those due to enhanced automaticity, not reentry) typically begin with a more gradual warm-up or gradual acceleration of rate and may terminate the same way, similar to the behavior of sinus rhythm (an automatic rhythm) before, during, and upon completion of exercise. Automatic rhythms include sinus
tachycardia, ectopic atrial tachycardia (Fig. 22-7), and junctional tachycardia (Fig. 22-8). Junctional tachycardia is a rare arrhythmia in adults and is most commonly confused with PSVT or sinus tachycardia with first-degree AV block (in which the P wave is not discernible because of its fusion with the preceding T wave). Retrograde (inverted) P waves may be visible in junctional tachycardia just preceding or following each QRS, but they may also be hidden from view within the QRS. When seen in adults, junctional tachycardia may be associated with the administration of catecholamine drugs (such as dopamine), which excite a junctional pacemaker focus and result in its more rapid firing.
tachycardia, ectopic atrial tachycardia (Fig. 22-7), and junctional tachycardia (Fig. 22-8). Junctional tachycardia is a rare arrhythmia in adults and is most commonly confused with PSVT or sinus tachycardia with first-degree AV block (in which the P wave is not discernible because of its fusion with the preceding T wave). Retrograde (inverted) P waves may be visible in junctional tachycardia just preceding or following each QRS, but they may also be hidden from view within the QRS. When seen in adults, junctional tachycardia may be associated with the administration of catecholamine drugs (such as dopamine), which excite a junctional pacemaker focus and result in its more rapid firing.
Clues to the Diagnosis of Narrow-Complex Tachycardias
Figure 22-2 provides a useful approach to the diagnosis of supraventricular tachycardias, which can be based on a number of serially asked questions:
How does the tachycardia begin? Capture of the actual onset of the tachycardia can provide a particularly valuable clue as to its mechanism. Reentry tachycardias typically begin abruptly (with a premature complex), whereas automatic tachycardias more commonly accelerate to their peak rate gradually.
Is the tachycardia irregularly irregular? Irregularly irregular supraventricular tachycardias include (most commonly) atrial fibrillation, atrial flutter (when there is variable atrioventricular block), and multifocal atrial tachycardia.
If the tachycardia is regular, are P waves visible? In AVNRT, where the reentry circuit “spins” within the AV node, retrograde P waves that are “spun off” to the atrium during the tachycardia are typically hidden within the QRS complex and not discernible on the surface ECG.
If P waves are visible, is their rate faster than the ventricular rate? If so, the likely diagnosis is atrial flutter or an atrial tachycardia.
What is the character of the RP interval? The R-to-P (or RP) interval is defined as the time between the QRS complex and the next visible P wave (or the converse of the PR interval) and usually refers to the timing of the retrograde P wave resulting from a reentry tachycardia (but it can also refer to atrial or junctional rhythms, as discussed below).
A “short-RP tachycardia” refers to a state in which the RP interval is less than half of the interval between successive QRS complexes (RR interval). That is, the P wave falls closer to the preceding QRS than to the QRS trailing it. Conversely, a “long-RP tachycardia” refers to a state in which the RP interval exceeds half of the interval between successive QRS complexes. That is, the P wave falls closer to the trailing QRS than to the preceding one.
A short RP tachycardia with an extremely short RP interval (<70 milliseconds) means the retrograde P wave is either buried within the QRS complex (and not seen) or might be seen to just coincide with the onset or offset of the QRS. If due to reentry, this is diagnostic of AVNRT. When the RP interval is somewhat longer but still relatively short (>70 milliseconds), this implies that the reentry circuit takes longer to spin off P waves back to the atrium. This could implicate retrograde P waves generated from AVNRT (with slower than normal conduction of the retrograde P wave back to the atrium) or from AVRT (which typically takes longer to generate a retrograde P wave because the reentry circuit requires that the impulse traverse the ventricles and accessory pathway before being spun back to the atrium).
Conversely, long-RP tachycardias can represent an atypical form of reentry (either the uncommon form of AVNRT or a slowly conducting accessory pathway, including an unusual accessory pathway–mediated arrhythmia called PJRT (permanent form of junctional reciprocating tachycardia). The longer R-to-P interval in these instances results from slower retrograde conduction back to the atrium.
Short- and long-RP tachycardia can also result from automatic (rather than reentrant) arrhythmias, such as atrial tachycardia. For example, an atrial tachycardia with relatively brisk AV conduction might have the appearance of a long-RP tachycardia; whereas an atrial tachycardia with a rate-related first-degree AV block might have the appearance of a short-RP tachycardia.
Finally, in the case of automatic junctional rhythms, retrograde P waves may just slightly precede, be hidden within, or immediately follow the QRS complex, depending upon the speed of retrograde conduction from the AV node back to the atria. When retrograde conduction is more rapid than anterograde conduction, the retrograde P wave may just slightly precede the QRS; when retrograde conduction occurs as rapidly as antegrade conduction to the ventricle, the retrograde P wave will be nearly simultaneous with and hidden within the QRS; whereas when retrograde conduction is slower than antegrade conduction, the retrograde P wave will trail the QRS.
In summary, the relationship of the P wave to the preceding and trailing QRS complex can provide a differential diagnosis for the arrhythmia; in concert with the behavior and other characteristics of the arrhythmia, this may help to establish its diagnosis. The differential diagnosis of a short-RP tachycardia includes reentry arrhythmias (AVNRT or AVRT), atrial tachycardia with first-degree AV block, or junctional rhythms. The differential diagnosis of a long-RP tachycardia includes the uncommon form of AVNRT, or AVRT with a slowly conducting accessory pathway (PJRT), atrial tachycardia, or junctional rhythms.
An additional question to ask that is not addressed in the algorithm shown in Figure 22-2 is: What is the configuration
(appearance) of the P wave? A P wave that appears identical to a sinus P wave suggests that the rhythm is sinus tachycardia or possibly sinus node reentry tachycardia. A retrograde P wave may be inverted in leads that would normally see an upright sinus P wave. And the P wave from an ectopic atrial focus will have a different configuration than a sinus P wave. Although a P wave that is clearly different in appearance from a sinus P wave implies that the rhythm is not of sinus origin, the converse is not true. P waves may appear sinus-like but still originate from an ectopic arrhythmia focus lying near the sinus node or even posterior to it (in the left atrium).
(appearance) of the P wave? A P wave that appears identical to a sinus P wave suggests that the rhythm is sinus tachycardia or possibly sinus node reentry tachycardia. A retrograde P wave may be inverted in leads that would normally see an upright sinus P wave. And the P wave from an ectopic atrial focus will have a different configuration than a sinus P wave. Although a P wave that is clearly different in appearance from a sinus P wave implies that the rhythm is not of sinus origin, the converse is not true. P waves may appear sinus-like but still originate from an ectopic arrhythmia focus lying near the sinus node or even posterior to it (in the left atrium).
As evidenced by the growing complexity of possibilities from these series of questions, rhythm diagnosis is likely to require expert consultation if such a diagnosis has not been made by the time the care providers arrives at question 5.
Wide-Complex Tachycardias
In describing tachycardias with a prolonged QRS duration, “wide” is the common term in the United States, whereas in the United Kingdom “broad” is frequently used. Such rhythms are formally defined by a QRS >120 milliseconds, although many experts would also regard a QRS of 120 milliseconds as wide. Wide- or broad-complex tachycardias present a diagnostic challenge because, in addition to being possibly due to ventricular tachycardia, they can be caused by any supraventricular arrhythmia with aberrant conduction. Aberrant conduction means that one or more of the His–Purkinje pathways normally responsible for depolarizing the ventricles failed to conduct the impulse, resulting in depolarization of that region of the ventricle by slower muscle-to-muscle conduction. Such a failure of conduction may be transient (due to the rapid rate of the tachycardia), or permanent (due to a preexisting conduction abnormality). The longer time required to depolarize the ventricle as a result of this interruption in the His–Purkinje system is expressed by a QRS complex of longer (wider) duration. In addition, conduction to the ventricle via an accessory pathway (see discussion of preexcitation in Chapter 19) will result in a wide QRS because of the direct insertion of the pathway into ventricular muscle outside the His–Purkinje system. A narrow-complex tachycardia can be said in most instances to be of supraventricular origin; virtually any arrhythmia can present as a wide-complex tachycardia.
Aberrant conduction means that one or more of the His–Purkinje pathways normally responsible for depolarizing the ventricles fails to conduct the impulse, resulting in depolarization of that region of the ventricle by slower muscle-to-muscle conduction. A narrow-complex tachycardia can be said, in most instances, to be of supraventricular origin, but virtually any arrhythmia can present as a wide-complex tachycardia.
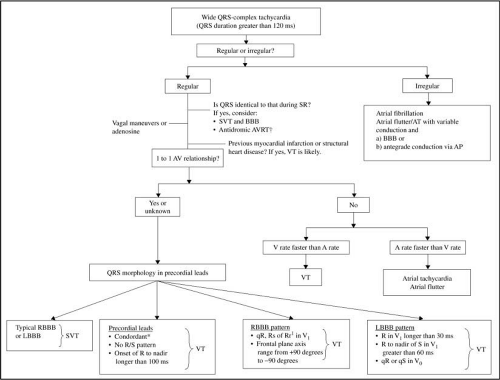
Differentiating a wide-complex tachycardia (Fig. 22-9) that is supraventricular from one of ventricular origin is important because of the differing treatment and prognostic implications for the patient. Guesses as to whether a wide-complex tachycardia is ventricular or supraventricular in origin are wrong as often they are right. The most common presumption is that a hemodynamically stable wide-complex tachycardia must be supraventricular (with aberrancy) in origin, whereas the hemodynamic characteristics of an arrhythmia have little to do with its site or origin. Accordingly, the clinician then proceeds to treat a true VT inappropriately with agents meant for SVT, which are not only ineffective but also expose the patient to adverse effects.2,3
Clinical Clues
Clues about the origin of the arrhythmia may be provided with some knowledge of the patient. Older patients with known structural heart disease are at higher risk for ventricular arrhythmias than younger patients without known heart disease, although both groups can have supraventricular arrhythmias. Thus a wide-complex tachycardia is more likely to represent ventricular tachycardia in an older patient with known heart disease than in a younger, healthy patient. A history of previous supraventricular tachycardia, known accessory pathway, preexisting bundle-branch block, or known rate-dependent bundle-branch blocks also suggests that a wide-complex tachycardia is more likely to be of supraventricular origin (with aberrancy) than of ventricular origin. When the QRS during a wide-complex tachycardia matches the QRS observed on a prior ECG obtained during sinus rhythm, this is further support to the arrhythmia being of supraventricular origin.
Clinical Clues—Differential Diagnosis of Wide-Complex Tachycardia (WCT)
Supports Diagnosis of WCT
Older patient with known structural heart disease.
Symptoms of acute ischemia/infarction.
Supports Diagnosis of SVT with Aberrancy
Young patient without structural heart disease.
Prior existing bundle-branch block and the appearance of QRS complex matches previous ECG.
History of SVT with aberrancy or known accessory pathway.
ECG Clues and Exceptions
The opportunity to establish a rhythm diagnosis is optimal when the patient is hemodynamically stable and the arrhythmia is ongoing. If possible, a 12-lead ECG should be obtained. Either the ECG or, if unavailable, the rhythm strip tracing should be carefully scrutinized for P waves that are slower in rate and dissociated (fewer in number) from the wide QRS complexes (Fig. 22-10) as this is arguably the most reliable evidence that an arrhythmia represents ventricular tachycardia. This is referred to as atrioventricular (AV) dissociation. Unfortunately, P waves can be challenging to identify amid a tachycardia because of their low amplitude relative to the size of QRS complexes, in which they can easily be hidden from view. Other ECG clues suggesting that a wide-complex tachycardia is due to VT include the presence of fusion and/or capture QRS complexes amid the wide-complex tachycardia. These result when an occasional sinus impulse is successfully
conducted across the AV node simultaneously with the tachycardia, resulting in “capture” of the ventricle by the supraventricular impulse. Were this event to occur between successive beats of the tachycardia, a narrow-complex (supraventricular) QRS may be seen amid the otherwise wide-complex tachycardia. Were this event to instead be superimposed on a VT complex, the resulting morphology would be intermediate between a narrow supraventricular and wide-complex VT beat, of a “fusion” of the two complexes (sometimes called a “Dressler” complex). While the occasional presence of either such fusion or capture complexes suggests that the underlying wide-complex rhythm is VT (see Fig. 22-13), unfortunately, this rule is not foolproof. Its notable exception occurs in patients with an accessory pathway (see discussion in Chapter 19). When such patients develop an atrial arrhythmia (such as atrial fibrillation), conduction to the ventricle may occur variably down the accessory pathway (resulting in a wide QRS), down the AV node (resulting in a narrow QRS), or both (resulting in complexes that combine some of both appearances). This can result in a mixture of wide, narrow and intermediate duration QRS complexes on the ECG due to a supraventricular arrhythmia, not ventricular tachycardia. This principle is illustrated in Figure 19-2 and exemplified in Figure 22-15.
conducted across the AV node simultaneously with the tachycardia, resulting in “capture” of the ventricle by the supraventricular impulse. Were this event to occur between successive beats of the tachycardia, a narrow-complex (supraventricular) QRS may be seen amid the otherwise wide-complex tachycardia. Were this event to instead be superimposed on a VT complex, the resulting morphology would be intermediate between a narrow supraventricular and wide-complex VT beat, of a “fusion” of the two complexes (sometimes called a “Dressler” complex). While the occasional presence of either such fusion or capture complexes suggests that the underlying wide-complex rhythm is VT (see Fig. 22-13), unfortunately, this rule is not foolproof. Its notable exception occurs in patients with an accessory pathway (see discussion in Chapter 19). When such patients develop an atrial arrhythmia (such as atrial fibrillation), conduction to the ventricle may occur variably down the accessory pathway (resulting in a wide QRS), down the AV node (resulting in a narrow QRS), or both (resulting in complexes that combine some of both appearances). This can result in a mixture of wide, narrow and intermediate duration QRS complexes on the ECG due to a supraventricular arrhythmia, not ventricular tachycardia. This principle is illustrated in Figure 19-2 and exemplified in Figure 22-15.
If available, the detailed characterization of QRS configuration on the 12-lead ECG may be helpful in differentiating SVT from VT, but accuracy requires experience.4,5,6,7,8 Complex rules exist for making the correct rhythm diagnosis by QRS morphology alone, as depicted in Figure 22-9. These morphology rules, however, are difficult to teach, learn, remember, and reproducibly apply; they are applicable only when a
12-lead ECG has been obtained.9,10,11,12,13 Moreover, morphologic QRS criteria are less accurate in patients who have a preexisting QRS conduction abnormality, particularly if they are taking antiarrhythmic medications, and (as with capture and fusion complexes) may also be confounded in patients with preexcitation (an accessory pathway). The challenges associated with these other approaches to rhythm diagnosis, underscores the importance of AV dissociation as arguably the simplest if not most reliable criterion for distinguishing supraventricular tachycardia with aberrancy from VT and why obtaining, either a rhythm strip or a 12-lead ECG is such a useful effort for looking for AV dissociation. If a 12-lead ECG is not available—as, for example, in the prehospital setting—an attempt to document the arrhythmia in at least two or more limb leads before proceeding to transport or with treatment can still serve to provide useful diagnostic information, even if only after the fact.
12-lead ECG has been obtained.9,10,11,12,13 Moreover, morphologic QRS criteria are less accurate in patients who have a preexisting QRS conduction abnormality, particularly if they are taking antiarrhythmic medications, and (as with capture and fusion complexes) may also be confounded in patients with preexcitation (an accessory pathway). The challenges associated with these other approaches to rhythm diagnosis, underscores the importance of AV dissociation as arguably the simplest if not most reliable criterion for distinguishing supraventricular tachycardia with aberrancy from VT and why obtaining, either a rhythm strip or a 12-lead ECG is such a useful effort for looking for AV dissociation. If a 12-lead ECG is not available—as, for example, in the prehospital setting—an attempt to document the arrhythmia in at least two or more limb leads before proceeding to transport or with treatment can still serve to provide useful diagnostic information, even if only after the fact.
ECG Clues—Differential Diagnosis of Wide-Complex Tachycardia (WCT)*
Supports Diagnosis of VT
P waves present in fewer number than QRS complexes (AV dissociation).
Fusion (Dressler) or “capture” beats consistent with occasional AV nodal conduction amid the WCT.
Supports Diagnosis SVT with Aberrancy
P waves present in equal or greater number than QRS complexes.
Prior ECG with bundle-branch block and similar QRS morphology.
Known accessory pathway conduction with similar QRS morphology.
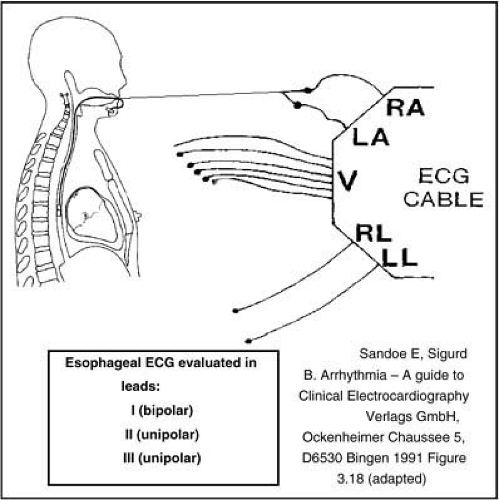
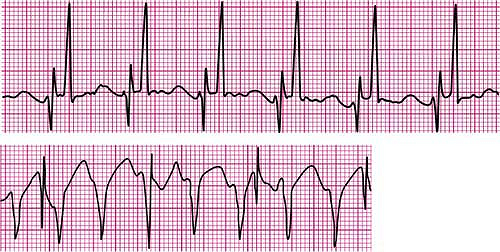 Figure 22-12 • Typical esophageal lead recording obtained in the manner depicted in Figure 22-11. Figure 22-12A depicts the appearance of normal sinus rhythm recorded from an esophageal lead. P waves appear larger in amplitude and more “spike-like” when recorded from a location that is closer to their site of origin compared to their smaller more rounded appearance on the ordinary surface ECG. In Figure 22-12B these higher amplitude, “spike-like” P waves can be more easily distinguished from the underlying wide complex tachycardia. In this instance, the atrial rate is much slower than the ventricular rate (AV dissociation) indicating that the rhythm is ventricular tachycardia. |
Esophageal Lead
If P waves are not seen on the 12-lead ECG, use of an esophageal lead may be helpful. The esophageal electrogram is a means of amplifying P waves to better evaluate a wide-complex tachycardia for atrioventricular dissociation. A standard transvenous pacing electrode can be used as an esophageal lead, although special esophageal electrodes are also commercially available. This electrode is placed in the esophagus, in similar fashion as a nasogastric tube, with the inserted length estimated to place the distal electrodes at center chest, or approximately behind the heart. In this location, the esophagus lies in close vicinity of and immediately posterior to the left atrium. Attaching the two pacing electrodes from the esophageal lead to the right and left arm electrodes of the ECG (with right and left leg leads in their usual positions) allows for recording amplified P waves in leads I, II, and III during the tachycardia (Fig. 22-11).14,15,16,17 A carefully evaluated 12-lead ECG, monitor tracing, or esophageal lead often permits identification of AV dissociation (Fig. 22-12). This is defined as the loss of a 1-to-1 relationship between atrial electrical activity (P waves) and ventricular response (QRS complexes), with more QRS complexes than can be accounted for by the number of P waves. AV dissociation is a highly specific criterion for VT.
Recently, the American Heart Association, American College of Cardiology, and European Heart Association updated standard definitions for the diagnosis and categorization of arrhythmias.4,5 These categories (which are modified for presentation here) help to characterize arrhythmias according to the patient’s symptoms (Table 22-1), ECG characteristics (Table 22-2), and associated heart disease (Table 22-3).
Regular Wide-Complex Tachycardias
General principles behind the creation of wide complex tachycardias were discussed previously (see page 320 of this chapter). In this section, we will discuss the specific rhythms that can present themselves as regular or irregular wide QRS tachycardias. Whereas regular narrow-complex tachycardias are virtually always of supraventricular origin, regular wide-complex tachycardias are more challenging to diagnose because they can be due to the same supraventricular causes as a regular narrow-complex tachycardia (see Fig. 22-2) but conduct aberrantly or via an accessory pathway to the ventricle; or they may be attributable to ventricular tachycardia. As previously discussed an occasional narrow QRS complex amidst a regular wide-complex tachycardia may represent an interposed sinus beat that happened to conduct to the ventricle between beats (called a capture or fusion beat) and suggests ventricular tachycardia (Fig. 22-13) in patients who are not known to have an accessory pathway (which can occasionally mimic the same finding during an atrial arrhythmia).18
Irregular Wide-Complex Tachycardias
In general, an irregularly irregular tachycardia with a uniform beat-to-beat QRS morphology most likely represents atrial fibrillation (Fig. 22-14). The QRS may be narrow or wide if there is aberrant conduction. The differential diagnosis of irregularly irregular tachycardias with QRS complexes that are not uniform across beats (QRS complexes vary in their appearance and in width) suggests the presence of atrial fibrillation with conduction to the ventricle variably
across one or more accessory pathways and the AV node, accounting for the variable appearance of QRS complexes (Fig. 22-15). This is referred to as preexcited atrial fibrillation. Alternatively, such an arrhythmia could represent polymorphic ventricular tachycardia, including torsades de pointes (Fig. 22-17). In this instance the varying QRS appearance is due to the unstable circuits and mechanisms causing the arrhythmia. Because both preexcited atrial fibrillation and polymorphic ventricular tachycardias are often quite rapid in rate and are hemodynamically unstable, they usually require immediate cardioversion. In addition, when polymorphic VT is sustained, it usually rapidly deteriorates to ventricular fibrillation.
across one or more accessory pathways and the AV node, accounting for the variable appearance of QRS complexes (Fig. 22-15). This is referred to as preexcited atrial fibrillation. Alternatively, such an arrhythmia could represent polymorphic ventricular tachycardia, including torsades de pointes (Fig. 22-17). In this instance the varying QRS appearance is due to the unstable circuits and mechanisms causing the arrhythmia. Because both preexcited atrial fibrillation and polymorphic ventricular tachycardias are often quite rapid in rate and are hemodynamically unstable, they usually require immediate cardioversion. In addition, when polymorphic VT is sustained, it usually rapidly deteriorates to ventricular fibrillation.
Table 22-1 • Classification of Arrhythmias by Clinical Presentation | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 22-2 • Classification of Ventricular Arrhythmias by ECG Characteristics | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
Table 22-3 • Heart Diseases Associated with Arrhythmias | |
|---|---|
|
The differential diagnosis of an irregularly irregular wide-complex tachycardia with nonuniform QRS complexes includes atrial fibrillation with preexcitation and polymorphic ventricular tachycardia. Because both preexcited atrial fibrillation and polymorphic ventricular tachycardias are often quite rapid in rate and are hemodynamically unstable, they usually require immediate cardioversion.
Treatment of Hemodynamically Stable Tachycardias
General Considerations
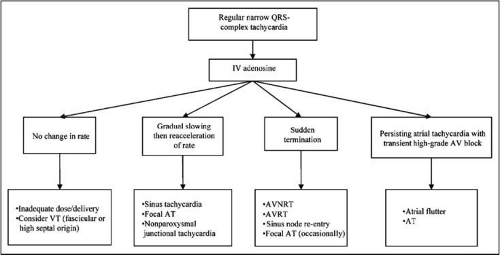
When circumstances and expertise allow, experienced health care providers should make a reasonable attempt to distinguish hemodynamically stable VT from SVT with or without aberrancy based on the QRS duration (width), regularity of the tachycardia, presence of P waves, and direct treatment of the most probable diagnosis. In general, vagal maneuvers or adenosine are recommended in the AHA ECC guidelines and the AHA/ECC guidelines for regular narrow-complex tachycardias. The response to adenosine
can help in the diagnosis and treatment of the patient with a regular narrow-complex SVT (Fig. 22-16). The key to understanding the response of a supraventricular tachycardia to adenosine is appreciating the differing effects of the drug on nodal tissue (sinus and AV nodes) as compared with muscle tissue. Adenosine slows sinus node impulse formation and slows (or transiently blocks) conduction in the AV node. Thus, given to a patient in normal sinus rhythm, adenosine would result in sinus bradycardia (or sinus arrest) with transient AV block, after which sinus node and AV node function would recover. Given for reentry arrhythmias that traverse the AV node (such as AVNRT or AVRT) or whose origin is in the sinus node (sinus node reentry tachycardia), adenosine would result in immediate termination of the arrhythmia. However, when given for atrial arrhythmias such as atrial fibrillation, atrial flutter, or an atrial tachycardia (either automatic or due to intra-atrial reentry) whose origin is in atrial muscle, the typical response to adenosine is continuation of the atrial arrhythmia with transient slowing of the ventricular response due the drug’s effects on the AV node, followed by resumption of the arrhythmia at its usual ventricular rate. Occasionally, however, adenosine may terminate a focal (automatic) atrial tachycardia.
can help in the diagnosis and treatment of the patient with a regular narrow-complex SVT (Fig. 22-16). The key to understanding the response of a supraventricular tachycardia to adenosine is appreciating the differing effects of the drug on nodal tissue (sinus and AV nodes) as compared with muscle tissue. Adenosine slows sinus node impulse formation and slows (or transiently blocks) conduction in the AV node. Thus, given to a patient in normal sinus rhythm, adenosine would result in sinus bradycardia (or sinus arrest) with transient AV block, after which sinus node and AV node function would recover. Given for reentry arrhythmias that traverse the AV node (such as AVNRT or AVRT) or whose origin is in the sinus node (sinus node reentry tachycardia), adenosine would result in immediate termination of the arrhythmia. However, when given for atrial arrhythmias such as atrial fibrillation, atrial flutter, or an atrial tachycardia (either automatic or due to intra-atrial reentry) whose origin is in atrial muscle, the typical response to adenosine is continuation of the atrial arrhythmia with transient slowing of the ventricular response due the drug’s effects on the AV node, followed by resumption of the arrhythmia at its usual ventricular rate. Occasionally, however, adenosine may terminate a focal (automatic) atrial tachycardia.
IV calcium or beta-blockers are recommended for irregular narrow-complex tachycardias or for regular narrow-complex tachycardias that recur or are resistant to adenosine. Wide-complex tachycardias known to be of supraventricular or ventricular origin should be treated in the same way as the suspected supraventricular arrhythmia. An exception is a wide-complex supraventricular tachycardia that is felt to be associated with an accessory pathway (such as preexcited atrial fibrillation or flutter). In this case, expert consultation is recommended before proceeding with treatment. Specifically, preexcited atrial arrhythmias (such as atrial fibrillation or flutter) should not be treated with AV-nodal blocking drugs such as adenosine, digoxin, calcium channel blockers, or beta-blockers.
Preexcited atrial arrhythmias (such as atrial fibrillation or flutter) should not be treated with AV nodal blocking drugs such as adenosine, digoxin, calcium channel blockers, or beta-blockers. Seek expert consultation. If a rhythm diagnosis is not possible, expert consultation is not readily available, and treatment is required, a wide-complex tachycardia may be empirically treated with IV amiodarone.
If a rhythm diagnosis is not possible, expert consultation is not readily available, and treatment is required, a wide-complex tachycardia may be empirically treated with IV amiodarone. The broad-range electrophysiologic properties of amiodarone make the drug effective for both ventricular and supraventricular tachycardias, including those involving an accessory pathway.19 However, if possible, expert consultation should be sought before such empiric treatment is initiated or if there is suspicion for preexcited arrhythmias or polymorphic ventricular tachycardia. If torsades de pointes is suspected, magnesium is the preferred treatment.20
Monitor Hemodynamics Carefully During Drug Administration
Because most drugs used for most tachycardias lower blood pressure, pretreatment blood pressures should be sufficiently high to permit use of such drugs. Typically the hypotensive effect of drugs is more than compensated for by the restoration of sinus rhythm. However, a precipitous drug-induced fall in blood pressure without termination of the arrhythmia should prompt immediate electrical cardioversion. Most but not all arrhythmias ([the notable exceptions being automatic (focal) atrial tachycardia and multifocal atrial tachycardia]) are shock-responsive.
Obtain Pre- and Postconversion 12-Lead Electrocardiograms
If possible, a 12-lead ECG or a continuous rhythm strip should be obtained immediately before and during pharmacologic interventions and after conversion to a regular rhythm.
Treatment of Specific Arrhythmias Ventricular Tachycardia (VT)
Hemodynamically Stable VT
The initial step in the management of any arrhythmia is to determine if the patient is stable or unstable. An unstable patient with a wide-complex tachycardia is presumed to have VT until proven otherwise. If the patient is hemodynamically unstable, immediate cardioversion is performed (see Fig. 22-1, Box 4). If the VT is hemodynamically stable,
further evaluation and treatment options can be considered with expert consultation.
further evaluation and treatment options can be considered with expert consultation.
VT is considered “hemodynamically stable” if there are no symptoms or clinical evidence of tissue hypoperfusion or shock. Hemodynamically unstable VT requires immediate termination with synchronized cardioversion. Even among patients who appear clinically stable, it is necessary to judge whether there is sufficient time and blood pressure margin for pharmacologic interventions, because success is uncertain, the onset of action often delayed, and side effects, which include hypotension, occur frequently. Electrical cardioversion is, therefore, a preferred treatment strategy for clinically stable ventricular tachycardia, given its high efficacy and ability to rapidly restore sinus rhythm without the uncertainties and potential side effects of antiarrhythmic drugs. However, in instances where cardioversion is not possible (if, for example, the patient is regarded as being at high risk from the required level of sedation for shock), cardioversion has already proven to be unsuccessful, or VT has recurred after successful cardioversion, pharmacologic therapy is reasonable and appropriate.
Even if patients appear clinically stable, it is necessary to judge whether there is sufficient time and blood pressure margin for pharmacologic interventions, because success is uncertain, onset of action often delayed, and side effects, which include hypotension, occur frequently.
Monomorphic VT
Monomorphic VT is defined as ventricular tachycardia with a regular rate and with QRS complexes that appear uniform (Fig. 22-10). It likely originates from a single reentry circuit in the ventricle. Although automatic ventricular tachycardias (emerging from an automatic rather than reentrant ventricular focus) can occur, most monomorphic ventricular tachycardias can be presumed to be caused by reentry and approached accordingly. The most typical setting for development of an automatic ventricular rhythm (accelerated idioventricular rhythm) can be during the reperfusion phase of acute myocardial infarction. An accelerated idioventricular rhythm (typically due to an excited automatic focus in the Purkinje system) is usually 120 bpm or slower, as compared with the more rapid rates of reentry VT. It frequently abates spontaneously and may not require specific treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree