Sympathetic Blocks: Stellate, Celiac, Lumbar, Superior Hypogastric, and Ganglion Impar
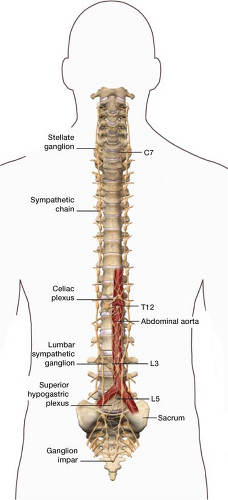
The sympathetic chain is a bundle of nerves that runs from the base of the skull to the tip of the spine. The sympathetic chain runs along the vertebral bodies in a paravertebral fashion (Fig. 24-1). At points the nerves bundle together into ganglia. Ganglia are groups of nerve cells forming a nerve center located outside the brain. Each ganglion is responsible for providing neural transmission to and from different parts of the body. These ganglia make up the sympathetic chain.
The sympathetic chain is part of the autonomic nervous system, which controls functions that occur automatically and unconsciously (dilation of a blood vessel, changes in heart rate, or contraction of a sphincter) compared with the somatic nervous system, which controls motor and sensory function (skeletal muscle control, e.g., flexing a bicep, and sensation, such as feeling sandpaper). Table 24-1 gives the name, location, and corresponding body part for each sympathetic ganglion.
When to use
Sympathetic blocks have three main indications.
First they are indicated for the treatment of sympathetically maintained pain. It has been shown that by blocking the sympathetic ganglion, pain relief can be achieved in the corresponding body part that lasts longer than the expected duration of a local anesthetic injected. Therefore, aberrant actions of the sympathetic nervous system may generate pain in peripheral tissues. The classic example of this is complex regional pain syndrome (CRPS, formerly known as reflex sympathetic dystrophy [RSD]). The presence of regional edema in the skin and accompanying irregularities in blood flow/temperature and pseudomotor regulation suggests an autonomic component to the disease. A stellate ganglion block is used for the treatment of upper extremity CRPS whereas a lumbar sympathetic block is used for the treatment of lower extremity CRPS.
Second indication is for pancreatic, pelvic, or peritoneal pain. The classical example of this is a celiac plexus block for pancreatic pain. Fibers that conduct painful impulses from the pancreas are transmitted to the brain along the celiac plexus. By blocking these fibers, it is possible to control pathologic painful impulses. For noncancerous pain, such as pancreatitis, a sympathetic block with a local anesthetic can help break the pain cycle. For cancer pain, a diagnostic block using a local anesthetic is necessary—if positive, a neurolytic block consisting of using pure alcohol or phenol. Phenol causes nerve destruction by inducing protein precipitation, leading to a separation of the myelin sheath from the axon and axonal edema. Six percent phenol produces nerve necrosis within 24 hours. Alcohol causes nerve destruction by extracting phospholipids, cholesterol, and cerebroside from neural tissues. Although 50% to 100% alcohol is used as a neurolytic agent, the minimum concentration required for neurolysis has not been established. Neurolytic sympathetic blocks are reserved for cancer pain because they can lead to deafferentation pain. Deafferentation pain is a complex pain syndrome characterized by burning pain and marked sensitivity to touch in the distribution of a chemically lysed ganglion. In oncology
patients deafferentation pain is not usually of concern, because by the time it develops the patients will most likely have succumbed to the disease. A superior hypogastric block is used primarily to control pelvic cancer pain from the bladder, urethra, uterus, vagina, vulva, perineum, prostate, penis, testes, or rectum. There is a crossover of innervation with the ganglion impar which is used classically for cancer pain from rectal, vulva, or distal third of the vagina.
patients deafferentation pain is not usually of concern, because by the time it develops the patients will most likely have succumbed to the disease. A superior hypogastric block is used primarily to control pelvic cancer pain from the bladder, urethra, uterus, vagina, vulva, perineum, prostate, penis, testes, or rectum. There is a crossover of innervation with the ganglion impar which is used classically for cancer pain from rectal, vulva, or distal third of the vagina.
Table 24-1 Spinal Location of Sympathetic Chain in the Body and Body Part they are Associated With | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Third they are indicated for ischemic syndrome of a limb. This includes peripheral vascular disease, gangrene, arterial embolism, and frostbite. In a patient with peripheral vascular disease, a sympathetic block can relieve the tonic baseline level of arterial vasoconstriction, allowing for increased circulation as well as decreased pain.
How to Perform the Procedure
Each of these procedures described involve the same initial steps. Fully explain the procedure to the patient, answer all questions, and obtain informed consent. Ensure that intravenous (IV) access has been placed, because all sympathetic blocks can cause hypotension. IV access should be available in the rare instances that it is necessary to give fluids to provide pressure support after a block. The patient lies on the fluoroscopic table. For accuracy and safety, all procedures are performed under fluoroscopic guidance (live x-ray). A “time out” is performed prior to the procedure including verbal confirmation of correct patient, procedure and procedural site. Noninvasive hemodynamic monitors and pulse oximetry are placed.
Stellate Ganglion Block
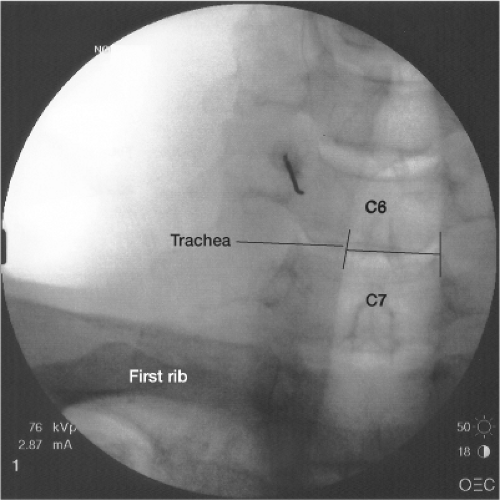
The stellate ganglion is formed by the fusion of the inferior cervical ganglion and the first thoracic ganglion. It is typically located at the level of C7 (seventh cervical vertebrae), anterior to the transverse process of C7 (Fig. 24-2). Anatomical variation does exist and the ganglion may be anterior to the transverse process of C6.
One expected result of a stellate ganglion block is an ipsilateral Horner syndrome (ptosis, miosis, and anhydrosis) because of the sympathetic blockade. Horner syndrome dissipates as the local anesthetic wears off. The patient should be informed of the expected after-block facial changes before the procedure.
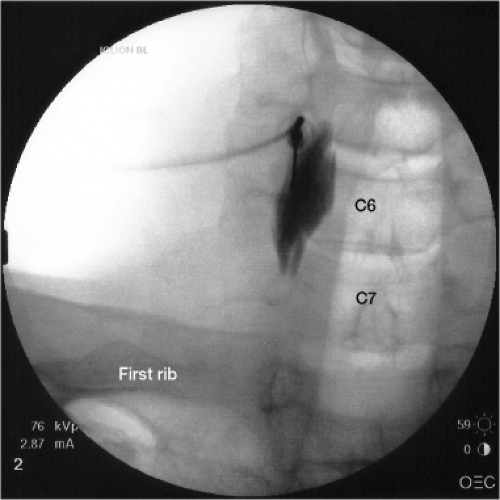
The patient should be in the supine position (face up) on the fluoroscopic table. The fluoroscopy machine is placed in the anteroposterior (AP) position. The skin between the chin and the nipple on the side of pain is prepped with betadine and drapes are placed over the area in standard sterile fashion. The tubercle of the C6 vertebral body, Chassaignac tubercle, on the side of pain is brought into focus. Needle placement at C6, rather than C7, provides sufficient clearance from the top of the lung fields yet is still anatomically close enough for proper medication diffusion over the area. Using a metal marker and a felt-tip marking pen, an “X” is placed on the skin overlying the intended target (Fig. 24-3). The skin is anesthetized with lidocaine using a 1.5-in, 25-gauge needle (Fig. 24-4). After the skin is anesthetized, a 2.5-in, 22-gauge spinal needle is placed through the “X” in a perpendicular fashion to the skin and parallel to the fluoroscope. The needle is advanced until it comes in contact with the bone of the C6 tubercle. The needle should remain lateral to the trachea. It may be necessary to manually maneuver the trachea gently to clear a path for the needle. After bony contact, the needle is withdrawn 2 mm to bring the needle tip out of the body of the longus colli muscle. The stylet of the needle is then removed. A 3-mL syringe filled with contrast is connected to tubing (the tubing primed) and is connected to the needle. Tubing is used so that you can see the contrast being injected under live x-ray without having your hand obscure the image and to protect your hand from radiation exposure. Aspirate with the 3-mL syringe to check for blood or cerebrospinal fluid (CSF) return. After negative aspiration, the contrast is injected to make sure that it spreads over the area of the stellate ganglion and that no contrast is taken up by a vessel, indicating that the
tip of the needle is in a vessel. Once proper contrast spread is seen (Fig. 24-5), the 3-mL syringe containing contrast is disconnected from the tubing. A 10-mL syringe with the therapeutic agent, a local anesthetic, is connected to tubing and injected in 2.5-mL aliquots. I use a mixture of 4 mL of 2% lidocaine and 4 mL of 0.5% bupivacaine in a 10-mL syringe as my therapeutic agent. The needle is then removed and a bandage placed.
tip of the needle is in a vessel. Once proper contrast spread is seen (Fig. 24-5), the 3-mL syringe containing contrast is disconnected from the tubing. A 10-mL syringe with the therapeutic agent, a local anesthetic, is connected to tubing and injected in 2.5-mL aliquots. I use a mixture of 4 mL of 2% lidocaine and 4 mL of 0.5% bupivacaine in a 10-mL syringe as my therapeutic agent. The needle is then removed and a bandage placed.
Celiac Plexus Block
There are many effective approaches to blocking the celiac plexus. Following discussion describes the standard splanchnic approach.
The patient is placed on the fluoroscopic table in the prone position (face down) with a pillow under the abdomen to flex the thoracolumbar spine. The fluoroscopy machine is placed in the AP position. The back is prepped with betadine and drapes are placed over the area in standard sterile fashion. The L1 vertebral body is brought into focus. Using a metal marker and a felt-tip marking pen, an “X” is placed on the skin overlying the lateral aspect of transverse process of the L1 vertebral body (Fig. 24-6). The skin is anesthetized with lidocaine using a 1.5-in, 25-gauge needle. After the skin is anesthetized, a 5-in spinal needle with at least a 30 degree curve at the end—the physician typically bends the needle to create a curve (Fig. 24-7)—is placed through the “X” in a perpendicular fashion to the skin and a parallel fashion to the camera. The curve at the tip of the needle is key in helping steer the needle medially in the latter part of the procedure. A 7-in needle may be needed for heavier patients. The needle is advanced until it comes in contact with the bone of the lateral aspect of the L1 transverse process. After contacting the transverse process, the needle is then slightly withdrawn and redirected toward the lateral aspect of the T12 vertebral body (toward the head) and further advanced (Fig. 24-8). This nondirect approach to the anterior border of the T12 vertebral body is used to avoid the lung fields. At this point, the camera is switched to a lateral view. When the needle touches the lateral aspect of the T12 vertebral body, the curved point is rotated away from the vertebral body so that it can be advanced further anteriorly. The needle is then rotated back medially to continue medially toward the celiac plexus, which lies near the anterior border of the T12 vertebral body (Fig. 24-9). Once the needle is brought into final position, just anterior to the T12 vertebral body, the stylet of the needle is removed. A 5-mL syringe is tightened on the spinal needle and aspirated to check for blood or CSF. If blood is withdrawn the needle tip is located too anterior and should be repositioned. After negative aspiration, the 5-mL syringe is
disengaged and a 3-mL syringe with tubing containing contrast is connected to the needle. Tubing is used so that you can see the contrast being injected under live x-ray without having your hand obscure the image and to protect your hand from radiation exposure. The contrast is injected to make sure that it spreads over the area of the celiac plexus and that no contrast is taken up by a vessel, indicating that the tip of the needle is in a vessel. If the needle is advanced too far anteriorly, you will see blood on aspiration or the contrast being whisked away under fluoroscopy. At this point, guide the needle posteriorly, toward you, until the needle is in proper position. Once proper contrast spread is seen (Fig. 24-10), the 3-mL syringe containing contrast is disconnected from the tubing. The spinal needle is now properly placed.
disengaged and a 3-mL syringe with tubing containing contrast is connected to the needle. Tubing is used so that you can see the contrast being injected under live x-ray without having your hand obscure the image and to protect your hand from radiation exposure. The contrast is injected to make sure that it spreads over the area of the celiac plexus and that no contrast is taken up by a vessel, indicating that the tip of the needle is in a vessel. If the needle is advanced too far anteriorly, you will see blood on aspiration or the contrast being whisked away under fluoroscopy. At this point, guide the needle posteriorly, toward you, until the needle is in proper position. Once proper contrast spread is seen (Fig. 24-10), the 3-mL syringe containing contrast is disconnected from the tubing. The spinal needle is now properly placed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree