Substance Abuse
Stephen Paul Holzemer PhD, RN
Joanne Singleton PhD, RN, FNP-C
The use of alcohol and other legal as well as illegal chemical substances is a growing problem in many societies. Approximately 10% to 20% of a primary care provider’s caseload involves patients with substance use disorders (Israel et al, 1996). Substance abuse has a profound effect on the mortality and morbidity of many patients, their families, and their communities. The social cost related to accidental death, violence, loss of productivity in the workforce, and unemployment can only be estimated. A definition of substance abuse must include the behavior of the patient and the effect of the abuse on all these variables.
This chapter is a general overview of substance abuse problems and challenges for the provider. A review of these issues should be made on a patient-by-patient basis because of the many complexities of substance abuse. Providers must construct an interdisciplinary approach based on the demographics of their practice locations.
The term substance abuse is used in this chapter to include concepts of use and misuse. Relationship-centered care would rely on assessing and intervening into patterns of substance use well before abuse patterns develop.
GENERAL PRINCIPLES FOR PLANNING CARE
Substance abuse is complicated because the drugs involved may be prescribed, purchased over the counter, or sold in illegal transactions. The addictive nature of these substances makes changing the using behavior difficult. Some patients may become physically or emotionally abusive if the pattern of their drug use changes, including withdrawal. Identifying, engaging, and managing the active substance user includes cooperation between generalist providers and an emerging cadre of specialists in substance abuse.
Primary care providers must first examine their own attitudes about substance abuse. Providers must define what is acceptable and unacceptable use and how to motivate or encourage patients to change their behavior. Exploring these issues with the patient allows care to be provided from a supportive but well-planned perspective. The plan of care involves family members and other support persons willing or able to participate in recovery.
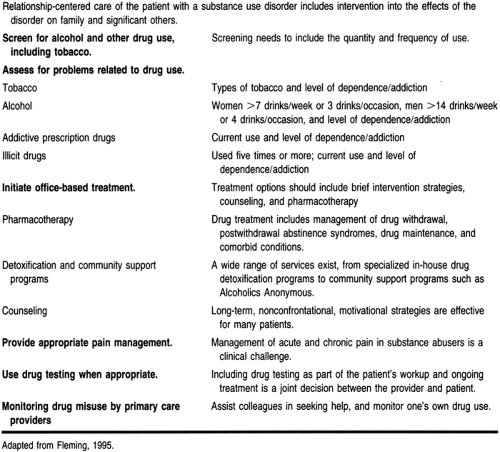
Caring for the substance abuser is very expensive (Lewis, 1997). The challenges of cost containment in health care make providing comprehensive care to the substance abuser a concern for many providers. Fleming (1995) identified nine competencies needed by primary care providers in caring for the substance abuser, and these nine have been restructured into six (Table 64-1). These competencies should allow providers a framework to identify their strengths and limitations in caring for substance abusers.
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
The effect of substance abuse on body systems ranges from temporary impairment to multisystem failure. Long-term drug use can cause diseases of the lungs (cancer), liver (cirrhosis), heart (cardiac myopathy, ischemia, hypertension), and gastrointestinal tract (gastritis, hemorrhage, malnutrition). Alcohol use has been associated with breast cancer in women (Smith-Warner et al, 1998), as well as demineralization of the bone (Chang et al, 1997). Cocaine has induced wide complex dysrhythmia in some patients (Kerns et al, 1997) and myocardial infarction. Patients may present only after serious health problems surface.
Changes in pleasure pathways occur in the brain and the number and receptivity of dopamine and serotonin receptors increase with substance use. These changes add to the physiologic challenge in substance use, which is sometimes overshadowed by the psychosocial aspects. Finding a chromosomal link to a biologic cause or predisposition to addiction would help predict who would be at risk for these health-related problems.
EPIDEMIOLOGY
Substance abuse accounts for 50% of the more than 1 million deaths attributed to unsafe or unhealthy lifestyle behaviors (Lewis, 1997). The morbidity often extends to include relatives and friends of the substance user. For example, children may have asthma attacks triggered by tobacco use (second-hand smoke). Family members may experience physical, emotional, and economic harm because of the behavior of the substance abuser. Family members and others may be the victims of crime when substance abusers seek money for drugs or are under the influence of drugs.
The differing effects of substance abuse on Hispanics, African Americans, and whites is still under study (Caetano, 1997; Herd, 1997). One predictor of substance abuse in women is childhood sexual abuse (Wilsnack et al, 1997) or victimization (Liebschutz et al, 1997). There is increasing research interest in how abuse affects the entire family (Ryan et al, 1997).
The wide variation in the physical, occupational, and economic attributes of drug users suggests that all patients should be screened for substance use and potential abuse. No clear profile of a typical substance user has emerged.
Alcohol Use
Approximately 70% of men and 60% of women drink (or have drunk) alcohol. Men are three times more likely to binge (five or more drinks on one occasion) than women and six to seven times more likely to be chronic drinkers. The disease occurs
earlier in men but may be fatal earlier in women (Centers for Disease Control and Prevention [CDC], 1996, 1997a; Chang et al, 1997).
earlier in men but may be fatal earlier in women (Centers for Disease Control and Prevention [CDC], 1996, 1997a; Chang et al, 1997).
Smoking
About 25% of men and slightly fewer women smoke. Almost 33% of college students smoke. There is some evidence that the incidence of smoking (defined as being a current smoker and having had smoked at least 100 cigarettes) is decreasing in teenagers, both boys and girls (CDC, 1996, 1997a, 1997b). Tobacco industry promotions are considered a major contributor to adolescent smoking (Pierce et al, 1998).
Illegal Drug Use
Almost 40% of adults have used an illicit drug during their lives. Of these, 33% have used marijuana and 11% have used cocaine (Schorling & Buchsbaum, 1997). Among college students, 48% had smoked marijuana, 14.4% had used some form of cocaine, 9.1% had used inhalants (eg, glue, spray can contents), and 1.7% had injected illegal drugs in their lifetime (CDC, 1997b). These percentages may be low because of underreporting, making the problem much more serious.
DIAGNOSTIC CRITERIA
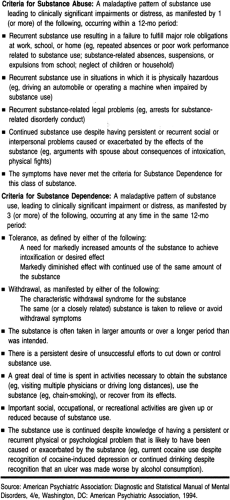
The criteria for substance abuse and dependence (including alcohol) are listed in Table 64-2 (American Psychiatric Association, 1994). This information can help the provider screen for substance use.
Toxicology screens do not differentiate between occasional use and dependence (Schorling & Buchsbaum, 1997). The presence of a drug in the body suggests the need for the provider to explore the impact of alcohol and drug use on the patient and family. For many patients, the impact of alcohol and other drugs on behavior and relationships defines the level of abuse. Events such as being arrested for driving while intoxicated are indicative of an alcohol-related problem that the provider must continue to explore.
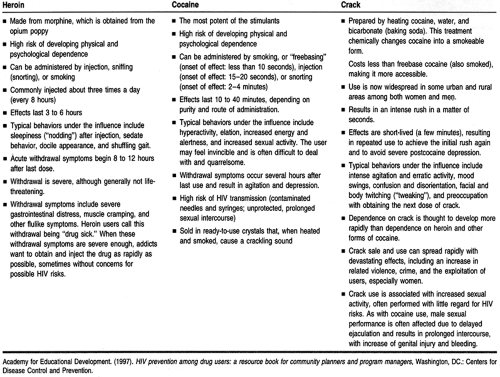
Two illegal drugs that account for much drug abuse are heroin and cocaine (including crack cocaine). The characteristics and effects of their use are listed in Table 64-3. These drugs are highlighted because of the complex nature of their addictive potential. They are also closely tied to the spread of HIV infection (Academy for Educational Development, 1997). Individuals under the influence of these drugs may have unprotected sex more often.
HISTORY AND PHYSICAL EXAM
Screening for alcohol and other drug abuse is a sensitive part of the history and physical exam. An interpersonal relationship between the patient and the provider needs to be established before the provider can expect such questions to be answered in a thorough and honest manner. Some providers ask patients if they have experienced recent trauma (physical or emotional) as a way to elicit problem drinking behavior (Israel et al, 1996). Many accidents are alcohol-related, and the provider needs to
screen for alcohol or other drug use when accidental or suspicious trauma occurs.
screen for alcohol or other drug use when accidental or suspicious trauma occurs.
Questionnaire Assessments
Numerous questionnaires have been designed to identify substance abuse disorders. However, in the absence of a trusting patient–provider relationship, patients may harbor the truth when answering these highly personal questions; a “no” response may be meaningless. Providers must assess the impact of using these questions on their relationship with patients.
Ewing (1984) developed the CAGE questionnaire to detect alcoholism, and these questions have been adapted to screen for other drug dependencies. The CAGE questionnaire is thought to be a gold standard for drug abuse screening. The CAGE questions are:
C: Have you ever felt that you should Cut down on your drinking?
A: Have people Annoyed you by criticizing your drinking?
G: Have you ever felt bad or Guilty about drinking?
E: Have you ever taken a drink first thing in the morning (Eye Opener) to steady your nerves or get rid of a hangover?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree