Sexually Transmitted Infections
Carol Buck-Rolland MS, PNP, OGNP
Deborah Wachtel MPH OGNP
This chapter begins with a discussion of sexually transmitted infections (STIs) in general, followed by sections covering chlamydia, gonorrhea, syphilis, herpes simplex virus, human papillomavirus, bacterial vaginosis, trichomoniasis, and moniliasis. The anatomy and physiology of the male reproductive system are described in Chapters 68 and 70. Female reproductive anatomy is described in Chapter 71. The pathology of each of the STIs is discussed in this chapter. Patient history is not specifically discussed; the provider should ask questions using the standard sexual history and symptom format when screening for STIs. For more specific information on history taking, refer to Chapters 66, 67, and 70. Comprehensive epidemiologic statistics are not provided for trichomoniasis, moniliasis, or bacterial vaginosis because these are not reportable infections; interested readers are referred to current gynecologic texts. Teaching and self-care is covered in the section on STIs in general.
STIs, also known as sexually transmitted diseases (STDs), present a major public health problem in the United States. STIs comprise more than 25 infectious organisms that are transmitted through sexual activity (vaginal, oral, and anal intercourse), along with the dozens of clinical syndromes they cause. Studies show that STIs enhance the risk of sexual transmission of HIV infection (Wasserheit, 1992; Laga et al, 1993, Kreiss, 1994; U.S. Department of Health and Human Services [USDHHS], 1993, 1997). The spectrum of health consequences of STIs ranges from mild acute illness to serious long-term complications (Eng & Butler, 1997).
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
In young female adolescents, the ectocervix has not yet changed from columnar cells to the more protective-type epithelial cells, biologically increasing their vulnerability to the invasion of sexually transmitted infections. Adolescents who initiate intercourse at a young age are more likely to be exposed to multiple partners and risk factors. Any or all of these factors increase the risk of infections over time. Men who are uncircumcised may be at a greater risk (as are their partners) of acquiring certain STIs, such as HIV and chancroid (see Chap. 70). Women who douche are at a higher risk for bacterial vaginosis as well as for later complications of STIs, such as pelvic inflammatory disease (PID). A correlation exists between PID and the frequency of douching (Eng & Butler, 1997) Douching alters the pH of the vaginal mucosa, resulting in an increased susceptibility to transmission of STIs.
STIs are transmitted among all sexually active people, including heterosexuals, bisexuals, and homosexuals. Men who have sex with men are at a greater risk for many life-threatening STIs, including AIDS and hepatitis B and C (American Medical Association, 1995). Women who have sex only with women seem to be at less of a risk for some bacterial STIs. Bacterial vaginosis and genital human papillomavirus infections, however, are not uncommon (Berger et al, 1995).
Certain sexual practices are more likely to facilitate the transmission of STIs. Unprotected receptive rectal intercourse is likely to result in tissue trauma and bleeding, which can facilitate invasion by pathogens. Unprotected vaginal intercourse may also result in tissue trauma, although generally to a lesser degree. Tissue damage facilitates the transmission of both bloodborne pathogens and other viral STIs. Vaginal intercourse during menstruation may facilitate STI transmission. Oral sex is less likely to promote the transmission of STIs.
EPIDEMIOLOGY
Currently, AIDS, syphilis, and gonorrhea are reportable diseases in all 50 states. Primary care providers need to be knowledgeable about the reporting requirements in the areas where they practice. Health departments in many states provide anonymous tracking and notification of partners of patients found to be infected with an STI that falls into the category of a reportable disease. Partner notification can help prevent the spread of reportable infections. According to recent data from the Centers for Disease Control and Prevention (CDC; USDHHS, 1996):
More than 12 million Americans, including 3 million teenagers, are infected with STIs each year.
Two thirds of persons who acquire STIs are under age 25.
87% of all STI cases reported were among the top 10 most frequently reported diseases in the United States in 1995.
Since 1980, eight new sexually transmitted pathogens have been recognized in the United States.
Every year, about $10 billion is spent on major STIs (other than AIDS) and their preventable complications.
Women and adolescents are disproportionately affected by STIs and their consequences of transmission (Eng & Butler, 1997; USDHHS, 1996).
Risk Factors
Behaviors that place patients at risk for STIs include:
TEACHING AND SELF-CARE
Because of the prevalence and consequences of STIs, all primary care providers need to participate actively in prevention efforts. These efforts should focus on preadolescents, before sexual activity begins, and should be driven by current research and surveillance data and re-evaluated frequently. Prevention efforts need to target high-risk populations and provide appropriate messages. These messages must be repeated often and in a variety of ways, altering the strategies depending on the target audience. Clinical services for prevention education as well as for diagnosis and treatment must be available and effective. Local primary care providers can provide such access. STI education should be included in all routine patient encounters. All sexually active patients need to be informed of how sexually transmitted infections are acquired. Primary care providers can work with local health departments and local schools to provide comprehensive STI services. Primary care providers should implement the recommendations of the U.S. Preventive Services Task Force (1996) and the CDC (1993, 1997) for prevention, screening, and management of STIs. The CDC publishes an annual STD surveillance report. Their guidelines for treating STDs are updated every 3 years.
CHLAMYDIA
Infections caused by Chlamydia trachomatis are among the most common STIs. Complications in women caused by chlamydia include PID, tubal factor infertility, and ectopic pregnancy. If not adequately treated, 20% to 40% of women infected with chlamydia will develop PID. Pregnant women can transmit the infection to their babies during delivery, potentially causing conjunctivitis or pneumonia. Adolescents and young adults are at a substantial risk of becoming infected with this infection. Unrecognized infection is believed to be highly prevalent in this group (USDHHS, 1993).
Anatomy, Physiology, and Pathology
Infection by chlamydia is insidious. Approximately 70% of chlamydial infections are asymptomatic. The rectum is a common site of initial chlamydial infection for men who engage in receptive anal intercourse. Exposure to chlamydia in females is a result of sexual intercourse. The site of the initial infection is typically the cervix. The urethra and the rectum may also be infected. The infection travels up through the cervix to the vagina, endometrium, and fallopian tubes. This upward migration may induce lower abdominal pain and minor irregular bleeding, such as postcoital bleeding. The proportion of women with chlamydial infection who develop upper reproductive tract infection (endometritis, salpingitis, and pelvic peritonitis) is uncertain. Chlamydia, alone or with other microorganisms, has been isolated from 5% to 50% of women seeking care for symptoms of PID. In 1991, more than 275,000 women were hospitalized and more than 100,000 surgical procedures were performed as a result of PID (USDHHS, 1993). Approximately 17% of women treated for PID will be infertile; an equal proportion will have chronic pain as a result of infection; and 10% of those who do conceive will have an ectopic pregnancy.
Chlamydial salpingitis may progress to perihepatitis. Chlamydia may be a cause of cystitis in women who have leukouria but negative urine cultures. Pregnant women with chlamydia are at risk for postpartum PID and endometritis (USDHHS, 1993).
Epidemiology
By 1995, 48 states had implemented legislation mandating reporting of chlamydia. The CDC has tracked chlamydial infections since 1984. The sharp increases in the prevalence of infection since 1984 primarily reflect increased screening, recognition of asymptomatic infection (mainly in women), and improved reporting capacity. In 1995, 477,638 chlamydial infections were reported to the CDC. For a second consecutive year, reported cases of chlamydia exceeded the 392,848 reported cases of gonorrhea in 1995. Reported cases of chlamydia for women (290.3 per 100,000 population) exceed those for men (52.1 per 100,000 population) (USDHHS, 1996).
Diagnostic Criteria
Symptoms rarely occur in either gender. When they do occur in females, symptoms include vaginal discharge and dysuria. Most men infected with chlamydia are asymptomatic. Chlamydial infections among heterosexual men may typically induce urethral symptoms of dysuria and discharge. Rectal infections in either gender are generally asymptomatic but may cause symptoms of proctitis (rectal discharge, pain during defecation) or proctocolitis (USDHHS, 1993).
CLINICAL WARNINGS
Reiter’s syndrome (reactive arthritis, conjunctivitis, and urethritis) is an uncommon complication of untreated chlamydial infection, occurring primarily among men.
In both genders, chlamydia should be considered in chronic conjunctivitis in adolescents and young adults. Although chlamydia can be detected in the pharynx after inoculation from oral–genital exposure, chlamydia has not been established as a cause of pharyngitis.
History and Physical Exam
Female partners of males with chlamydial infection should be offered a pelvic exam, chlamydia testing, and treatment. The testing and exam of female partners is recommended because:
A positive test result may mean that additional partners may be infected.
Asymptomatic women may have signs of PID on examination, requiring more intensive therapy.
Women may be asymptomatically infected with other STIs.
Male partners of females with chlamydial infection should be evaluated for symptoms of chlamydia and other STIs and for allergy to the treatment medication. A physical exam of
male sex partners should be encouraged, but the exam is less important than treatment. The exam is recommended because:
male sex partners should be encouraged, but the exam is less important than treatment. The exam is recommended because:
A positive test may lead to the treatment of additional partners who may be infected.
Men may be asymptomatically infected with other STIs.
Male partners may be allergic to the treatment medication.
If it is not possible for a male partner to be examined, the provider must determine that the man does not have symptoms suggestive of another STI and is not allergic to the treatment medication.
Diagnostic Studies
A number of nonculture tests are marketed for the detection of chlamydia. Nonculture tests are easier to perform and are less expensive than cultures. Tests available include:
Enzyme immunoassays to detect chlamydia antigens
Fluorescein-conjugated monoclonal antibodies for the direct visualization of chlamydia elementary bodies on smears
Nucleic acid hybridization tests
Rapid tests.
CLINICAL WARNING
Nonculture tests have less specificity, leading to false-positive results. All positive nonculture tests should be interpreted as presumptive.
CLINICAL PEARLS
The preferred collection site is the endocervix in women, the urethra in men. Cell culture testing is available and highly specific.
Endocervical specimens should be obtained after obtaining Pap smears or cervical cultures. Urethral specimens should be delayed until 2 hours after the patient has voided. Specific instructions for the various tests must be followed.
The disadvantages of cell cultures include:
Delayed results (3 to 7 days)
Only viable organisms are detected, necessitating a special transport medium with control of temperature, and additional cost.
Both enzyme immunoassay and direct fluorescent antibody assay of a first morning urine sample can identify as many infected symptomatic men as does a culture of urethral swabs. Few if any false-positive results are associated with these tests. However, they fail to identify more than 40% of cases in women (Lee et al, 1995).
Urine collection for chlamydia assay uses the nucleic acid amplification method to detect the presence of chlamydia DNA in the specimen. Two methods are the polymerase chain reaction and the ligase chain reaction. Urine collection for detection is less invasive, and early studies have shown a high rate of infection detection, almost 30% greater than that of endocervical swab culture (Chernesky et al, 1994; Epidemiology Newsletter, 1996; Lee et al, 1995).
The leukocyte estrase test is a dipstick that is applied to urine specimens to screen for urinary tract infection. Data are being collected to determine the role of this tool in the diagnosis of chlamydia.
Culture is the preferred method for detecting chlamydia in rectal specimens. The performance of nonculture tests with conjunctival specimens has been at least as effective as with genital specimens. Chlamydial serology has little value in the routine clinical care of genital tract infections. Chlamydial infections elicit long-lasting antibodies that cannot be easily distinguished from the antibodies produced in a current infection.
CLINICAL PEARL
If a post-treatment test is performed using a nonculture test, the test should be scheduled at least 3 weeks after the completion of antimicrobial therapy.
Everyone with whom the patient has had ongoing sexual exposure within 60 days of the positive test result should be treated. The primary care provider should inform infected patients to have their partners examined and treated. Public health department providers can anonymously contact exposed partners if the patient chooses not to inform them.
Treatment Options, Expected Outcomes, and Comprehensive Management
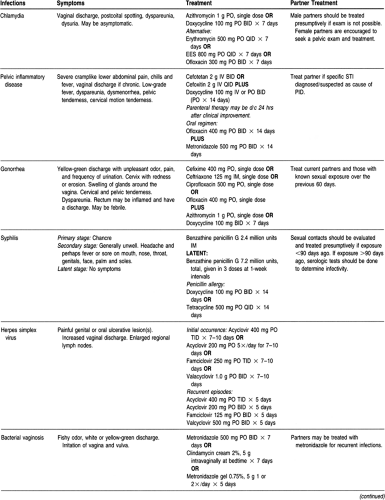
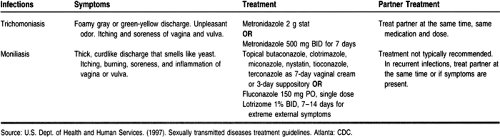
The recommended antimicrobial agent for uncomplicated urethral, endocervical, or rectal chlamydia in adults is doxycycline or azithromycin. Table 69-1 gives treatment guidelines for both chlamydia and the complication of PID.
TEACHING AND SELF-CARE
Chlamydial infection is especially prevalent among adolescents. Prevention strategies must be targeted toward young people and their sexual partners. Community-based prevention programs should target all sexually active adolescents and young adults. These can include school-based programs, adolescent recreation programs, television programs and ads, and newspaper ads. Posters and patient education materials can be placed in settings where there is a high traffic flow of adolescents and young adults. These measures can help promote increased awareness and vigilant screening and treatment. The principal goal is to prevent both overt and silent chlamydial salpingitis and PID sequelae. Prevention of perinatal and postpartal infection is also critical.
Strategies should target infection prevention. Specific strategies include:
Recommending behavioral changes that reduce the risk of acquiring or transmitting chlamydia
Advising teens to delay having intercourse, to decrease the number of sexual partners, and to use barrier contraception
Identifying and treating patients with genital chlamydial infection before they infect their sexual partners, and infected pregnant women before they infect their infants.
CLINICAL PEARL
Active screening and prompt treatment are necessary because the infections are typically asymptomatic.
Efforts aimed at preventing complications among patients found to be infected with chlamydia include careful screening to identify and treat asymptomatic infection, and treatment of the female partners of men infected with chlamydia.
CLINICAL PEARLS
Early recognition of clinical symptoms suggestive of infection, including mucopurulent cervicitis and urethral symptoms, is important. Treatment is critical for preventing complications.
Screening guidelines should reflect prevalence rates within the provider’s geographical area.
Because of the high incidence of chlamydial infection among sexually active females, the CDC’s screening recommendations include (USDHHS, 1993):
Women younger than 20 should be tested when undergoing a pelvic exam, unless sexual activity since the last test for chlamydia has been limited to a single, mutually monogamous partner.
All other women who meet the suggested screening criteria:
Mucopurulent cervical discharge Sexually active and younger than 20
Age 20 to 24 who meet either of the following criteria, or older than 24 who meet both criteria:
Inconsistent use of barrier contraception New or more than one sex partner during the last 3 months.
CLINICAL WARNING
Young men tend to seek health care less frequently than young women. When men and adolescent males present for health care, screening for chlamydia should be considered.
GONORRHEA
Anatomy, Physiology, and Pathology
Gonorrhea is transmitted almost exclusively sexually, because the gonococcus cannot survive outside the body. Sexual transmission occurs more easily from man to man or man to woman rather than the reverse. Men may have symptoms after a short incubation period of 3 to 7 days. Typically, men note urethritis and a purulent penile discharge. If left untreated, the infection may spread to the urethra, prostate, seminal vesicles, and epididymis. This may result in urethral stricture and obstructive uropathy. Proctitis may result after anal intercourse, although anal transmission is most often asymptomatic. Anoscopy may reveal punctate ulcerations and intraluminal pus. Pharyngitis may occur after oral–genital sex, although these patients are typically asymptomatic.
Conjunctivitis may occur as a result of inoculation into the conjunctiva. Lack of treatment may progress to corneal ulceration. Newborns may acquire gonococcal ophthalmia from contact with infected vaginal discharge during vaginal birth.
In females, the infection ascends to the uterus and fallopian tubes if untreated. This may lead to salpingitis and PID.
Gonococci may disseminate; this occurs more often in women than in men. Gonococcemia manifests as bacteremia, fever, chills, and characteristic hemorrhagic, painful, vesicopustular skin lesions. Frequently seen is tenosynovitis, particularly of the small joints of the hands and feet. Less common manifestations include endocarditis and perihepatic involvement (Fitz-Hugh-Curtis syndrome).
Antimicrobial resistance remains an important consideration in the treatment of gonorrhea. The resistance, caused mainly by the production of a beta-lactamase (penicillinase), affects 5% to 20% of patients in the United States. In 1995, 31.6% of isolates collected by the Gonococcal Isolate Surveillance Project were resistant to penicillin, tetracycline, or both (USDHHS, 1996). Resistance to ciprofloxacin was first identified in 1991 but remains rare (USDHHS, 1996).
Epidemiology
Infections caused by Neisseria gonorrhoeae are a major cause of PID, tubal infertility, ectopic pregnancy, and chronic pelvic pain in the United States. Epidemiologic studies provide strong evidence that gonococcal infections facilitate HIV transmission (Eng & Butler, 1997). An estimated 1 million new infections with gonorrhea occur in the United States each year. The rate
of gonorrhea has continued to decline since 1975. From 1994 to 1995, the rate decreased from 165.1 per 100,000 population to 149.5. Teens age 15 to 19 had higher rates than the general population; young adults age 20 to 24 from minority populations had the highest rates.
of gonorrhea has continued to decline since 1975. From 1994 to 1995, the rate decreased from 165.1 per 100,000 population to 149.5. Teens age 15 to 19 had higher rates than the general population; young adults age 20 to 24 from minority populations had the highest rates.
History and Physical Exam
The exam of the external female genitalia may demonstrate swelling and discharge from Bartholin’s glands. In men, the exam includes assessing for discharge and regional lymphadenopathy. The prostate should be palpated for signs of acute prostatitis (see Chaps. 68 and 70).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree