(1)
University of Linköping, Linköping, Sweden
Abstract
The possibility of situations in which available resources are insufficient for the immediate need of medical care within the health care system, defined as major incidents (MIs), has significantly increased during the last few decades, subsequent to development throughout the world, and continues to increase. Experiences from MIs since the beginning of the new millennium clearly illustrate that, regardless of where we live, we can at any time and without any warning be faced with a large number of casualties; the need for treatment highly exceeds available resources and people’s life and health depend on how well we are prepared and trained for such situations.
MIs include a wide spectrum of events, from those where all patients who can normally be rescued can be saved by adapting organization and methodology to the situation (MI level 1), to those with a large number of casualties and destroyed national infrastructure, requiring international assistance (MI level 4). However, even if the demands on triage and simplified methods vary with the extent of the incident, the basic principles of management and performance are the same.
The goal of the health care system in these situations is to eliminate or reduce avoidable loss of life and health, as well as physical and psychological suffering. This requires planning and preparedness; however, more important is for all staff involved in the rescue to have appropriate training. Because the dominating scenario so far has been physical trauma, this is a heavy responsibility, not only for the leaders, but for all staff involved in the management of traumatized patients.
4.1 Definitions
Ever since disaster medicine was established as an academic discipline, many attempts have been made to define the term disaster from a medical point of view. A wide range of definitions have been proposed and discussed, but many of these proposals have been only constructions of words and do not entail any practical function, neither as a basis for decision making in the process of alert nor as a basis for evaluating and comparing various incidents.
In order to achieve this, more practical and useful terminology originating from the term Major Incident (MI), defined as any situation where available resources are insufficient for the immediate need of medical care, has been developed during recent years for the health care sector. MI is not related to any specific number of critically ill or injured patients, or to any specific level of resources, but rather to the balance between resources and need. The term is used only in the acute situation where lack of resources can cause immediate loss of life or severe impairment of health – a “chronic” discrepancy between recourses and need that might be present within an increasing part of the present health care system is not classified as MI.
The text in this chapter is to a part based on the textbook Lennquist S. (Ed): Medical Response to Major Incidents and disasters, Springer 2012, with permission from the publisher.
The impact on the health care system is related to the MI level.
1.
MI Level 1: By adjusting organization and methodology, we can attain the level of expectation of our medical care and rescue all patients who can be saved. Alternative definitions are Major Incidents or Major Accidents, Major Emergencies, and Compensated Incidents.
2.
MI Level 2: The number of casualties is so high that even with adjusting organization and methodology we cannot attain the level of expectation, meaning that all patients cannot be saved. Alternative definitions are Mass–Casualty Incidents, Disasters, or Decompensated Incidents.
3.
MI Level 3: The same as level 2, but combined with destruction of the infrastructure in a region. This means even higher demands on triage, as well as demands on other types of support, requiring national assistance from outside the affected region.
4.
MI Level 4: The same as level 3, but affecting a country where the entire national infrastructure is impaired or where the national resources are insufficient to handle the situation and international assistance is needed. Alternative definitions for levels 3 and 4 are Complex Emergencies or Compound Incidents.
The advantage of this terminology is that it provides a direct practical base for decisions in response to the alert.
Level 1 means that disaster plans should be activated and the methodology of working adjusted to that, but the goal can still be to save all patients.
Level 2 means upgrading the degree of alert and preparedness, giving a lower priority to casualties with minimal prospects of cure to be able to save patients with a better chance of survival (i.e., use of the triage category “expectant”).
Level 3 means mobilizing national resources from outside the affected region, including support functions for supply of water, electricity, food, and temporary accommodation, and transport facilities both for evacuation of casualties and for delivery of personnel and material resources.
Level 4 has the same meaning as level 3 but on an international basis, indicating activation of international relief organizations.
When this terminology was introduced, levels 3 and 4 were combined into level 3. Recognition of incidents that can be handled nationally in spite of destroyed infrastructure and the need for clear indications for activation of international relief operations has led to the proposal for separating the last level into two separate categories (levels 3 and 4).
Most incidents in high-technology countries, or countries with good health care resources, fall under the category MI level 1. From a medical point of view, the World Trade Center terrorist attack of 2001 can be included in this category, even if, in general terminology, it has been classified as a disaster. The primary mortality on the scene was so high that there was an ambulance for every surviving casualty, and the hospital resources were more than adequate.
An example of an MI level 2 situation is the Estonia Ferry Incident in the Baltic in 1994, where in a storm and cold water the resources were sufficient enough to rescue only a limited number of passengers from the cold water, with a total of 852 casualties; the evacuation of those with signs of life was restricted, leaving hypothermic and “normally” rescuable casualties on the rafts.
Examples of MI level 3 are the floods after Hurricane Katrina in the United States in 2005 and the earthquake/tsunami disaster in Japan in 2011. Examples of MI level 4 are the tsunami disaster in the South East Ocean in 2004 and the earthquake in Haiti in 2010.
Even though an internationally uniform terminology is desirable, there will probably be variations in definitions between countries, based on differences in resources, potential scenarios, community structure, culture, and traditions. Regardless of terminology, it is important that the definitions used are not only a theoretical construction of words, but practical and useful for basing decisions and performance in such situations, and they should be well known to health care staff at all levels.
4.2 Risks of MIs in Modern Societies
It has been clearly shown that the possibility of situations where available resources are insufficient for immediate medical care has increased significantly during the past decades and continues to increase in parallel with the development of the community:
The global population has increased from 1.6 to 6 billion people during the past century, and with the current annual increase of 1.33 %, the calculated number for the year 2050 is 8.9 billion, which is a risk factor in itself.
Continuing urbanization means increasing numbers or people in crowded areas, both for permanent living and gathering for different public events. Such areas are also a potential target for terrorist actions.
Increasing movement of people, whether permanent or by travelling. As an example, of the 9 million inhabitants of Sweden, more than 400,000 are in other countries at any given time of the year, in many cases, traveling in areas known to be a focus of natural disasters and/or terrorist activity.
Production, transport, and use of hazardous material has greatly increased over the past decades; only in Sweden, 18 million tons of flammable, explosive, chemical, or toxic agents are transported over roads every year, with an additional 3 million tons transported by rail.
Hazardous material also includes radioactive substances that modern society has been increasingly dependent on for supply of energy, which involves risks that cannot be ignored.
Global terrorism has apparently come to stay, partly replacing armed conflicts. This means that at any time, at any place, regardless of active involvement in any conflict, and without warning, we can be faced with large numbers of severely injured people. The goal of the terrorists is to gain attention for their own interests, with killing being the easiest way and having the biggest effect, regardless of whether innocent people are killed.
Even if the risk for a global war has decreased temporarily, history speaks for itself, and armed conflicts are continuously occurring all over the world and will probably continue to occur, with increasing political tensions, accelerated by increasing divisions between poor and rich populations.
It is today agreed that the ongoing climatic changes have generated an escalation of so-called natural disasters and that the effects of such disasters with regard to loss of health and life have the potential to increase, subsequent to the increased global population and increased concentrations of people in limited areas.
The World Disaster Report 2007 showed a 60 % increase of occurrence of incidents defined as “disasters” during the decade 1997–2006. During that period, the reported deaths from such incidents increased from 600,000 to more than 1,200,000, and the number of affected people increased from 230 to 270 million.
Reviews of MIs occurring in the world during the past few decades clearly show that wherever we live or work in the world and however safe and peaceful the area may seem, we can at any time face a situation requiring all the knowledge and preparedness described below to be able to reduce loss of health and life, as well as suffering, of people who depend on and trust the competence of experts in this field.
For a review of recent MIs, experiences, and lessons learned, the reader is referred to text books on medical response to MIs.
4.3 Demands on Health Care in Major Incidents
Parallel to the increasing risk for MIs wherever we live in the world, we can – as a paradox – identify an increased vulnerability of our health care system to these kinds of situations.
Reduced reserve capacity because of increasing demands on efficiency, with continuous optimal utilization of all available resources
Increased dependence on advanced technology
Increased specialization, with reduced ability to deal with conditions outside one’s own specialty
The goal of the health care system during MIs is to reduce (as far as possible) or eliminate loss of life and health and physical and psychological suffering as consequences of the incident.
The following are required to achieve this goal:
Relocating of available resources to where they are most needed and rapid mobilization of additional resources (personnel and material).
Optimal utilization of available resources by accurately prioritizing between patients and diagnostic and therapeutic measures and the use of simplified methods for diagnosis and treatment.
Relocation and mobilization of resources require planning and preparedness, including a prepared structure for coordination and command, defining the positions responsible for decisions on different levels.
Optimal utilization of available resources requires education and training for all the staff involved in responding to the incident, possibly the most important part of preparedness.
Planning, education, and training require development and research within this field, as in all other fields of medicine.
4.4 Prehospital Response
4.4.1 Demands on Prehospital Response in MIs
This situation is different from the “normal accident” where an ambulance (at least within a short time) can be expected to be available for every patient needing transport, with a varying number of patients now having to wait for transport. Evacuation may be delayed by time-consuming extrication, difficulties in obtaining access to the scene, and/or lack of rescue staff in relation to the need. All these points generate a need for additional medical functions at the scene:
Leading and coordinating the medical activities at scene in conjunction with other organizations (rescue service, police);
Continuous communication with the medical coordination center (the alarm center, ambulance dispatch center, or regional medical command center, depending on local organization), reporting expected need for care, and requesting resources according to needs;
Triage on the scene (i.e., deciding in what order the patients should be treated and evacuated);
Treatment at the scene because evacuation is delayed, but also because treatment may permit lower priority for some casualties, saving ambulances for those requiring immediate hospitalization;
Transport to hospitals, with estimation of available hospital resources, which requires communication with a coordinating medical center.
These demands result in an immediate need for medical staff at the scene who (1) can lead and coordinate the work according to the above and (2) can start triage as a basis for transport priority.
Regardless of organization, these tasks are always primarily performed by the crew of the first ambulance at the scene.
Incidents with many casualties and/or delay in evacuation require additional medical staff at the scene for the tasks described above. Planning for MIs must include preparedness for them. It is important for the medical officer in command at the scene to identify such needs at an early stage so that prehospital teams can be mobilized for this function and ambulance crews can instead be utilized for transport.
4.4.2 Structural Variations Among Countries
The type of organization on the scene naturally varies among countries depending on structural differences among communities with regard to involved participants and their responsibilities, national traditions, geography and culture, economy, and political system. However, the basic principles are the same and will be described based on what is common practice in at least most European countries, but also with emphasis on where alternative ways of organization may exist. Some basic rules that are important to follow regardless of type of organization will be particularly emphasized, as well as the most common mistakes.
A concept that will be referred to, because it is frequently used in European courses in this field, is the Major Incident Medical Management and Support (MIMMS) concept, originating from the United Kingdom. It is influenced by British organization, which differs somewhat from the organization in Central Europe, but parts of it are valid for any organization and it is educationally well presented, using acronym-based poems to support memory in critical situations.
It is important that all medical personnel who might be deployed for work at the scene of MIs are familiar with their own local organization, have postgraduate education and training in the positions they may be expected to have in a MI.
4.4.3 Terminology
As the organization at the scene varies on some points between countries, there are also variations in terminology. With the aim of avoiding continuous repetition of alternative terminology, which can cause confusion, only one form of terminology will be used in the following text, explained below with mention of alternatives. Regarding organization, it is important for all medical personnel to learn and use the terminology adopted in their own country; hopefully it will be possible sometime in the future to come to an agreement on an internationally uniform terminology.
MIC
Medical Incident Commander. Leads and coordinates the medical work at the scene. Alternative term: Ambulance Incident Officer.
RIC
Rescue Incident Commander. Leads and coordinates the rescue work at the scene. Alternative term: Fire Incident Officer.
PIC
Police Incident Commander. Leads the police work at the scene.
TRO
Triage Officer. Medical officer responsible for the primary triage. The term is not used in all organizations.
ALO
Ambulance Loading Officer. Leads and coordinates transport of casualties from the scene. Alternative terms: Transport Officer, Transport Leader, Chief of Transport.
RMC
Regional Medical Command Center. Leads and coordinates the whole medical response to the incident. In some countries, this is a specially prepared function staffed by medical and administrative officers. In other countries, this function is covered by other organizations: Alarm Center, Ambulance Dispatch Center, or a defined hospital in the area, and in some countries it does not exist.
RVP
Rendezvous Point. Point where all incoming units in the rescue action are directed to stand by for access to the scene. Alternative terms: Check Point, Break Point.
4.4.4 First Unit at the Scene
4.4.4.1 The First Report
The first unit at the scene always has an important role, even more so in MIs. Regardless of what type of information has already been relayed to the coordinating center, this will be the first report from medical staff, which is of critical importance for further activation of the entire medical response chain: Mobilizing transport facilities, equipment and prehospital teams, and alerting hospitals. Delay in this report will cause a delay in the response that can have fatal consequences for the victims of the incident.
The first report is commonly referred to as “Window report”−it should not try to be complete, but is only a primary indication of how great the need for medical care is expected to be, and therefore in many cases can be based on what can be seen through the window of an arriving vehicle. Possible information at this stage may be restricted to “Many injured, probably many dead, need both medical support at scene and transport facilities”−enough to pull the trigger for MI and start activation of the medical response.
According to the MIMMS concept, the acronym-based word for the first report is METHANE:
Major incident declared (or standby)
Exact location
Type of incident
Hazards
Access
Number of casualties
Extra resources
This concept is used as standard in some countries, but is not always easy to translate into other languages. It is based on the British system where the first ambulance crew may declare a Major Incident, whereas in many countries this is the responsibility of a coordinating medical center. The difference may be of theoretical interest; the probability is that no coordinating center would object if the first arriving ambulance evaluates the situation as a MI. However, it is important that it is clearly stated in the disaster plan to which position the authority (and responsibility) to declare a MI is connected, so that confusion on this point does not delay the decision and thereby the alerting of resources.
If an MI is apparent and immediate contact cannot be established with the coordinating center, the first ambulance crew at the scene should act according to the action cards for MI (see Table 4.1) until contact has been established.
Table 4.1
Action card for medical incident commander (example)
Action card MIC |
|---|
1. Deliver window report to alarm center (rough estimation of number of casualties, estimated need of transport and medical care on scene)a |
2. Confirm MI. If MI is not already declared but apparent on arrival, inform alarm center, act according to MI until contact from RMC b |
3. Park ambulance, take on tabards for MIC and (other crew member) TRO |
4. Contact RIC (if arrived) direct or by Channel X |
Request information about: |
Estimated number of injured and dead |
Risk zones(hot, warm) and other risks at the scene |
The most urgent need of care |
Required and expected resources from rescue service |
Decide together with RIC location of casualty-clearing and ambulance-loading zones |
5. Decide if incoming ambulance crews should be retained at the scene for medical support, and if so how may and for which tasks |
6. Dispatch TRO to start primary triage according to action card |
7. Make quick survey of the scene and: |
Estimate again number and severity of casualties |
Need of support in injury zone (trapped). Identify urgent needs |
8. Decide Level of MI as guideline for medical work, inform all staff and re-evaluate this level continuously |
9. Contact RMC Channel X (if no contact with RMC, Alarm center or ADC) and: |
Deliver second report based on the information above |
Request prehospital teams to scene if needed |
Request helicopters if needed and not already alerted |
Request distribution key for transports to hospital |
10. Start transport of patients triaged by TRO. Until distribution key given, start to send severely injured according to: |
Six to Major City University Hospital |
Four to Small Town Regional Hospital |
Two to Small Town County Hospital |
11. Organize casualty–clearing and ambulance–loading zones for primary and secondary triage and dispatch teams according to that, and also teams to injury zone when needed (to risk zone = not without communication with RIC) |
12. Appoint ALO for transport coordination |
13. Repeat contacts with RMC, update reports from scene, request updated distribution keys, request additional support and equipment when needed |
14. Maintain contact with RIC and PIC, in big incidents establish Command Place |
15. Decide “MI Stand Down” on scene in agreement with RMC when all injured are evacuated. Inform RIC, PIC, and all medical staff at the scene. Lead debriefing for all medical staff before departure from scene |
4.4.4.2 Taking Command
When an MI is declared, the first arriving ambulance will not be involved in transport of casualties, but will stay at the scene. One of the officers will take the role of Medical Incident Commander (MIC) and the other, the primary role of Triage Officer (TRO) and immediately prepare the ambulance loading zone and triage the first casualties for transport to the first available ambulances.
In some organizations with very good access to ambulances, both officers in the first ambulance take administrative roles, but with such an urgent need of medical care at this stage, it is often difficult to have two administrators.
In most organizations, the ambulances are equipped with tabards labeled with the positions referred to above (Fig. 4.1). The labeling may vary between countries, but the most generally internationally accepted colors for medical staff are green and yellow. The figure also illustrates the need of personal protection clothes and is valid for all medical staff working in the field.


Fig. 4.1
The crew in the first ambulance at the scene in a major incident takes the roles of Medical Incident Commander (MIC) and Triage Officer (TRO). They wear tabards with these markings, available in all ambulances, unload medical equipment needed on the scene, and follow the action cards for these positions, also available in all ambulances (Table 4.1). Their ambulance is not used for transport but stays on the scene as a command ambulance, in some countries indicated by keeping the blue light on (From Lennquist S (ed): Medical Response to Major Incidents, Springer 2012, with permission)
The MIC should have a prepared action card for MIC telling what steps to take, and in which order (see Table 4.1). Such action cards should also be included in the equipment of all ambulances.
The acronym-based word used in the MIMMS concept to summarize the contents of the action card is CSCATTT, standing for “Command, Safety, Communication, Assessment, Triage, Treatment, Transport”. This can be good support for memory if the action card is lost or not found.
4.4.4.3 Coordination with Collaborating Agencies
The leader of the rescue operation in most countries is the officer in charge of the first fire brigade that arrives, the Rescue Incident Commander (RIC), and in some countries the officer in charge of the first police unit to arrive, the Police Incident Commander (PIC). In some countries, the rescue leader has overall command of rescue operations, whereas in others, every organization involved is on its own. This difference is mainly theoretical because no chief of rescue or police would give orders with regard to medical care, and medical staff naturally respect the advice of police and fire brigade with regard to security matters.
Regardless of organization, the RIC has authority to request any type of resource needed for the rescue work, including private property (even if he/she has to answer for it afterward).
If the RIC (in most places clearly marked with tabard and helmet [see Fig. 4.2]) has arrived at the scene before the first ambulance, one of the first steps is to establish contact, request available information (Table 4.1), request resources for medical care, and agree on location for triage and ambulance loading zones, which should be as close together as possible, but outside potential risk zones.


Fig. 4.2
Police Incident Commander (left), Rescue Incident Commander (middle) and Medical Incident Commander (right). These officers constitute the Command group at the scene and stay in continuous communication during the response, and a command place is usually established that can be at a vehicle or, in extensive incidents, in a special command wagon (From Lennquist S (ed): Medical Response to Major Incidents, Springer 2012, with permission)
The RIC, PIC, and MIC normally constitute the command group on the scene. In complex incidents, or incidents extended in time, a command center is established from where this command group can coordinate the operation.
4.4.4.4 Safety
The MIC is responsible for the safety of the medical staff, and a dead or injured medical officer is of no benefit to the victims. Communication with the RIC with regard to possible risks in the area (Table 4.1) is mandatory as a basis for dispatching medical staff onto the scene.
The rescue service commonly uses the terminology hot, warm, and cold zones:
Hot zone = risks for life and health so high that only rescue staff with special equipment and training should go in (fire, smoke, or high concentrations of hazardous material).
Warm zone = medical staff can go in, but only if they are wearing protective equipment and are trained for it (smoke or hazardous material in concentrations so low that simple protection equipment is sufficient).
Cold zone = no risks requiring special equipment or training (not excluding other risks).
In some countries, the RIC decides who is allowed to enter warm or hot zones; in other countries the MIC decides on medical staff, but should nevertheless respect the advice of the RIC.
In incidents caused by, or involving, criminal activities such as terrorist attacks, riots, or gunfire, the police are also responsible for security and making decisions with regard to which zones can be entered by rescue and health-care staff without risk of being injured from such activities.
4.4.4.5 Overview of the Scene
Before delivering the next report, the MIC should make a quick scene reconnaissance (1–3 min) to get the first medical overview of the scene and identify urgent needs of care such as need for medical support for extrication of trapped, and make a preliminary estimation of the number of severely injured. This offers a personal knowledge of the conditions at the scene, valuable as a basis for leading the work and for dispatching medical staff within the area.
In bigger incidents, the RIC usually organizes the scene in sectors (part of a building, one or more wagons in a train) with a rescue officer responsible for each sector. If there is a need for medical support at the scene, it would be wise to dispatch medical staff to make contact with the responsible rescue sector officers to obtain information and establish collaboration.
4.4.4.6 Second Report
The second report is the confirming report, coming after the first “window report”. It is important that this report come as soon as possible. At this stage, the whole medical organization, triggered by the first alert, is awaiting more information as a basis for a decision regarding the level of alert and steps to be taken within every unit. Therefore, again, there should be no details, no attempts to give the anatomical distribution of injuries, just the information that can be extracted from communicating with other units at the scene, and from the rapid reconnaissance of the area.
4.4.4.7 Decision of Strategy for the Medical Work
At this stage, the MIC should be able to estimate the relation (or discrepancy) between the need for medical care at the scene and available resources. Based on this estimate a decision about strategy must be made: Is this a situation where the normal level of medical care can be maintained with the steps:
taken as above (= MI Level 1: all potentially rescuable can be saved, what is called a compensated incident), or
Is the load of casualties so high that the standard of care must be lowered to be able to save as many as possible (= MI Level 2: decompensated incident)?
It is difficult for medical staff at the scene to obtain the overview needed to make such judgments and this is therefore the task of the MIC. Decisions with regard to strategy should be clearly communicated to all the staff involved as a guideline for triage and can be changed, depending on incoming resources or initially undiscovered needs.
4.4.4.8 Establishing Continuous Contact with the Regional Medical Coordinating Center (RMC)
After following these first steps on the action card, the MIC should take a position where he/she is not involved in medical care or decisions with regard to triage and establish repeated contacts with the RMC to:
Request information on hospital capacity
Request additional support at the scene if needed (transport resources, equipment, staff)
Report casualty load at the scene and departed transports
4.4.5 Building up the Structure at the Scene
4.4.5.1 The Need for Simplicity
As stated in Chap. 1, simplicity is the key to successful management of MIs and that is valid also for the operations at the scene. It should be remembered that the majority of MIs occur in densely populated areas with good access to ambulances and short distances to hospitals. The first ambulance is often at the scene within 5–15 min after the alarm and then the medical work begins, and with many ambulances within close range, the evacuation from the scene can (and should) start a few minutes later.
This does not allow time for building up a complex organization. Schedules of organization that are too complex with too many boxes, too many levels of command and decision, and too many ranks and titles, will involve a risk that “the war is over” before the organization is built up.
It is an understandable temptation to transfer experiences from a military organization to a civilian one because military personnel are (and must be) good organizers, using a clear and strict hierarchy. However, there are significant differences between the civilian MI and the combat situation with regard to (1) time for preparation, (2) demands on endurance:
A war rarely commences without warning, which allows for a long preparation time. However, the organization must have the ability to run on a high capacity for a long time, days, weeks, months, or even years.
An MI in peace time in a civilian community, on the other hand, occurs at any time, without any warning at all, and within a few minutes, an organization fully occupied with routine medical care must have the ability to deal with a number of severely injured, far exceeding available capacity, regardless of whether any of the available staff has any experience of such situations. However, the peak of the casualty load usually passes within a few hours (exceptions exist, of course).
This means higher demands on existing facilities than in the combat situation. There is no time to build up a new organization, only to adapt the existing organization to the specific demands of the MI.
4.4.5.2 The First Step: Starting Triage and Transport
The tasks of the first medical unit at the scene have already been described, illustrating that one of the officers in the first unit will be fully occupied with the important role of MIC.
At the same time, it is of critical importance that the transports to hospitals begin as soon as possible – “no fully staffed ambulance should be standing waiting”, and the sooner they get moving, the sooner they come back.
Therefore, the triage process must start as soon as there are ambulances at the scene, and this is the reason to use the second officer in the first ambulance as primary triage officer = TRO.
The first step in organizing relief work, based on the presence of only one ambulance staff, is illustrated in Fig. 4.3. The TRO sorts the patients into three routes of evacuation: (1) Should go with the first available ambulance, (2) needs ambulance but can wait, and (3) injured but without need of ambulance transport. A very simple system should be used for this primary triage, for example Triage Sieve (see below under triage).
Fig. 4.3
The organization on scene is built up step by step, the first step when the first ambulance arrives. The Triage Officer (TRO) makes only a simple primary triage and sorts the patients according to three routes: (1) Severely injured, can go with available ambulance, necessary resuscitation done by ambulance crew. (2) Need ambulance transport, but can wait. (3) Do not need ambulance transport. The Medical Incident Commander (MIC) at this stage has the role as transport coordinator and decides the destination for the first patients. RVP Rendezvous Point (From Lennquist S (ed): Medical Response to Major Incidents, Springer 2012. Artwork Lats-Ake Pettersson, with permission)
In this phase, the MIC may also have the role of transport coordinator and direct available (staffed) ambulances to hospitals. The principles for the distribution between hospitals are described below under “Transport”.
As soon as casualties in route (2) begin to accumulate, or need surveillance, additional medical staff at the scene is mandatory and that is the task of the MIC. Thereby the organization is transferred to the next step.
4.4.5.3 The Second Step: Completing Casualty and Ambulance Loading
There is now access to additional medical staff at the scene, either ambulance crews from arrived ambulances or deployed prehospital teams (they usually take longer to arrive on the scene).
This means that the second route of evacuation goes to one or more teams for secondary triage, including measures of resuscitation needed before transport (Fig. 4.4). Two staff members in each such team are preferable to, for example, one ambulance crew, or a prehospital team with a physician and a nurse. For this secondary triage a system with better discriminative capacity than Triage Sieve is recommended, for example Triage Sort (see below under “Triage”).
Fig. 4.4
When it is apparent that there are additional patients needing ambulance transport than there are available ambulances, the organization is extended with a second step: Patients who are not ready to depart, or cannot depart because of lack of available ambulance, now follow line (2) to teams devoted to necessary resuscitation/treatment and secondary triage before transport. An additional medical officer/team surveys patients waiting for transport, and another is dispatched for secondary triage/survey of patients estimated not to need ambulance transport. The Medical Incident Commander is now replaced by another ambulance officer having the role as Ambulance Loading Officer (ALO) (From Lennquist S (ed): Medical Response to Major Incidents, Springer 2012. Artwork Lats-Ake Pettersson, with permission)
If there is congestion in the evacuation area and no immediate access to ambulances for high priority patients, staff are needed to attend to and help casualties awaiting transport (Fig. 4.4).
At this stage, evacuation of casualties not needing ambulance transport should also be begun, and they must be examined and re-triaged by medical staff before departure (Fig. 4.4).
The MIC should be released to assume the position of transport coordinator as soon as possible and replaced by another ambulance officer (ALO, Fig. 4.4).
4.4.5.4 The Third Step: Completing the Organization at the Scene
The Injury Zone
As mentioned above, the need for medical support in MIs is usually not restricted to the casualty-clearing and ambulance-loading zones, even if, as a general principle, the work should begin there to have the transport going as soon as possible. There may also be an urgent need for resuscitation and triage where the injured are located, the injury zone (Fig. 4.5) and may be in the wreck after an airplane, rail, or bus crash; in a collapsed building; or in an area of explosion. One of the objectives of the rapid overview of the scene performed by the MIC immediately upon arrival is to identify such needs and deploy staff to the location as soon as possible. Note that there can be risk zones (see above) within the injury zone; do not deploy staff there without communicating with the RIC.
Fig. 4.5
The organization at the scene in a greater incident completely built up (see further the text) (From Lennquist S (ed): Medical Response to Major Incidents, Springer 2012, Artwork Typoform, with permission)
Non-injured People
People who survive an MI without physical injuries are also victims. Exposure to a situation like this is a severe psychological shock for most people, and even if the reactions are not apparent immediately, they may appear later. In addition, many of the non-injured people may have lost contact with friends and relatives, or seen them killed or injured, and they may have lost their property and/or be far from home. This group of people cannot just be sent away, but need to be taken care of.
Additionally, the same considerations are valid with regard to potential severe injuries here as for the group primarily triaged as “less severely injured” (see below): They should also be examined by a medical officer, if possible, before departing from the scene.
The police have the responsibility of taking care of those who were not injured. They must be registered and taken to a prepared zone where they can be given protection and obtain transport to a location where they can get psychosocial support, information with regard to lost friends and relatives, and help with further transport (Fig. 4.5).
The Dead at the Scene
Management of dead victims on the scene is the responsibility of the police. In most countries, only doctors are allowed to declare patients dead, unless death is apparent: Head separated from the rest of the body or the patient totally crushed or burned. Victims who are apparently dead should be left where they are found to facilitate identification and investigation by the police. For management of the dead, the reader should consult text books on medical response to MIs.
Other casualties without any signs of life should be labeled as low priority patients until they can be examined by a doctor and death confirmed. Note the hazard of differentiating between hypothermia and death: In a cold environment, no one should be declared dead until warm and dead! For triage and management of hypothermic casualties, the reader should consult text books on medical response to MIs.
Helicopter Landing Area
Helicopters are a useful resource in MIs, not only for evacuation of casualties (see below under “Transport”) but also for transport of equipment and staff to the scene. In incidents where the benefit of helicopters is apparent and there is access to them, they should be alerted early for this purpose, and a helicopter landing area prepared and clearly marked out. It should be located at such a distance from the casualty-clearing zone that ambulance transport to the helicopters is not necessary, but not so close that it disturbs the work in the casualty-clearing zone (a distance of approximately 50 m is recommended for standard helicopters).
Cordoning Areas Off and Traffic Control
The first task of the police is to cordon off the area to prevent access to all traffic not involved in the rescue action.
If all rescue and transport vehicles arriving at the area should proceed into it, it would soon create a congested and chaotic situation where no vehicle can move. One of the first tasks of the incoming rescue leader is to decide a check–point or rendezvous point (RVP) in conjunction with the police: A place easy to identify on the map, well connected to routes for both entrance and evacuation, and with space enough to park waiting vehicles.
This point is often decided already before arrival of rescue units, based on local knowledge of the area, and information about it should be forwarded to all alerted units. Traffic control at this point should be handled by the police.
Figure 4.5 illustrates the principles for a fully developed organization at the scene of an MI, with many injured and need of medical support both in the injury zone and in the casualty-clearing and ambulance-loading zones. The figure illustrates a scene with immediate access to a road which is the case in most, but not all, MIs. Long distances from the injury zone to a road require off-road transport between casualty-clearing and ambulance-loading zones, which puts even higher demands on the rescue organization.
Inflatable tents can be life-saving measures in severe climatic conditions with delayed evacuation, but also involve a potential risk of congestion: They give the impression of being in a field hospital with a temptation to extend the treatment to more than is absolutely necessary before transport, which may create a congestion of waiting patients and also non-utilized ambulances (Fig. 4.6). If tents are used, it is of vital importance that the structure and principles of working as described above are maintained.
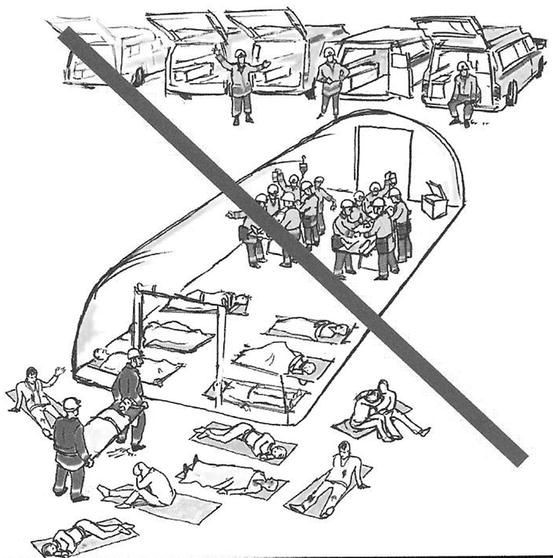
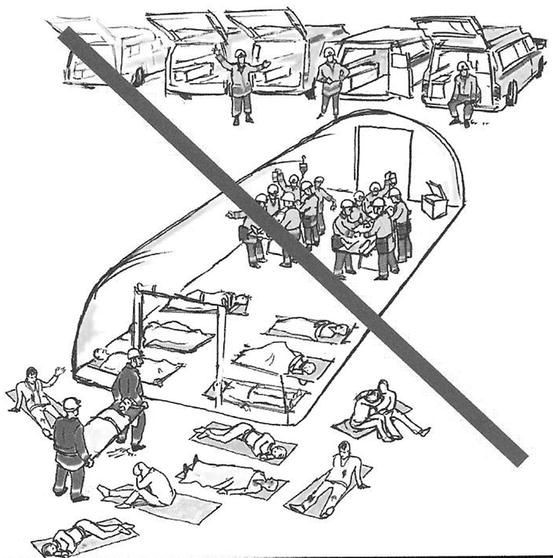
Fig. 4.6




The use of inflatable tents for protection of casualties and staff may be necessary in extreme climatic conditions and delayed evacuation. Even if such tents are used, it is important to maintain the simplicity of the structure and not fall for the temptation to overdo treatment with the feeling of being in a field hospital. What, as seen in this figure, could also be the effect of exercises performed without real times, giving the impression that everything can be done without consuming any time (From Lennquist S (ed) (2012) Medical response to major incidents. Springer, Artwork Lats Ake Pettersson with permission)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








