Procedural Sedation and Analgesia
Robert J. Vissers and James R. Miner
The care of patients with painful conditions and the performance of painful diagnostic and therapeutic procedures are routine aspects of emergency care. Approximately half of emergency department (ED) visits are for pain-related chief complaints. Many of these conditions are also associated with anxiety. Accordingly, procedural sedation and analgesia (PSA) has become a fundamental skill of emergency physicians and an important part of emergency medicine residency training (1).
Despite the emphasis on PSA, oligoanalgesia has been well described in emergency care. Inadequate pain control has been ascribed to underestimation of patient pain, concern for patient safety, fear of delays associated with oversedation, and the alteration of physical findings (1,2). PSA can improve quality of care and patient satisfaction through the relief of pain and anxiety and the facilitation of therapeutic or diagnostic procedures such as cardioversion, incision and drainage of abscesses, tube thoracostomy, lumbar punctures, fracture reduction, complex suturing, and imaging studies (1,3–5). Many drugs used for sedation and analgesia have the potential to cause respiratory, cardiovascular, and central nervous system (CNS) depression. The introduction of protocols using shorter-acting, more effective drugs, the development of noninvasive monitoring devices, and published clinical policies for PSA have made it an extremely safe, practical procedure. The airway and critical care expertise of emergency physicians make them ideal providers of safe PSA (1).
The wide variety of procedures and patient types requires the ability to individualize PSA. This can be achieved only through a comprehensive understanding of the drugs used and by proper patient assessment. Protocols delineating staffing responsibilities, monitoring guidelines, medications, observation periods, and discharge criteria and instructions are recommended before implementing PSA in the ED.
DEFINITIONS
The term conscious sedation has previously been used to describe the process of providing analgesia, sedation, and amnesia for patients undergoing painful procedures. However, this term may be misleading. A more precise and preferred term is PSA. In a recent clinical policy published by the American College of Emergency Physicians, PSA was defined as a technique of administering sedatives or dissociative agents with or without analgesics to induce a state that allows the patient to tolerate unpleasant procedures without undue pain or anxiety while maintaining cardiorespiratory function. PSA is intended to result in a depressed level of consciousness that allows the patient to maintain oxygenation and airway control independently and continuously (1).
The Joint Commission on Accreditation of Healthcare Organizations (JCAHO), in its 2003 Comprehensive Accreditation Manual for Hospitals, states that “the standards for sedation and anesthesia care apply when patients receive, in any setting, for any purpose, by any route, moderate or deep sedation and general, spinal, or other major regional anesthesia” (6). JCAHO has adopted the American Society of Anesthesiologists (ASA) definitions of sedation and analgesia created in 1999 to better describe the continuum of sedation and analgesia. Moderate sedation most closely approximates the replaced term conscious sedation.
Minimal sedation is primarily anxiolysis for a procedure, during which patients respond normally to verbal commands. Ventilatory and cardiovascular function remains unaffected.
Moderate sedation/analgesia is a drug-induced depression of consciousness during which the patient responds purposefully to verbal commands, alone or accompanied by tactile stimulation. Typically, no interventions are required to maintain a patent airway. Spontaneous ventilation is adequate, and cardiovascular function is maintained; therefore, this is associated with less respiratory depression than deep sedation. At this level of sedation, patients generally are amnestic, even to painful procedures, but moderate sedation should be used only when the procedure is likely to be successful on a more responsive patient rather than a deeply sedated patient (7–9).
Deep sedation/analgesia is a drug-induced depression of consciousness during which patients cannot be easily aroused but respond purposefully following repeated or painful stimulation. Assistance may be needed to maintain a patent airway, and independent ventilation may be inadequate. Cardiovascular function is usually maintained. This level of sedation is associated with a greater degree of respiratory depression than moderate sedation but is often necessary for the successful completion of procedures for which patient relaxation and amnesia is required (9–11).
General anesthesia is a drug-induced loss of consciousness during which patients are not arousable, even by painful stimulation. Independent ventilatory function is often impaired, and ventilatory and airway support is often required. Cardiovascular function may be impaired.
The response to medications can vary greatly between individuals and may be unpredictable. Therefore, it is recommended that clinicians be competent in the skills required to manage patients at least one level greater than the intended sedation (12). The management of impaired ventilatory function is a usual part of the practice of emergency medicine and represents a critical skill for the management of procedural sedation in the ED.
ED EVALUATION
Careful patient selection is necessary to provide safe and effective PSA. The comorbid illness or injury, any underlying medical problems, patient age, the procedure, and the ability to manage the airway are important considerations in determining the indication for and the method of PSA. Not all patients or procedures are appropriate candidates for PSA and may be best served in the operating room.
The agents used in procedural sedation, to some degree, all cause hypoventilation and diminished airway reflexes. The principle complication of procedural sedation associated with significant morbidity is aspiration pneumonia from the loss of airway reflexes (3,13–15). Luckily, this is a rare complication, but a principle goal of sedation must be to avoid situations where a patient is at risk of its occurrence. Other complications include hypoxia, hypotension, and paradoxical agitation reactions from the sedative agents.
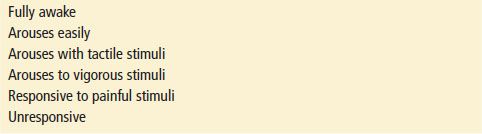
A patient’s physical status can be conveniently described using the ASA’s classification (Table 17.1) (16). This is frequently incorporated into the documentation of the preprocedure assessment. Patients with ASA physical status scores of 3 and 4 are more likely to have complications from hypoventilation and hypotension than patients with scores of 1 and 2, and the risk/benefit ratio of performing PSA in these patients must be considered (17).
TABLE 17.1
American Society of Anesthesiologists Physical Status Classification
A history of prior problems with anesthesia or PSA should be elicited. Particular attention should be paid to underlying hypovolemia, cardiorespiratory diseases, neurologic diseases, medications, and intoxicants. Physical examination should focus on the cardiovascular, respiratory, and neurologic systems and performing an assessment of airway difficulty. There is no evidence to support the need for specific diagnostic testing before PSA. A discussion including the risks, benefits, and potential side effects of PSA should take place before the procedure. Written consent is recommended when possible; however, patient condition may preclude this (12).
There is insufficient literature to recommend a necessary period of fasting prior to PSA. The combination of vomiting and loss of protective reflexes during PSA causing aspiration is considered to be a rare event (13). There is no evidence that gastric emptying or antacids reduces the incidence of PSA-associated complications. It is likely, however, that increasing depth and duration of PSA is associated with an increased risk of aspiration, and it may be beneficial in patients who have recently taken more than clear liquids and require nonurgent procedures to delay until 3 hours after the last oral intake. For patients needing a procedure urgently (fracture reductions, intractable pain, etc.) recent intake should be considered in the choice of the target sedation level and duration of the planned PSA. The complimentary use of local anesthesia when appropriate, such as a regional block, can reduce the amount of sedation required. Patients at high risk for aspiration may benefit from the lightest level of sedation for the shortest amount of time that will allow successful completion of the procedure. Recent food ingestion is not a contraindication but rather a consideration when choosing the targeted level of sedation (13,17,18).
KEY TESTING
• Interactive monitoring
• Airway assessment
• Physical status score
• Procedural plan
• Sedation plan
• Mechanical monitoring
• Capnography
• Pulse oximetry
• Cardiac monitor
• Blood pressure
ED MANAGEMENT
Preparation
The necessary equipment and supplies should be gathered in an appropriate setting prior to the initiation of PSA. There does not have to be a specific dedicated area for PSA. However, the capability to provide cardiovascular and respiratory support and availability of personnel may dictate the location. Monitoring equipment, oxygen, suction, advanced life support equipment and medications, a bag-valve-mask, and intubation equipment must be readily available. IV access should be established and maintained before PSA with IV agents. The antagonists naloxone and flumazenil should be available when opioids and benzodiazepines are being used (19).
The Joint Commission and compliant institutions insist that the PSA provider demonstrate adequate training to administer the agents effectively and safely and have the skills to manage all potential complications (6). These are all within the scope of the emergency physician’s expertise, especially in the unpredictable setting of the ED, which is unique to the practice of emergency medicine. There is no clear guideline in the literature or organizational policies regarding the required number of support personnel. It is essential that an individual is present who is capable of recognizing the respiratory and hemodynamic responses to the medications and is able to perform interactive monitoring without interruption throughout the procedure. The performance of a procedure often precludes the continual clinical assessment of the patient. Therefore, one individual provider not performing the procedure is usually recommended to monitor and document patient status when providing deep sedation (15). Moderate sedation using a single provider has been described (20).
The use of supplemental oxygen during PSA is somewhat controversial. Although its routine use may prevent hypoxemia in some patients, there is concern that it will delay the recognition of respiratory compromise and hypercarbia, due to its effect on the sensitivity of pulse oximetry to changes in ventilation (21,22). Evidence supports the use of supplemental oxygen in patients undergoing PSA to reduce episodes of hypoxia; but care must be taken to use monitoring modalities other than pulse oximetry, such as close interactive monitoring, when supplemental oxygen is used (11,23).
Monitoring
The most important aspects of monitoring during PSA are the interactive observation and assessment of physiologic changes and the level of consciousness. The patient’s ability to follow commands and the response to varied levels of stimulation are useful in quantifying the level of consciousness. Direct observation of the patient’s airway and breathing (interactive monitoring) are likely to be the most accurate monitors of a patient’s ability to maintain adequate ventilations and airway protection and to assess the safety of giving further medication to patients who have not yet achieved the desired level of sedation, and are therefore critical to the safe titration of sedatives and the avoidance of oversedation and its associated adverse effects (15,24,25). Interactive monitoring can be augmented by blood pressure, oxygen saturation, capnometry, and cardiac rhythm monitors.
The use of pulse oximetry is widely recommended in national and institutional PSA guidelines. Many studies have demonstrated its utility in monitoring oxygenation; however, there is no clear demonstration that its use during PSA affects patient outcome other than decreasing episodes of transient hypoxia (1,26). This may be as a result of the extremely low risk of morbidity and mortality during PSA when the patient’s respiratory efforts and level of consciousness are clinically monitored. Furthermore, the clinical significance of transient decreases in oxygen saturation is not known (26), but we at least assume it is a marker of ventilatory depression and therefore a marker of risk for aspiration. Pulse oximetry measures oxygenation, not ventilation. A patient breathing supplemental oxygen may not exhibit changes in the oxygen saturation until several minutes after the onset of hypoventilation. In a patient breathing room air with a normal oxygenation prior to PSA, however, decreases in oxygenation correlate with decreases in ventilatory effort. In either case, it represents useful information and should be utilized during PSA. However, it should not be a substitute for continuous clinical assessment.
Capnometry can be used to monitor ventilation. Capnographs measure expired CO2 and display a waveform that represents the patient’s ventilation. The peak of each wave represents the end-tidal CO2, or the maximum concentration of CO2 in the expired air. Large changes in the end-tidal CO2 values and in the shape of the waveform have been associated with respiratory depression in sedated patients and may allow earlier identification of hypoventilation than oximetry (21,22,26,27). An increasing end-tidal CO2 value can represent CO2 retention from hypoventilation. A decreasing end-tidal CO2 value can represent hyperventilation and decreasing arterial CO2 levels, or increased mixing of room air and expired air in the upper airway owing to airway obstruction. An absent waveform on the capnograph can represent apnea or possibly upper airway obstruction if respiratory effort is present. The earlier detection of hypoventilation associated with the use of capnographic monitoring has been shown to decrease episodes of hypoxia during procedural sedation in the ED (26). Capnographic monitoring of end-tidal CO2 improves the detection of hypoventilation, even in patients receiving supplemental oxygen, and decreases episodes of hypoxia. It should be considered in patients undergoing deep sedation who are receiving supplemental oxygen.
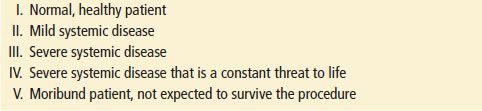
Blood pressure, heart rate, and respiratory rate should be assessed at regular intervals throughout PSA. Patients are at the highest risk for complications when they are at their deepest level of sedation, primarily within 90 seconds to 3 minutes of receiving IV sedatives, and when noxious stimuli are removed (immediately after the procedure). Continuous electrocardiographic monitoring is not routinely recommended. However, it should be used in older patients or those with a history of cardiovascular or pulmonary disease. Documentation of the level of sedation can be quantified using a predefined sedation score, such as the Aldrete score or a simplified version suggested in Table 17.2.
TABLE 17.2
Assessment of Sedation