
Cervical Spine Fractures
William R. Mower and Jerome R. Hoffman
Each year, U.S. emergency physicians evaluate nearly 1 million patients for cervical spine injury (CSI). Two to three percent of these patients actually have spine injuries, including nearly 11,000 who suffer catastrophic injury and permanent paralysis. Lifetime medical care exceeds $3 million per injury victim, and the cost of annual nationwide care for these patients exceeds $2 billion (1). Medical costs reflect only a portion of the burden produced by catastrophic cervical spine injuries. Affected patients also encounter severe limitations on activity and mobility, loss of income, productivity, and independence and increased rates of medical illness, depression, and suicide (1–3).
CLINICAL PRESENTATION
CSI most frequently occurs after blunt trauma and is often accompanied by other significant injuries, particularly head injury. CSI may be severe and life threatening and may require immediate attention (1). Conversely, unstable CSI can present with subtle clinical findings. Though truly occult injury rarely if ever occurs, patients may be unaware of a serious neck injury if they are intoxicated, have another painful injury that distracts their attention, or have an altered level of alertness that impairs their ability to appreciate the spine injury (4). Though CSI should be suspected in the setting of new-onset neurologic impairment, a normal neurologic examination does not preclude a serious and potentially unstable spine injury (4).
Classification Based on Mechanism
The specific injuries associated with a given force reflect compressive, tensile, and rotatory stresses generated by the force. In general, compressive forces produce failure (fracture) in osseous elements, whereas distractive or tensile forces can result in failure of either ligament or bone, depending on the strength of the involved bone and the rate of loading (ligamentous failure is more likely at high rates of loading) (5). For example, forced flexion generates compressive stress along the anterior spine and posterior tensile or distractive stresses. The anterior compression can produce mechanical failure of the vertebral body resulting in wedge compression and flexion teardrop fractures, whereas the posterior tensile forces can cause stretching and tearing of the posterior ligament complex, as seen in anterior subluxation, or failure across the spinous process, as found in clay shoveler’s fractures. Severe flexion forces may destroy the entire posterior ligament complex, obliterate all middle and anterior support, and produce bilateral interfacetal dislocation (6).
Hyperextension and lateral flexion also produce forced curvature of the spine, generating compressive stresses along the concave side of the curvature and tensile stresses along the convexity. Alternatively, pure vertical compression generates only compressive stresses, whereas some combined actions (rotation coupled with hyperflexion or hyperextension) produce relatively complex force distributions. Each of these mechanisms generates specific stress patterns and is associated with a particular family of injuries (5,6).
It is not possible to classify all CSIs in terms of specific applied forces. Injuries involving the occipital articulation and atlantoaxial complex, such as occipitoatlantal and atlantoaxial dissociation, as well as fracture of the dens, appear to have multiple etiologies (5,6). These injuries indicate the application of significant forces capable of producing other spine injuries and should prompt a careful search for additional lesions.
Classification Based on Stability
Functionally, the spine is considered stable if it is able to support physiologic loads without developing displacement or structural changes that cause irritation of the spinal cord or nerve roots or incapacitating deformity or pain (5). Although this definition is relatively straightforward, determining the stability after specific spine injuries can be extremely difficult. Consequently, general principles have been developed to aid in assessing stability (5).
The two-column concept of the spine is particularly useful in understanding pathophysiology and assessing stability of injuries to the lower cervical spine (base of the second cervical vertebra through first thoracic vertebra) produced predominantly by flexion or extension. This construct divides the spine into anterior and posterior columns based on anatomic elements. The anterior column consists of the posterior longitudinal ligament and all anatomic elements anterior to it, including the vertebral body, annulus fibrosus, intertransverse ligaments, and anterior longitudinal ligament. The posterior column consists of all elements posterior to the posterior longitudinal ligament, including the facet and capsular ligaments, the lamina and ligamentum flavum, and the spinous process and interspinous and supraspinous ligaments (5). Biomechanical studies demonstrate that clinical stability is preserved if all of the elements from one column and any single element from the other column remain intact (i.e., all of the anterior elements plus one posterior element or all of the posterior elements plus one anterior element) (7,8).
The two-column concept is not useful in assessing stability for injuries involving the occipital articulation and atlantoaxial complex, and it is of limited utility in assessing injuries associated with lateral flexion (5,6). With a very limited number of exceptions (fractures to the posterior arch of atlas, small avulsion fractures of the anterior arch, and type I dens fractures), consultation with an experienced spine specialist is recommended to determine the stability of these injuries.
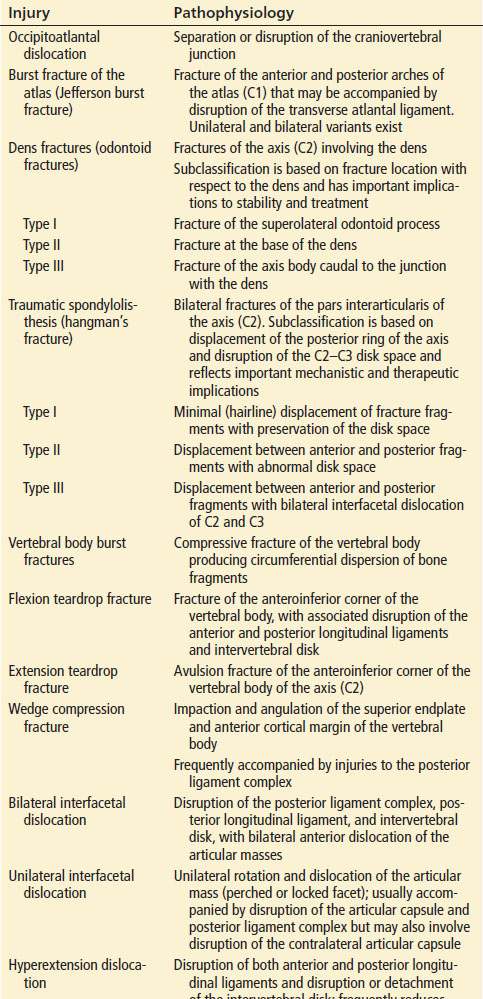
Table 28.1 summarizes the injury mechanism and clinical stability associated with common cervical spine injuries. This table presents a conservative interpretation of clinical stability in that many of the injuries described as unstable may actually have stable variants, but the detailed considerations required for a definitive assessment are beyond the scope of this text. Consultation with an experienced spine specialist is recommended in cases of uncertainty. Table 28.2 describes the specific injuries that characterize common cervical spine fractures.
TABLE 28.1
Injury Mechanism and Clinical Stability of Common Isolated Cervical Spine Injuries
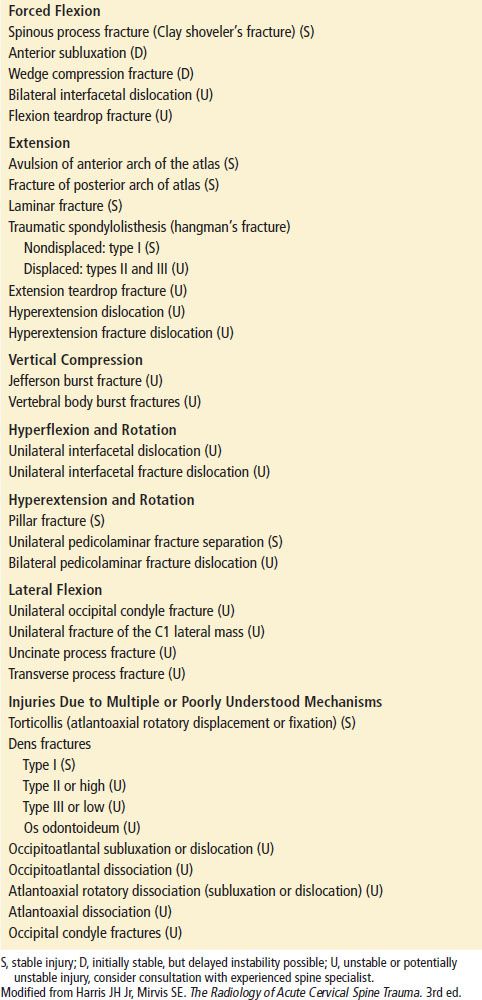
TABLE 28.2
Pathophysiologic Lesions Associated with Common Cervical Spine Injuries
DIFFERENTIAL DIAGNOSIS
Neck pain and tenderness are common findings among trauma patients, but significant CSI is rare. Most patients have minor strains and contusions that require no specific therapy. As such, it is not necessary to identify specific soft tissue injuries in most cases but rather to exclude serious injuries that could result in permanent dysfunction or catastrophic disability.
Injury to the spine and spinal cord should be suspected in any trauma patient presenting with a new-onset neurologic deficit. At the same time, it is important to recognize that these same deficits can be due to a variety of other etiologies outside the cervical spine, such as vascular injury, intracranial injury, lower spine injury, or injury to one or more peripheral nerves (4,6). Respiratory distress in blunt trauma patients may also be due to a variety of causes, including upper CSI. The neck contains a remarkable number of vital structures, including the spinal cord, carotid and vertebral arteries, jugular veins, trachea, and esophagus. All are susceptible to injury and may produce pain indistinguishable from that produced by CSI. It is important to note that trauma patients frequently have multiple injuries, and identifying a specific injury does not preclude the presence of other injuries. Spine injuries in particular provide evidence of significant axial forces and should prompt clinicians to evaluate affected patients for secondary CSIs as well as injuries to other axial elements, including the lower spine.
ED EVALUATION
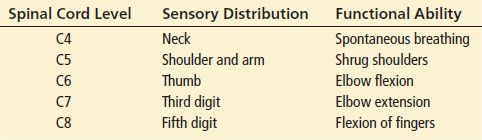
Once vital functions have been ensured, blunt patients should undergo a meticulous examination to detect other injuries and ascertain baseline function. Patients should be assessed for mental status changes that may limit the reliability of clinical evaluations. Careful attention should be placed on assessing the face and calvarium. Many of the force vectors that cause CSIs originate in the head, and meticulous evaluation may disclose such injuries as well as provide information relating to potential spine injuries. The neck and spine should be examined to detect areas of pain and swelling. A detailed neurologic examination is essential and should include an assessment of reflexes and pathologic findings associated with spine injury (bulbocavernosus reflex, priapism, decreased rectal tone). Sensory innervation follows dermatomal distributions and is particularly helpful in localizing lesions in patients with cord injuries (Table 28.3). Similarly, deficits in motor function are associated with specific nerve root levels and may also prove informative in determining injury levels (Table 28.3). Any patient with suspected spine injury should also undergo a careful evaluation of the remaining axial anatomy.
TABLE 28.3
Sensory and Motor Examination
Because CSI can be permanent and devastating, all trauma patients should be evaluated for potential CSI. Radiographic imaging provides the definitive means of assessment but is unnecessary in many cases. Clinical assessments based on decision guides such as the NEXUS low-risk criteria (4) and Canadian C-spine rule (CCR) (9) allow clinicians to identify patients who are at very low risk of CSI and can be safely spared the expense and radiation exposure associated with imaging. Although these instruments reliably detect injury (high sensitivity) and preclude injury in patients deemed “low risk” (high negative predictive value), they exhibit poor positive predictive value, and the majority of “non–low-risk” patients do not have a CSI.
The NEXUS criteria are based on five historical and physical examination findings. Patients are at low risk and may safely be spared radiographic imaging provided they exhibit all of the following criteria: (a) no posterior midline cervical spine tenderness, (b) no evidence of intoxication, (c) normal level of alertness, (d) no focal neurologic impairment, and (e) no distracting painful injuries. The criteria are subject to interpretation by individual physicians. Although they are not precisely defined, each criterion is further clarified as follows (10).
• Midline posterior bony cervical spine tenderness is present if the patient complains of pain on palpation of the posterior midline neck from the nuchal ridge to the prominence of the first thoracic vertebra or if the patient has pain with direct palpation of any cervical spinous process.
• Patients should be considered intoxicated if they have either of the following: (a) a recent history by the patient or an observer of intoxication or intoxicating ingestion or (b) evidence of intoxication on physical examination such as odor of alcohol, slurred speech, ataxia, dysmetria or other cerebellar findings, or any behavior consistent with intoxication. Patients may also be considered to be intoxicated if tests of bodily secretions are positive for drugs (including but not limited to alcohol) that affect level of alertness.
• An altered level of alertness can include any of the following: (a) Glasgow Coma Scale (GCS) score of 14 or less; (b) disorientation to person, place, time, or events; (c) inability to remember three objects at 5 minutes; (d) delayed or inappropriate response to external stimuli; or (e) other evidence of cognitive impairment or altered alertness.
• Any focal neurologic complaint (by history) or finding (on motor or sensory examination).
• No precise definition for distracting painful injury is possible. This includes any condition thought by the clinician to be producing pain sufficient to distract the patient from a second (neck) injury. Examples may include, but are not limited to (a) any long-bone fracture, (b) a visceral injury requiring surgical consultation, (c) a large laceration, degloving injury, or crush injury, (d) large burns, or (e) any other injury producing acute functional impairment. Physicians may also classify any injury as distracting if it is thought to have the potential to impair the patient’s ability to appreciate other injuries; conversely, no injury should be considered distracting in a given patient simply because it is frequently so among a group of patients. Thus, not all fractures are distracting; it is as always a matter of judgment for the clinician to decide whether a given injury is likely to impair a given patient’s ability to appreciate other (e.g., cervical spine) injuries.
The CCR excludes patients from risk classification if they (a) are younger than 16 years, (b) have a GCS score <15, (c) have grossly abnormal vital signs, (d) were injured more than 48 hours previously, (e) have penetrating trauma, (f) present with acute paralysis, (g) have known vertebral disease (ankylosing spondylitis, rheumatoid arthritis, spinal stenosis, or previous cervical surgery), as determined by the examining physician, (h) are returning for reassessment of the same injury, or (i) are pregnant (9).
According to the CCR, among patients suitable for risk classification, imaging is mandatory for those aged 65 years or greater, those with a dangerous mechanism of injury (fall from a height of 3 ft or greater, or 5 stairs; axial load to the head such as from diving; motor vehicle collision involving speed of 100 km/h or greater; motor vehicle accidents involving rollover, ejection, or a recreational vehicle; or a bicycle collision). Patients who do not meet these high-risk criteria require further risk assessment based on range of neck motion. Prior to assessing range of motion, clinicians must first determine whether a patient can safely undergo rotational assessment. Patients for whom rotational assessment can be safely completed include (a) those with a rear-end motor vehicle collision (excluding those pushed into traffic, those hit by a large vehicle such as a bus or truck, and those hit by high-speed vehicles); (b) those in a sitting position in the ED; (c) patients who were ambulatory at any time; (d) patients whose neck pain was delayed in onset (neck pain not immediately following event); or (e) those who have no midline cervical spine tenderness. Imaging should be obtained on patients who cannot safely undergo assessment of range of motion, as well as all patients who are unable to actively rotate neck 45 degrees to the right and left (9).
Patients who fail to meet low-risk classification based on clinical assessment, should undergo imaging that is individualized according to the patient’s clinical presentation and potential for CSI. Plain radiographs frequently fail to identify important cervical spine injuries, and are not highly sensitive for CSI—including for some clinically important injuries—so they should not even be considered in patients with at least a moderate prior probability of injury. These include the elderly (in whom it is often difficult to evaluate plain films because of the common presence of concomitant osteoarthritis), those in whom any movement is impossible or contraindicated, those already scheduled for computed tomography (CT) scanning for some other reason, and those with a truly high prior probability of injury (11). On the other hand, in a reasonably young patient who requires imaging merely because of failure to meet low-risk criteria, but in whom the prior probability of CSI is truly low, and it is likely that clearly interpretable plain films can be accomplished, an adequate three-view series has an extraordinarily high-negative predictive value if it can be read as clearly negative (12).
Noncontrast CT provides the most definitive means of evaluating the bony cervical spine and is the current standard for evaluating the cervical anatomy of most blunt trauma patients, including most adults and older pediatric patients (12,13). Such an imaging is highly sensitive in detecting the presence of CSI as well as the specific form of injury (12). CT imaging may miss fractures of the dens as well as injuries in the plane of the scanner such as dislocations and subluxations, particularly if imaging is completed using early-generation scanners (14). The cross-table lateral radiograph provides a reliable means for detecting these potential missed injuries and, consequently, still plays a role in the initial evaluation of blunt trauma patients undergoing radiographic imaging when reconstructions are inadequate (6,13).
Radiation exposure is an important concern on younger children, and x-ray imaging that includes an anteroposterior (AP), lateral, and open-mouth odontoid still plays an important role in screening this population for injury (13). Plain radiography requires correct exposure and positioning; injury cannot be reliably excluded if images are incomplete or inadequate. Abnormal radiographs should also cause concern, even though no specific injury is evident. Misalignment of spine elements and changes in soft tissue contours may indicate the presence of serious injuries. The interpretation of plain radiographs can be difficult and requires comprehensive knowledge of the subtle findings that may indicate significant injury as well as a detailed understanding of the normal variants that may simulate injury patterns (6). The inexpert interpretation of inadequate cervical spine radiographs is a recipe for disaster. Noncontrast CT imaging is indicated for children with demonstrated cervical spine injuries, and for those who cannot be safely cleared on the basis of x-ray imaging (13).
Imaging, whether CT or x-ray, must be of high quality, with complete visualization of the spine and soft tissues from the base of the skull to the top of the first thoracic vertebra. High technical quality is essential, with proper patient positioning, removal of foreign bodies, and avoidance of motion artifact (6).
Magnetic resonance imaging (MRI) offers an effective and discriminating means for assessing the soft tissues of the cervical spine. Bony injuries are frequently missed on MRI; hence, it is not an adequate substitute for CT or x-ray imaging. MRI is most useful in assessing injuries to the cord, intervertebral disks, and paracervical tissues, including supporting ligaments. Use of this modality should be limited to patients with posttraumatic myelopathy or radiculopathy, patients with pain disproportionate to their physical and radiographic findings, and those with demonstrated occipitoatlantal subluxation, and to assess the acuity of anterior subluxations. MRI and MR angiography may also be valuable in assessing the vertebral arteries, particularly in patients who have pedicolaminar fracture separations (6,13).
Flexion–extension radiographs have been advocated in the acute evaluation of suspected anterior subluxation when plain films are nondiagnostic. However, this type of imaging is known to miss acute anterior subluxations, presumably because of reflex cervical spasm, and has not been shown to enhance the early detection of this initially stable injury (15,16). Consequently, the value of flexion–extension imaging is questionable in the emergency setting and may provide false security to patients with missed injuries. A better approach to the diagnosis and management of patients with suspected anterior subluxation would be to employ MRI to evaluate patients with typical imaging findings or those with neurologic symptoms such as radiculopathy. The remaining patients appear to be best evaluated by delayed flexion–extension imaging once their spasm has resolved (13,15,17).
Motion fluoroscopy has been used to assess spine stability in selected patients, particularly those who cannot cooperate with flexion–extension imaging. Use of this modality, particularly passive fluoroscopy, is controversial because of its potential to produce permanent cord injury. Currently, there are no emergent indications for the use of this imaging (13,18).
KEY TESTING
• Use clinical judgment to initially assess whether a blunt trauma patient is truly at risk of a CSI.
• Apply a decision instrument to determine whether radiologic imaging is indicated.
• High-quality x-ray imaging provides appropriate radiologic evaluation for children and lower-risk young adults.
• CT imaging should be used in assessing high-risk individuals, and older patients.
• MR imaging is inappropriate for most patients. It is inadequate for assessing bone integrity and should be used selectively in assessing vascular and soft tissue structures.









