
Replantation
James L. Larson, Jr
Advances in microsurgery have enabled surgeons to perform replantation procedures on almost all parts of the body. Viability is the only one consideration when evaluating for replantation. The most important factor is the ultimate function of the replantation. Decisions by the emergency physician can significantly impact the viability and function of the replantation.
CLINICAL PRESENTATION
The majority of replantations involve digits injured in industrial accidents (1). Cutting machines, press machines, and belts are the leaders in producing amputations. Significant causes of injury and amputation in children are bicycle chain rings and spokes, including those on stationary exercise bikes (2).
DIFFERENTIAL DIAGNOSIS
An amputated part is a completely severed part of the body, and replantation is the reattachment of an amputated part. An incomplete amputation is partially attached, but the part has lost arterial circulation. The repair of an incomplete amputation is a revascularization. Revascularization is more successful than replantation, because the venous outflow system may be intact.
ED EVALUATION
Identification and treatment of life-threatening injuries takes precedence over the evaluation for potential replantation. A systematic approach to patients with traumatic injuries is necessary to avoid distraction from amputations (see Chapter 18, General Principles of Trauma). Serious undetected concomitant injuries have been found in patients after transfer to a tertiary care facility for replantation (3).
Indications and Contraindications for Replantation
The evaluation of a patient with an amputation or near-amputation should be expeditious. The key considerations are identifying the injuries and the potential for replantation. Amputations that are considered for replantation are listed in Table 47.1. The decision to proceed with replantation is based on potential viability and long-term function. Success rates have been reported to be 66% to 91% for digital replantations (4). A working knowledge of factors that impact success will facilitate patient care and case discussion with the surgeon.
TABLE 47.1
Replantation Candidates
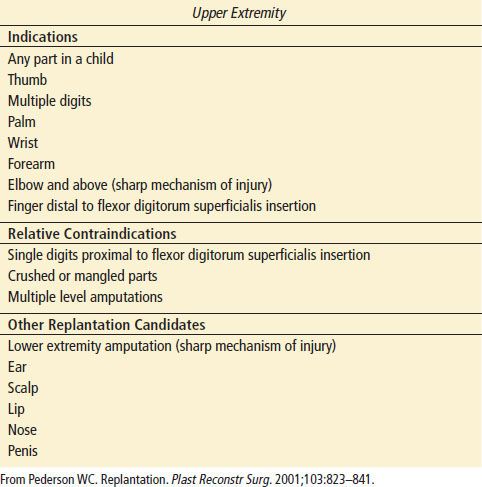
The mechanism of the amputation and resulting condition of the anatomic structures are most significant. Guillotine-like “sharp” amputations are more amenable to surgical repair than crush and avulsion mechanisms. Injuries at one level are easier to replant than multiple insults along an extremity. Children are more likely to have a good result from a replantation, and surgeons are more likely to proceed in pediatric cases (6).
There are several relative contraindications to replantation. Multiply-injured patients who require surgery or prolonged resuscitation for traumatic injuries are not candidates for a prolonged replantation procedure. Patients with complex medical problems that affect vascular integrity, immune function, and healing may be poor candidates for replantation. Patients without sufficient mental capacity or judgment to comply with postoperative rehabilitation are unlikely to have success with replantation (5). Ultimately the decision to proceed with replantation is made by the consulting surgeon. All potential replantation cases, even those with relative contraindications, should be discussed with a replantation surgeon.
KEY TESTING
• Radiographs of the amputation
• Radiographs of the involved extremity
• These should not delay transfer









